Childhood trauma has been associated with first-episode psychosis, Reference Fisher, Jones, Fearon, Craig, Dazzan and Morgan1,Reference Mondelli, Dazzan, Hepgul, Di Forti, Aas and D'Albenzio2 affective dysfunction, Reference Nanni, Uher and Danese3–Reference Upthegrove, Chard, Jones, Gordon-Smith, Forty and Jones6 and substance use. Reference Madruga, Laranjeira, Caetano, Ribeiro, Zaleski and Pinsky7–Reference Konings, Stefanis, Kuepper, de Graaf, ten Have and van Os9 In a recent case-control study patients with first-episode psychosis showed a prevalence of physical abuse of 14–15% and a prevalence of sexual abuse of 18%. Reference Fisher, Jones, Fearon, Craig, Dazzan and Morgan1 In a similar sample two-fold higher rates of childhood trauma were reported in cases compared with controls. Reference Mondelli, Dazzan, Hepgul, Di Forti, Aas and D'Albenzio2 Exposure to childhood trauma was found to be associated with a two-fold risk of both recurrent and persistent depression; Reference Nanni, Uher and Danese3 it predicts lifetime suicide attempts in patients with treatment-resistant depression (OR = 2.79, 95% CI 1.14–6.84), Reference Tunnard, Rane, Wooderson, Markopoulou, Poon and Fekadu4 and has been related to the presence of psychotic features in mood disorders. Reference Gaudiano and Zimmerman5 Finally, childhood trauma has been associated with a higher risk of substance use in adolescence and early adulthood in the general population (OR = 3.83, 95% CI 1.29–11.30), Reference Madruga, Laranjeira, Caetano, Ribeiro, Zaleski and Pinsky7 and may also have a role in modulating and moderating the association between cannabis use and the later development of psychosis. Reference Houston, Murphy, Shevlin and Adamso8 The risk of psychosis is higher in those who have been exposed to both childhood trauma and cannabis use compared with those exposed to only one of the two. The strength of this association was found to be dose-dependent, with higher rates of psychosis occurring as the frequency and severity of traumatic experiences increased. Reference Konings, Stefanis, Kuepper, de Graaf, ten Have and van Os9 We therefore aimed to verify, in a large, epidemiologically representative sample of people with first-episode psychosis, whether people who had experienced childhood trauma (when compared with those who had not) showed a psychosis onset characterised by a higher rate of affective psychosis, and second, had an increased lifetime rate of substance use.
Method
This study was conducted within the framework of the Genetics Endophenotypes and Treatment: Understanding early Psychosis – Psychosis early Intervention and Assessment of Needs and Outcome (GET UP PIANO) trial. This is a large, multicentre, randomised controlled trial comparing an add-on multi-element psychosocial early intervention with routine care for people affected by first-episode psychosis and their relatives, provided within Italian public mental health services. Detailed information on the study design, sample recruitment and clinical assessment has been reported elsewhere. Reference Ruggeri, Bonetto, Lasalvia, De Girolamo, Fioritti and Rucci10 The trial was proposed to all community mental health centres (CMHCs) located across two northern Italian regions (Veneto and Emilia-Romagna) and the urban areas of Florence, Milan and Bolzano, covering an area with 9 951 306 inhabitants. Reference Ruggeri, Bonetto, Lasalvia, Fioritti, de Girolamo and Santonastaso11 Of 126 CMHCs, 117 (93%, covering 9 304 093 inhabitants) participated. The trial was approved by the ethics committees of the coordinating centre (Azienda Ospedaliera Universitaria Integrata di Verona) and each participating unit, and was registered with ClinicalTrials.gov (NCT01436331).
