Primary care practices are busy places. Clinicians and staff are challenged to address an individual patient’s reason for visit, reconcile medications, manage chronic conditions, advocate prevention, review and respond to lab reports, consults, email, and telephone queries [Reference Baron1]. Although researchers determined two decades ago that a lack of time rendered primary care delivery of United States Preventive Services Task Force (USPSTF) A and B graded recommendations impracticable [Reference Yarnall2], expectations connected to patient-centered medical home transformation, and triple or quadruple aim goals continue to increase time burdens. Time-constrained primary care practices will be further challenged by translational science goals involving discovery and development of learning healthcare system capabilities for implementing new therapies. So what do we know about the time it currently takes primary care practices to introduce new knowledge into practice? This brief report begins to address the lack of systematic inquiry by providing preliminary data about the pace of adoption or time to adoption of a USPSTF guideline into the primary care setting.
Study Context
The Ask About Aspirin study employed a two-arm group randomized design to implement the USPSTF guideline for the use of aspirin for primary prevention of cardiovascular events within primary care practices. In addition to changes in clinical practice, this study included a public health information campaign to motivate individuals to talk with their doctor. Phone survey data form the primary approach to assessing changes in aspirin use. The potential for contamination in densely populated areas and the absence of comparators led to the exclusion of clinical practices in the Metropolitan Minneapolis-St. Paul and Rochester areas. The rest of Minnesota was divided into 24 geographic and population units with healthcare systems and primary care practice groups in 12 units invited to participate during the initial two years. The remaining 12 units would be engaged over two subsequent years. Eight health care organizations with 55 primary care clinics and a combined staff of ≈380 clinicians and ≈620 nursing and support staff opted to participate and partner in this study during the first two years. Alternatively, 8 health care organizations with 28 total clinics declined to participate; reasons for refusal included lack of time or competing projects (often Information Technology (IT) related). In addition, a few systems declined to participate because randomization would differentiate practice within a subset of clinics. However, the randomization scheme did not pose a barrier for every system. Addressing randomization by testing a process within a limited number of sites and, if successful, disseminating it throughout an organization is recognized as a “stage implementation scale up” implementation strategy [Reference Powell3]. In this case, dissemination within systems would occur when the clinics in the remaining 12 geographical units joined the project. This study of practice facilitation support for improving aspirin prescriptive behaviors within primary care was described at the proposal stage as a pragmatic clinical trial.
All participating healthcare systems and practice groups signed a memorandum of understanding (MOU). The University of Minnesota Institutional Review Board approved and provided ethical oversight.
Implementation Strategy
The study implementation strategy utilized practice facilitators (PFs). Practice facilitation goals included supporting operationalization of the USPSTF recommendations through organization and clinic staff development and implementation of a workflow [Reference Pinnock4] or health intervention [Reference Proctor5]. Using facilitation to support staff was projected to increase the likelihood that changes in care delivery would be appropriate, feasible, adoptable within clinical practice, and acceptable to patients, because they were designed by people familiar with ongoing care practices and patient panels. In addition, routinizing care delivery through implementation of a shared workflow was expected to contribute to sustainability. The PFs utilized skills honed in formal training at a local Practice Facilitation course. This training included methods of clinic interaction such as motivational interviewing, appreciative inquiry, and relationship building. During the study, the PFs also encouraged performance improvement by bringing a Plan-Do-Study-Act mentality to the analysis of monthly and then quarterly reports. In this way, the implementation strategy focused on the quality of workflow adherence or fidelity as an implementation outcome [Reference Proctor5].
Two PFs and a co-investigator began to prepare the implementation strategy by reviewing the research proposal, the 2009 and then 2016 USPSTF aspirin use for primary prevention recommendations [6,Reference Bibbins-Domingo7], and research about primary care transformation [Reference McNellis, Genevro and Meyers8–Reference Nutting11]. The group created a standardized onboarding process with milestones to monitor partner progress (Table 1). The onboarding process contained a detailed description of the following USPSTF recommendations: (1) Identify the primary aspirin candidates from the general patient population by age and by using a cardiovascular disease (CVD) risk assessment calculator to determine patients with a CVD risk score of 10% or above over 10 years. (2) Educate the patient regarding the use of low-dose aspirin for primary prevention. (3) Document the outcomes of discussions between the primary care provider and the patient as (a) aspirin recommended, (b) aspirin contraindicated, or (c) patient refused to take aspirin. The onboarding process was essential because many organizational leaders who decided to participate tasked their staff with executing this project.
