Limbic encephalopathy is characterised by the acute or subacute onset of seizures, recent memory loss, confusion and psychiatric symptoms, including anxiety, depression and hallucinations (Reference LishmanLishman, 1998). Current diagnostic criteria take into account neuropathological or neuroradiological evidence of a malignancy, usually testicular cancer, small-cell lung cancer or thymoma (Reference Graus, Delattre and AntoineGraus et al, 2004). However, it is now recognised that in a small proportion of cases this syndrome is not paraneoplastic in nature, but is due to an autoimmune disorder, namely voltage-gated potassium channel (VGKC) antibody-associated encephalopathy (Reference Buckley, Oger and CloverBuckley et al, 2001).
Antibodies to VGKC are known to have central and peripheral effects, and neurological disorders associated with their presence include: neuromyotonia, cramp fasciculation syndrome, Isaacs' syndrome, Morvan's syndrome and limbic encephalitis. These conditions characteristically involve the peripheral neuromuscular system with hyperexcitability and frequent neuromyotonic discharges. Morvan's syndrome additionally involves the autonomic system. Psychiatric symptoms have not been prominent in the 25 cases of VGKC antibody encephalopathy reported to date (Reference Buckley, Oger and CloverBuckley et al, 2001; Reference Thieben, Lennon and BoeveThieben et al, 2004; Reference Pozo-Rosich, Clover and SaizPozo-Rosich et al, 2003; Reference Vincent, Buckley and SchottVincent et al, 2004; Reference Ances, Vitaliani and TaylorAnces et al, 2005). Here we report on a patient who, initially at least, had a predominantly psychiatric presentation which concealed many of the characteristic features associated with the syndrome.
METHOD
A 58-year-old man was referred to the liaison psychiatry department with a 6-week history of episodes that had been diagnosed as psychogenic nonepileptic seizures. During an initial psychiatric assessment, it was noted that the attacks had developed in the setting of moderately severe marital and family stresses and that there was a marked element of anxiety associated with them. A 24 h electroencephalogram (EEG) had been performed and was reported as normal.
Several attacks were witnessed and took the following form. Often in apparent response to questions about emotional topics, he would suddenly appear to become aroused, would flush, breathe heavily, start sweating and make sudden coordinated movements such as trying to take his shirt off, turn round and reach for an object on a shelf, or hold the doctor's hand. Otherwise, the patient was considered to be rather histrionic and was notably indifferent to his attacks. There had been suggestions of odd, child-like behaviour at home, and at times he behaved oddly and inappropriately on the ward, for example being flirtatious and sexually disinhibited. Cognitive state examination was normal and he scored 30/30 on the Mini-Mental State Examination, Reference Folstein, Folstein and McHughFolstein et al, 1975).
There was no previous psychiatric history, no history of alcohol misuse and no family history of mental illness. A history of Huntington's disease in two paternal uncles and the paternal grandmother came to light after admission; however, genetic testing was negative in this case.
The man's condition deteriorated over about 4 weeks. Insomnia, which had been present from an early stage, became marked. At times he appeared to show thought disorder with derailment, tangentiality and numerous word approximations. He also began to express odd ideas (e.g. that the psychiatrist was going to insert wires into his head), and he refused to shake hands because he felt he would pass germs to the psychiatrist which ‘would make him schizophrenic’. Later he believed his partner might have become involved in a paedophile ring and that there were gangs in the hospital selling cocaine. Auditory and visual hallucinations appeared, for example he saw a woman in his bed and heard his partner calling his name. By this time he showed disorientation, mainly at night, and poor recall of recent events. His seizure-like attacks remained frequent, at times occurring every few minutes.
Physical examination was unremarkable except for absent knee and ankle reflexes. Investigations revealed increased inflammatory markers: C-reactive protein 19 mg/l, erythrocyte sedimentation rate 49 mm/h and mildly elevated white blood count. Screening for infections was negative. An autoantibody screen was also negative. Later in the course of the admission the patient developed fluctuating hyponatraemia measuring from 130 to 122 mmol/l. Cerebrospinal fluid analysis revealed mildly elevated protein of 0.65 g/l, with a single band of oligoclonal immunoglobulin which was also present in serum. Nerve conduction studies showed mild demyelination of sensory nerves at axonal levels. Structural magnetic resonance imaging of the brain was normal. A single photon emission computed tomography scan demonstrated hypoperfusion in the frontal, temporal and posterior parietal cortices bilaterally. Whole-body computed tomography, whole-body positron emission tomography and tumour markers indicated no underlying malignancy. Neuropsychological tests revealed moderate impairment on two non-verbal memory tests, Rey figure recall (21st percentile) (Reference Stern, Javorsky and SingerStern et al, 1999) and Warrington Recognition Memory Test (5th-10th percentile) (Reference WarringtonWarrington, 1984). Scores on the three executive tests, the Brixton Test (Reference Burgess and ShalliceBurgess & Shaw, 1997), the Stroop Test (Reference StroopStroop, 1935), and verbal fluency were all in the average or above average range.