Participants
All CMHC professionals were asked to refer potential psychosis cases at first contact during the index period (1 April 2010 to 31 March 2011) to the study team. Immediately thereafter, a screening questionnaire for psychosis was administered. Reference Jablensky, Sartorius, Ernberg, Anker, Korten and Cooper12 The inclusion criteria were:
-
(a) age 18–54 years;
-
(b) residence within the catchment areas of CMHCs;
-
(c) presence of at least one of the following symptoms: hallucinations, delusions, qualitative speech disorder, qualitative psychomotor disorder or bizarre or grossly inappropriate behaviour; or two of the following symptoms: loss of interest, initiative and drive; social withdrawal; episodic severe excitement; purposeless destructiveness; overwhelming fear or marked self-neglect;
-
(d) first lifetime contact with CMHCs, prompted by these symptoms.
Exclusion criteria were antipsychotic medication (>3 months) prescribed for an identical or similar mental disorder; mental disorders due to a general medical condition; moderate to severe mental retardation assessed by clinical functional assessment; and psychiatric diagnosis other than ICD-10 for psychosis. Since a first psychotic episode is generally a phase of high diagnostic instability, the specific ICD-10 codes for psychosis (Flx.4; Flx.5; Flx.7; F20–29; F30.2, F31.2, F31.5, F31.6, F32.3, F33.3) were assigned at 9 months. The best-estimate ICD-10 diagnoses were made by consensus by a panel of clinicians by taking into account all available information gathered in the 9-month follow-up period, as required to apply the Item Group Checklist of the Schedule for Clinical Assessment in Neuropsychiatry (SCAN). Reference Wing, Babor, Brugha, Burke, Cooper and Giel13 Eligible patients, identified as those who were sufficiently clinically stable, gave written informed consent. Reference Ruggeri, Bonetto, Lasalvia, Fioritti, de Girolamo and Santonastaso11
Assessment
Participants were assessed by a team of 17 independent researchers who underwent specific training on the use of the standardised instruments and an interrater reliability exercise to determine consistency of evaluations between investigators. Information about childhood trauma and substance use was collected using the Childhood Experience of Care and Abuse – Questionnaire (CECA-Q) and the Cannabis Experiences Questionnaire respectively. Reference Bifulco, Bernazzani, Moran and Jacobs14,Reference Barkus, Stirling, Hopkins and Lewis15 Severe sexual abuse has been defined as an experience that:
had to meet at least two of the following criteria: the perpetrator was known to the individual; the perpetrator was a relative; the perpetrator lived in the same household; the unwanted sexual experience occurred more than once; the perpetrator touched the child's genitals; the perpetrator forced the child to touch the perpetrator's genitals; the abuse involved sexual intercourse. Reference Aas, Navari, Gibbs, Mondelli, Fisher and Morgan16
Severe physical abuse has been defined as a repeated exposure to physical violence from parental figures before age 16:
that had to meet at least two of the following criteria: the abuse consisted of being hit with a belt or stick or being punched or kicked; the abuse resulted in an injury, including broken limbs, black eyes or bruising; the perpetrator was considered to be out of control. Reference Aas, Navari, Gibbs, Mondelli, Fisher and Morgan16
Separation has been defined as a detachment from at least one living relative longer than 6 months within the first 17 years of life; loss was defined as the death of one or both parents during the participant's childhood. Participants were defined as ‘traumatised’ if they had experienced at least one trauma: severe sexual abuse, severe physical abuse, separation, and/or loss. Lifetime substance use, including several types of drugs, was assessed using the Cannabis Experiences Questionnaire. Reference Barkus, Stirling, Hopkins and Lewis15 The sample was stratified into two groups: those who had never used substances and those who had used substances at least once in their life.
Statistical analysis
The association between categorical variables was evaluated by chi-squared or Fisher's exact test, where appropriate. Adjustment for gender was performed in univariate logistic regression models, with specific types of traumas as dependent variables and diagnosis and substance misuse as independent variables. Interaction between gender and trauma was controlled for in all models. All tests were bilateral at P < 0.05. Analyses were performed using SPSS version 22.0 for Windows.