Table 1. Practice facilitator standardized onboarding approach: activity and purpose

USPSTF, United States Preventive Services Task Force; PF, practice facilitator.
The PFs worked in pairs and split participant and observer responsibilities. One PF had responsibility for managing interactions with a project team throughout the workflow development process. The second PF observed and kept notes on planning process interactions during conference calls, onsite meetings, and through email. Consistent documentation of observations was achieved through regular discussion among the PFs. PF discussions to finalize observations of project team progress doubled as assessment and planning meetings. Documented observations included dates used to assess partner progress through the project milestones.
The PFs considered each project team to represent a “complex adaptive system [Reference Berwick and Fox12,Reference Litaker13].” They assumed system and practice variation. They accepted responsibility for supporting individual project team development of an approach to incorporating aspirin guideline recommendations into their practice sites. As an implementation strategy, practice facilitation combines the Expert Recommendations for Implementing Change strategies of facilitation or interactive problem solving through ongoing consultation and implementation advice [Reference Powell3].
Results
This study observed practice facilitation support for workflow planning within primary care across multiple systems to learn about the average time it took to adopt a guideline and change clinical practice. While this project did not originate within organizational planning processes, which likely influences preparation time, having to accommodate new initiatives in real time helps establish a baseline and shape expectations regarding pace of adoption within primary care. Results are organized according to implementation outcomes [Reference Proctor5]. However, a PF implementation strategy brings intentionality or awareness of outcomes into the workflow planning process, assessment and success of planning can only be determined post adoption.
Adoption
The PF implementation strategy resulted in all eight partners, successfully developing and adopting a workflow to identify patients with an appropriate cardiovascular risk profile and to facilitate a clinician–patient discussion about taking low-dose aspirin daily for primary prevention. From signed MOU to adoption of the workflow in clinical practice across all sites required an average of 252 days [Reference Knierim14]. Progress through each milestone varied across project partners. For example, three project teams started working with the PFs an average of 43 days before returning a signed MOU; this is calculated as a negative number in the project milestone visualization (Fig. 1); the immediate action decreased the overall average pace of adoption by 21 days (8%) and suggests inefficiency with project-by-project agreements.

Fig. 1. Time to guideline adoption across all primary care practices. (a) Average time to adoption across all sites, (b) Average time across all sites through PF onboarding milestones, and (c) Implementation strategy and outcomes addressed. MOU, memorandum of understanding; PF, practice facilitator.
The project teams varied in their access to resources. For example, accessing IT expertise to create and refine electronic records, alerts and reports, often had extended delivery deadlines that contributed to delay. However, one team with direct involvement from a system leader developed and adopted their workflow in the fewest number of days. Systems with established quality improvement teams required less time to begin planning a workflow.
Appropriateness
The PFs accommodated variation across systems and practices. Variation was first encountered among the eight project teams, which averaged 3.4 persons (range 1–9 persons). Each team designated a leader who served as the liaison between the PF, the project team and its system and practices. Some team leads worked at the system or organizational level, while others were managers in one or more clinical practices. Project team interactions with the PFs averaged 2.25 on-site meetings (range 1–5), 8.3 conference calls (range 2–20), and 23.5 emails (range 9–37).
The PFs demonstrated flexibility by encouraging project teams to align the development of a workflow with existing practices and policies; this resulted in a variety of workflows. For example, identification of aspirin candidates occurred during pre-visit planning, during rooming by accessing a dot-phrase screen within the medical record, or by having an alert fire when clinicians accessed a patient’s medical record. One clinician alert identified patient aspirin candidates or indicated when data was needed to complete the assessment and determine patient risk. Project teams expressed appreciation for PF support and flexibility about workflow planning, for the posters and patient and provider education materials made available at no cost, and for the opportunity to align the project with health system practices and priorities.
Acceptability
The practice workflows described in Table 2 can be organized into two general strategies. One strategy localized within the patient–practitioner encounter, and a second strategy incorporated into the multiple interactions between care team members and patient. These two approaches were previously observed in relation to guideline implementation [Reference Hysong, Best and Pugh15]. Given our understanding of complex adaptive systems and practice variation, it is not possible to identify the most effective implementation strategy.