RESULTS
About 3 months after the onset of his symptoms, the patient was found to be positive for voltage-gated potassium channel antibodies at >2000 pM (normal <100 pM). A repeat 24 h EEG now showed episodes of frontal sharp-slow complexes consistent with focal seizures probably of frontal origin.
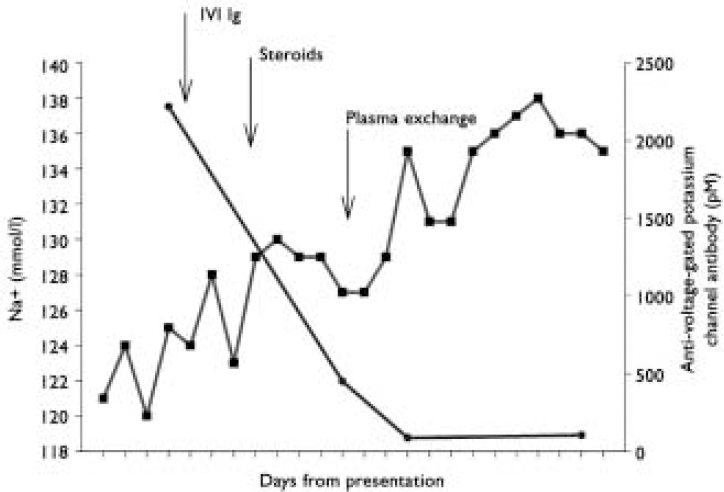
He was treated with intravenous immunoglobulin and steroids, plus phenytoin. This initially resulted in improvement, but it was not sustained. Plasma exchange was therefore commenced and was followed by a dramatic improvement. The seizures stopped; serum sodium levels returned to normal; and antibody titres progressively decreased (Fig. 1). His psychotic symptoms abated but then returned transiently, possibly related to steroid treatment; they responded well to low-dose neuroleptic treatment. He was discharged from hospital and has remained well without psychotropic medication. His non-verbal memory test scores have improved.

Fig. 1 Serum sodium levels and antibody (VGKC-Ab) titres in relation to
different treatments. ![]() VGKC
Ab;
VGKC
Ab; ![]() serum
sodium level.
serum
sodium level.
DISCUSSION
In the 25 cases of VGKC antibody-associated encephalopathy reported to date, the main symptoms have been memory loss and seizures (usually of temporal lobe type). Agitation and insomnia have been described in a majority of cases, plus hallucinations in three cases and depression and delusions in one case (Reference Vincent, Buckley and SchottVincent et al, 2004). In the case reported here, however, psychiatric symptoms were to the forefront of the clinical picture. The exact syndromal diagnosis remains open to debate, but is probably best understood as a state resembling organic schizophrenia, giving way to delirium.
This case illustrates how easy it is to mistake frontal lobe seizures for psychogenic non-epileptic seizures. Frontal lobe seizures (Reference Kellinghaus and LudersKellinghaus & Luders, 2004) are typically brief, lasting less than a minute, and may present with organised and semipurposeful movements, including thrashing of the limbs, rocking and bicycling, and also laughing and shouting. Fear and other ictal emotions may be present. These features are often so striking that further ictal manifestations may be overlooked, such as lapse of consciousness, conjugate eye deviation, head turning or clonic movements. Abnormalities on EEG may not be present, even during an attack, because of the difficulty in detection of mesial or basal foci.
In the case reported here the diagnosis of limbic VGKC antibody-associated encephalopathy was made only after protracted investigation and several false leads. This disorder needs to be added to the long list of differential diagnoses in cases presenting atypical psychiatric pictures with organic features (Reference Butler and ZemanButler & Zeman, 2005), and it is an important diagnosis to make because, as this patient's case reveals, it is eminently treatable.



eLetters
No eLetters have been published for this article.