Results
Description of the sample
Within the GET UP PIANO trial, 444 patients identified at intake with a confirmed ICD-10 diagnosis of psychosis at 9 months were assessed. Of these, 345 (78%) individuals (58% male, mean age 29.8 years, s.d. = 9.7) agreed to be interviewed about their childhood traumatic experiences and represented the sample of this study. No significant difference was found with regard to sociodemographic or clinical characteristics between participants who completed the CECA-Q and those who did not (data available from the authors), with the exception of non-Italian nationality, which was more frequent among those who did not complete the questionnaire (P = 0.01). Among the 345 persons who completed the CECA-Q, 80 (23%) received an ICD-10 code for affective psychoses, whereas 265 (77%) received an ICD-10 code for non-affective psychoses (schizophrenia n = 96, 28%; non-affective, non-schizophrenic psychosis n = 169, 49%). Regarding childhood trauma, of the 345 people with first-episode psychosis 8% experienced severe sexual abuse during their childhood, 14% reported severe physical abuse and 20% were separated for more than 6 months from at least one of the parental figures and/or lost one of their parents. Overall, 37% had had at least one traumatic experience during their childhood. In terms of lifetime substance use, 43% of the 345 participants reported cannabis use, 20% recalled cocaine use and 6% reported heroin use. When looking at combined lifetime use we found, as expected, that all participants (100%) who reported a lifetime use of heroin had both cocaine and cannabis lifetime use. Similarly, those who reported a lifetime use of cocaine also had a lifetime cannabis use in 96% of cases. Finally, among those with a cannabis lifetime use, 52% reported an exclusive use of cannabis.
Sociodemographic features and clinical characteristics of the sample are shown in Table 1.
Table 1 Sociodemographic profile of the sample (n = 345)
| Sociodemographic factor | n (%) |
|---|---|
| Gender, male: n (%) | 199 (57.7) |
| Age at first contact with services, years: mean (s.d.) | 29.8 (9.7) |
| Educational level, n (%) a | |
| Low (primary-middle school) | 125 (37.2) |
| High (secondary school, university) | 211 (62.8) |
| Marital status, n (%) b | |
| Single | 251 (75.4) |
| In a relationship/married | 62 (18.6) |
| Widowed/separated/divorced | 20 (6.0) |
| Working status, n (%) a | |
| Unemployed | 107 (31.8) |
| Employed | 126 (37.5) |
| Student/homemaker/retired | 103 (30.7) |
| Nationality, n (%) c | |
| Italian | 311 (91.2) |
| Other | 30 (8.8) |
a. Data missing for 9 participants.
b. Data missing for 12 participants.
c. Data missing for 4 participants.
Childhood trauma and diagnosis
The overall rate of affective psychosis detected in traumatised and non-traumatised participants was around 24% in both groups (Fig. 1). Analysing the specific types of traumas, we found a significant association between severe childhood sexual abuse and affective psychosis (χ2 = 4.9, P = 0.04). In particular, 42% of those who reported severe sexual abuse had an affective psychosis compared with 22% of the non-sexually abused group; this finding remained significant after adjusting for gender (OR = 2.2, 95% CI 1.1–6.2; P = 0.03). The interaction between gender and trauma was not significant. In contrast, the percentage of affective psychosis was lower in participants with severe physical abuse than in those without it (16% v. 24%; P = 0.25), although this difference was not significant. Moreover, no significant difference was found in terms of diagnosis between participants with a history of separation or loss of parents and those without such a history (22% v. 24%; P = 0.85).