Table 2. Site workflows developed for primary care adoption by project teams
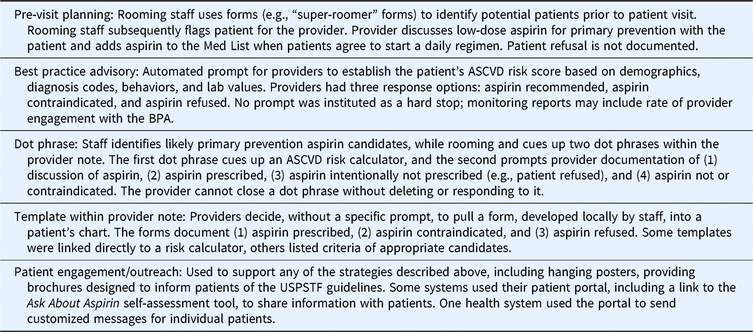
BPA, best practice advisory; ASCVD, atherosclerotic cardiovascular disease; USPSTF, United States Preventive Services Task Force.
Feasibility
The Ask About Aspirin project was designed as a group randomized trial, organizing comparable populations into matched geographic territories and working with primary care practices within those territories. The NIH reports that PubMed abstracts about “Group- or Cluster-Randomized Trials for human studies has more than doubled every five years since 1995 [16].” While some system partners accommodated a staged implementation with minimal resistance, ongoing consolidation of primary care practices into larger healthcare systems may complicate future use of trial designs that randomize by practice.
Cost
To avoid drawing attention to the pace of work, the PFs did not collect information about staff time or resources devoted by practices to this project. However, refining our understanding of implementation outcomes will advance our ability to hone economic projections about primary care guideline adoption costs that are essential to the learning healthcare system’s ability to change practice, improve outcomes, and reduce overall costs [Reference Shiell, Hawe and Gold17].
Financial challenges in primary care were discussed in two Agency for Healthcare Research and Quality EvidenceNOW project commentaries: Bitton observed that the extension agent (or PF) approach “if supported financially, is one promising approach [Reference Bitton18].” However, Casalino suggested that free external support may not ensure that “practices will supply free labor to transform [Reference Casalino19].” Being able to estimate the pace of adoption marks an important step in organizing cost data on knowledge translation.
Limitations
This study examined the pace of practice adoption of a USPSTF guideline as the primary implementation outcome. As a result, this study could not ascertain how this deployment of a practice facilitation implementation strategy addressed the implementation outcomes of workflow sustainability, penetration or fidelity.
We began by recognizing that primary care practices are busy places. While encouraging efficiencies in implementation, we also recognize that change produces intended and unintended consequences. Time to adoption must provide practices time to examine safety and ethical issues.
The challenge of determining the unit of analysis, in this case system or individual practice, complicated assessing readiness for change. In addition, this study did not attempt to identify competing system or practice change projects in order to avoid drawing attention to the pace of adoption.
Conclusion
Motivated by systems’ thinking and a preoccupation with context for understanding how adoption takes place [Reference Green and Seifert20], this project studied the adoption of USPSTF guidelines into primary care clinical practices with a support from PFs. Observations about guideline implementation planning and the pace of adoption should encourage clinician and researcher sensitivity to the pace of change within primary care practices and to achieving translational efficiencies within learning healthcare systems.
This Ask About Aspirin report combined observations across multiple partners. Every partner who agreed to participate successfully launched an implementation strategy, confirming practice facilitation as a reliable support for practice transformation amidst competing system and practice priorities. Study observations of busy practices indicate that planning to implement the USPSTF aspirin for primary prevention guideline required about two-thirds of one year.
Acknowledgements
The authors acknowledge the work of four University of Minnesota colleagues: Dr. Kevin Peterson (Professor, Department of Family Medicine and Community Health), Dr. John Finnegan (Dean, School of Public Health) and the late Dr. Alan T. Hirsch (Professor, Medicine, Epidemiology and Community Health) contributed to the design and implementation of the Ask About Aspirin campaign; Dr. Niki Oldenberg and Dr. Jeremy Van’t Hof (Cardiovascular Division, University of Minnesota Medical School) reviewed and commented on earlier manuscripts.
This work was supported in part through grant R01HL126041 from the National Heart, Lung, and Blood Institute at the NIH and the Clinical and Translation Science Institute grant UL1 TR002494 from the National Center for Advancing Translational Science. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
The authors declare that they have no competing interests.