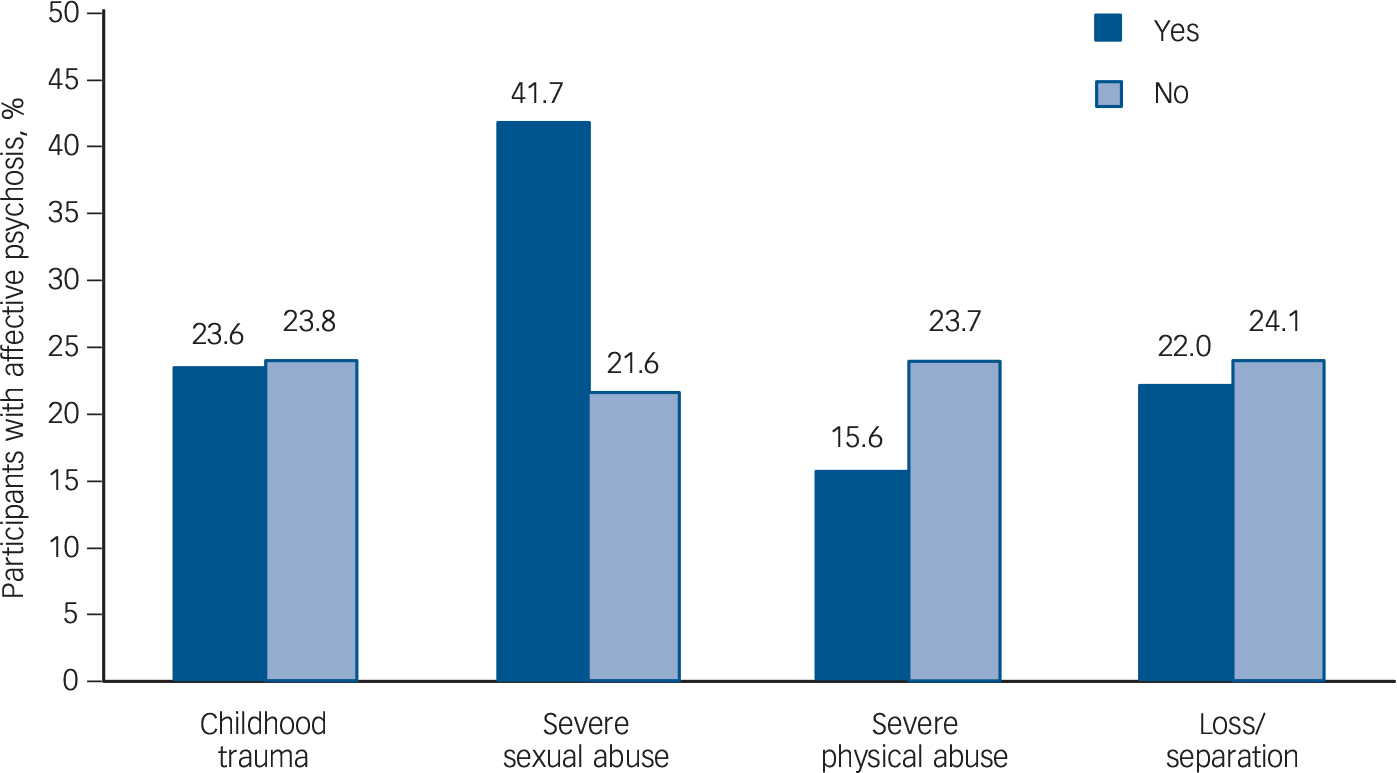
Fig. 1 Association between childhood traumatic experiences and diagnosis. The association for severe sexual abuse was significant at P = 0.04.
Childhood trauma and substance use
Overall, severely abused individuals showed a significantly higher frequency of lifetime substance use (cannabis, cocaine or heroin) than non-abused individuals (60% v. 39%; P = 0.008).
Cannabis
About half (54%) of the participants with traumatic experiences during childhood reported lifetime cannabis use compared with 34% of those without traumatic experiences (P = 0.013) (Fig. 2). In particular, cannabis use was significantly more frequent among those reporting severe sexual abuse compared with those who did not report such abuse (68% v. 41% respectively; P = 0.023). This finding remained significant after adjusting for gender (OR = 4.6, 95% CI 1.7–12.5; P = 0.003). The interaction between gender and trauma was not significant. In contrast, no significant association was found between severe physical abuse or loss/separation and lifetime cannabis use.
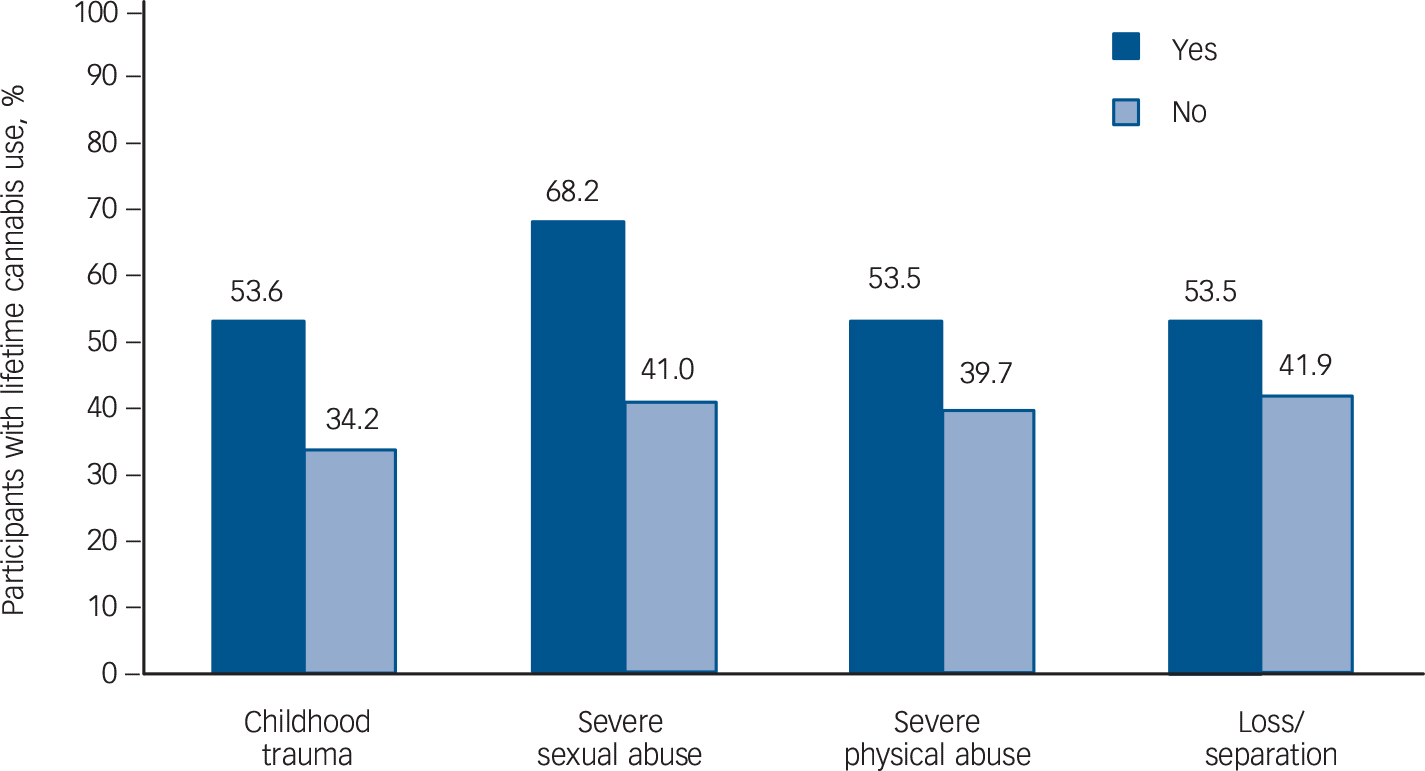
Fig. 2 Association between childhood traumatic experiences and lifetime cannabis use. The association for trauma was significant at P = 0.013 and for severe sexual abuse at P = 0.023.
Heroin
No significant difference in lifetime use was found between traumatised and non-traumatised individuals in terms of heroin use (6% v. 5%; P = 0.74). However, severely sexually abused participants reported significantly higher lifetime heroin use compared with non-sexually abused participants (20% v. 5%; P = 0.02). This finding remained significant after adjusting for gender (OR = 12.6, 95% CI 2.7–58.1; P = 0.001). Similarly, physically abused individuals reported substantially more heroin lifetime use when compared with those who had not been physically abused (15% v. 5%; P = 0.03). This finding remained significant after adjusting for gender (OR = 3.7, 95% CI 1.2–11.3; P = 0.02). The interaction between gender and trauma was not significant. In contrast, no significant association was found between loss/separation and lifetime heroin use (8% in exposed v. 6% in non-exposed groups; P = 0.71).
Cocaine
No significant difference in lifetime cocaine use (23% v. 16%; P = 0.30) was found between traumatised and non-traumatised participants. In particular, no significant association was found between severe sexual abuse or loss/separation and lifetime use of cocaine. Conversely, severely physically abused participants showed higher lifetime cocaine use in comparison with non-physically abused patients (32% v. 17%; P = 0.05). This finding gained significance after adjusting for gender (OR = 2.3, 95% CI 1.1–4.9; P = 0.04). The interaction between gender and trauma was not significant.
Discussion
This is the first study to investigate the relationship between childhood trauma and affective psychosis in a large sample with first-episode psychosis recruited in a ‘real world’ setting. As predicted, we found a significant association between affective psychosis and severe sexual abuse and between drug misuse and both severe sexual and severe physical abuse. We found the frequency of sexual and physical abuse to be substantially lower than in previous studies of first-episode psychosis. Reference Fisher, Jones, Fearon, Craig, Dazzan and Morgan1,Reference Neria, Bromet and Sievers17 In fact, severe sexual abuse was reported in 8% of our sample v. 15–18% in previous studies; similarly, severe physical abuse was reported in 14% v. 15–22%. Reference Fisher, Jones, Fearon, Craig, Dazzan and Morgan1,Reference Neria, Bromet and Sievers17 Variability in the prevalence of abuse has been widely described before. Methodological issues such as heterogeneity of definition, sample size and demographic and social context issues have been identified as possible reasons for this variability. Reference Fisher, Craig, Morgan, McKenzie and Fearon18 The use of a ‘severe’ abuse category, instead of the ‘abuse’ one, might account for differences with other studies. Rates of sexual and physical abuse in our sample were 11% and 29% respectively. Regarding sexual abuse, our rate remains substantially lower than that found by others; Reference Fisher, Jones, Fearon, Craig, Dazzan and Morgan1,Reference Neria, Bromet and Sievers17 however, the prevalence of physical abuse is broadly in line with other research. The surge in the rate of physical abuse in our sample might depend on the inclusion in this category of physical punishments (i.e. open-handed smacks) and maltreatments (such as punches and kicks), even when occurring once in a lifetime. The social acceptability of corporal punishments as a method of education and their consequent high frequency within Italian families might therefore explain the data. Overall, the lower percentage of abused participants in our sample is consistent with a survey carried out in the Italian general population, in which 8 children out of 1000 were reported to be victims of maltreatments; specifically, among minors under the care of child services, 4% were sexually abused whereas 7% experienced physical maltreatment. Reference Bollini, Giannotta and Angeli19 When compared with rates from the World Health Organization (WHO) Global Status Violence Prevention, a discrepancy comes to light with Italian rates, which are substantially lower than rates in other high-income countries. 20 In the USA the prevalence rates of sexual abuse and physical maltreatment were 7% and 10% respectively; in Canada the respective rates were 7% and 23%, and in Australia 10% and 28%. These differences might be due to a more cohesive family and an enhanced social support network, which are common in southern European countries, Reference Bertani, Lasalvia, Bonetto, Tosato, Cristofalo and Bissoli21 or it could reflect the proneness to silence, connected with the feelings of shame and stigma, related to the experience of trauma. Reference Taylor22 Nonetheless, comparing trauma rates in our sample (sexual abuse 11%, physical abuse 29%) with those of the Italian general population (sexual abuse 4%, physical abuse 7%), the results confirm at least a two-fold increase and are consistent with findings shown previously. Reference Mondelli, Dazzan, Hepgul, Di Forti, Aas and D'Albenzio2
Affective psychosis and childhood trauma
In our study severely sexually abused people with first-episode psychosis had a five-fold higher likelihood of receiving a diagnosis of affective psychosis. Our results are in line with previous studies, which showed an increased presence of psychotic features in both major depressive disorder and bipolar affective disorder when the person had been abused. Reference Gaudiano and Zimmerman5,Reference Upthegrove, Chard, Jones, Gordon-Smith, Forty and Jones6,Reference Hammersley, Dias, Todd, Bowen-Jones, Reilly and Bentall23 Affective symptoms could mediate the victimisation-psychosis association. Our data are consistent with previous studies, Reference Garety, Bebbington, Fowler, Freeman and Kuipers24,Reference Gracie, Freeman, Green, Garety, Kuipers and Hardy25 which advocate a significant role of negative beliefs about self and others and of depression and anxiety within the pathway from early trauma to psychosis. Most interestingly, only sexual abuse – not physical abuse – has been proved to be a strong and specific risk factor for mental disorders, including major depression and anxiety disorder, Reference Fergusson, McLeod and Horwood26 once more supporting our results. A recent study described a significant association between sexual abuse and depressive symptoms in women but not in men, suggesting that maltreatments may have a gender effect on the development of maladaptive self-images and depression, Reference Haug, Oie, Andreassen, Bratlien, Nelson and Aas27 mediated by a gender difference in stress reactivity. Women have been shown to be more susceptible to the negative consequences of stress in general, Reference Myin-Germeys, Krabbendam, Delespaul and Van Os28 and of early traumatic experiences in particular. Reference Myin-Germeys and Van Os29 In contrast, we did not find any effect of gender on the association between severe sexual abuse and affective psychosis. Our study did not investigate the presence of depressive symptoms but focused on diagnostic category; issues other than gender might therefore be involved and explain the discrepancy with previous evidence.
Substance use and childhood trauma
In our sample, drug use was found to be associated with both severe sexual and severe physical abuse. Traumatised participants – in particular, those reporting severe childhood sexual abuse – showed significantly higher lifetime cannabis use. The trauma-cannabis-psychosis association could involve several psychosocial elements, contributing to an enhanced vulnerability, Reference Houston, Murphy, Shevlin and Adamso8 and various biological factors, including the dopamine neurotransmitter system, Reference Kaufman, Plotsky, Nemeroff and Charney30 and the hypothalamic-pituitary-adrenal (HPA) axis. Reference Mondelli, Dazzan, Hepgul, Di Forti, Aas and D'Albenzio2 First, childhood trauma has been significantly associated with depression, which usually precedes the onset of substance dependence among traumatised people. Reference Douglas, Chan, Gelernter, Arias, Anton and Weiss31 Consistent with this, abused individuals in our sample more frequently received a diagnosis of affective psychosis when compared with those who were not abused. We may therefore propose the role of affective symptoms as mediators or modulators of the trauma-cannabis-psychosis association. Abused people tend to become more frequently depressed and thus might more frequently use cannabis to alleviate depressive symptoms, or could develop dysfunctional coping strategies such as self-medication to reduce trauma-related stress. Reference Houston, Murphy, Shevlin and Adamso8 Second, social factors might have a meaningful influence: disadvantaged environments, where it is easier to become entrapped in substance dependence, and social adversities, such as a low socioeconomic status and unemployment, have been shown to be significantly associated with both psychosis and childhood trauma. Reference Wicks, Hjern, Gunnell, Lewis and Dalman32 Finally, it is a reasonable hypothesis that abused and non-abused individuals have similar drug use patterns but that only the former develop psychosis owing to their pre-existing enhanced vulnerability. Reference Houston, Murphy, Shevlin and Adamso8,Reference Tosato, Lasalvia, Bonetto, Mazzoncini, Cristofalo and De Santi33
Biological factors may also be involved. First, and in line with the ‘sensitisation’ hypothesis, genetically predisposed individuals, whether exposed to environmental risk factors (as childhood trauma and cannabis use) or not, have been proved to show an increased dopaminergic response to social stressors. It may lead to stable changes in the stress-related dopaminergic response system, Reference Collip, Myin-Germeys and Van Os34 and eventually to a subsequent enhanced vulnerability for psychosis. Second, animal studies have shown an influence of environmental stressors on a rat's delta-tetrahydrocannabinol (ΔTHC) response: Reference Suplita, Eisenstein, Neely, Moise and Hohmann35 under stressful housing conditions (i.e. isolation and food deprivation) ΔTHC administration resulted in an increased dopamine uptake and significant behavioural abnormalities not observed in control group rats. Reference MacLean and Littleton36 Finally, early traumatic experiences have been associated with permanent HPA axis overreactivity (higher levels of Cortisol) to stressors and changes in brain structures. Reference Read, Perry, Moskowitz and Connolly37 Moreover, we found that both sexual and physical severe abuse experiences were significantly associated with heroin lifetime use, whereas cocaine lifetime use appeared to be associated only with severe physical abuse, which is to some degree in line with results for other psychiatric disorders (anxiety, mood and borderline personality disorders). Reference Banducci, Hoffman, Lejuez and Koenen38 Our findings seem to contrast with a recent study that found no association between childhood trauma and use of cannabis or other illicit drugs. Reference Duhig, Patterson, Connell, Foley, Capra and Dark39 This inconsistency might be partially explained by the different time frame used when investigating substance use: we explored lifetime use, whereas the other study investigated substance use in the preceding month.
Strengths and limitations
The GET UP PIANO trial is the first trial in first-episode psychosis patients performed in a large catchment area, corresponding to nearly 10 million inhabitants. Over 90% of CMHCs completed the study, demonstrating that the participants were highly representative of the patients treated in the community psychiatric services. We used reliable, internationally validated instruments and adopted conservative cut-off points, previously applied, to identify only the most severe forms of abuse. Moreover, we systematically performed adjustments excluding the gender effect, known to represent a potential confounder on the association between trauma and psychosis. Reference Fisher, Morgan, Dazzan, Craig, Morgan and Hutchinson40
However, some limitations should also be considered. Reliance on the retrospective reporting of abuse might increase the risk of recall bias. However, the reliability of patients affected by psychosis in referring trauma has been clearly demonstrated; Reference Fisher, Craig, Fearon, Morgan, Dazzan and Lappin41 their reports were independent of symptoms, stable over time and generally consistent with other sources of information. It has also been proved that retrospective recall yields an underestimation of the phenomenon, rather than an overestimation. Reference Hardt and Rutter42 Despite clear evidence of association between trauma, cannabis and psychosis, our data do not elucidate whether childhood traumatic experiences and drug misuse represent vulnerability factors for psychosis or environmental stressors that trigger the disorder acting on a pre-existing vulnerability. Traumatic experiences and drug misuse could both be vulnerability agents, decreasing the individual's resilience in response to other stressors such as migration, and leading to psychosis. They might represent two different environmental stressors, acting – in an additive or multiplicative way – on another type of vulnerability (possibly genetic). Childhood trauma could enhance vulnerability and cannabis use acts as an exacerbating agent or vice versa. Finally, because of the relative rarity of abusive experiences, resulting in small numbers, no further adjustments for social factors (such as employment or socioeconomic status) and/or genetic vulnerability (familiality) have been carried out in the analysis.
Future research
In addition to clarifying whether cannabis and childhood trauma represent vulnerability factors or stressors triggering psychosis, studies should also analyse this association, taking into account other environmental variables and/or biological markers. A population-based, longitudinal prospective study design, with long-term follow-up (from infancy to adulthood) would be most appropriate. Reference Poulton, Moffitt and Silva43 Overall, our study suggests that patients with first-episode psychosis exposed to childhood trauma constitute a distinctive subgroup characterised by diverse features in terms of nosology and drug use. It has elucidated, albeit partially, to what extent the presence of childhood trauma affects features of first-episode psychosis. Finally, this study may provide some important hints for specific therapeutic and/or preventive interventions, which might carry within themselves an enhanced impact on illness course, outcomes and prognosis.
Funding
The study was funded by the Ministry of Health, Italy – Ricerca Sanitaria Finalizzata, Code .
Acknowledgements
We thank all members of the Genetics Endophenotypes and Treatment: Understanding early Psychosis (GET UP) group; see online supplement DS1 for full details of the group.






eLetters
No eLetters have been published for this article.