A high consumption of free sugars is associated with dental caries, CVD and higher energy intake, leading to an increased risk of overweight and obesity(Reference Te Morenga, Howatson and Jones1,2) . As a result, the WHO currently recommends a global reduction in intakes of free sugars, suggesting these should constitute no more than 10 % of total energy intake(2), which, based on a 2000-calorie diet, equates to approximately twelve teaspoons of sugars per d. A further reduction to 5 % of total energy intake is advised for optimal health benefits(2). Despite these guidelines, in numerous countries, sugar consumption continues to surpass recommended thresholds(Reference Walton, Bell and Re3).
To assist with the reduction of dietary free sugars, some public health organisations(4–6) advise limiting the consumption of all sweet-tasting foods and beverages, regardless of whether the sweet taste originates from free sugars, low/no-calorie sweeteners or occurs naturally in foods, such as fruit. The rationale is that regular exposure to sweet-tasting foods and beverages increases sweet taste preferences, thereby increasing the consumption of foods and beverages that contain free sugars. It is therefore proposed that limiting exposure to the experience of sweet taste will reduce sweet taste preferences, leading to reduced sweet food and beverage consumption and consequently lower free sugar intakes(4–6). Although this idea may appear logical, based on research on dietary exposure(Reference Mela and Risso7), limited research has been conducted to examine the effects of repeated dietary sweet taste exposure on subsequent generalised preferences and intakes of sweet foods and beverages.
Furthermore, this research lacks consensus. A recent systematic review suggests that clear conclusions regarding the existence or direction of effects of modifying dietary sweet taste exposure cannot be made due to the limited and heterogeneous evidence base(Reference Appleton, Tuorila and Bertenshaw8). The majority of available studies also focus on testing the effects of repeated exposure to either a single sweet-tasting food item, such as a sweet beverage(Reference Ebbeling, Feldman and Steltz9–Reference Kendig, Chow and Martire11) or sweet snack(Reference Hetherington, Bell and Rolls12), or a single aspect of the diet, such as breakfast(Reference Appleton, Rajska and Warwick13,Reference Carroll, Chen and Templeman14) . Although these studies provide some evidence to test the rationale behind the recommendations to reduce sweet food and beverage consumption, the observed effects are potentially confounded by eating behaviours outside of the intervention protocols. To date, only one study of which we are aware has accounted for all eating behaviours by assessing the effects of exposure to an entirely sweet-tasting or an entirely non-sweet-tasting diet for 24 h(Reference Griffioen-Roose, Hogenkamp and Mars15). The findings from this study, by Griffioen-Roose et al. (Reference Griffioen-Roose, Hogenkamp and Mars15), contradict the predictions made above. They demonstrate that a 24-h exposure to a predominantly sweet-tasting diet led to reduced rather than increased preferences and intakes of sweet-tasting foods and beverages at an ad libitum buffet(Reference Griffioen-Roose, Hogenkamp and Mars15). A further study of interest is that by Wise et al. (Reference Wise, Nattress and Flammer16). Participants in this study were asked to replace 40 % of energy from simple sugars with energy from fats, proteins and complex carbohydrates without consuming low-calorie sweeteners, which, while unmeasured, presumably also reduced the sweet taste of the whole diet. This study found no changes in sweet food preferences following exposure for 3 months. The taste profile of the diet, however, was not explicitly adjusted or monitored.
Extending this previous research, the present study aimed to assess the effects of a whole-diet, sweet taste intervention for 6 d. Participants were asked to increase, decrease or make no change to their sweet food and beverage consumption for 6 d. Our outcome measures were pleasantness, desire to eat and sweet taste intensity, for sweet and non-sweet foods, and sweet food and beverage intake. The study was explicitly about the effects of the taste of the diet, rather than the sugar content. We hypothesised that there would be changes in all outcomes over time in intervention groups and no changes in a usual diet control group. No predictions were made regarding the direction of effects.
Methods
Design
This study utilised a parallel-groups, randomised controlled trial design with three arms. Participants were randomised to either increase, decrease or make no change to their daily intake of sweet-tasting foods and beverages for 6 consecutive days. All outcomes were assessed at two time points, on day 0 (baseline) and day 7 (end), alongside measures of adherence to the assigned diet.
Participants
A priori power calculations were based on changes in pleasantness ratings of approximately 6–9 mm (sd = approx. 13–17 mm), as reported in response to sweet taste exposure over 6 d in two previous studies(Reference Hetherington, Bell and Rolls12,Reference Hetherington, Pirie and Nabb17) . For a two-sided α of 0·05 and power of 0·8, these calculations estimated the need for forty participants per intervention group. Eligibility criteria for the study were being over the age of 18 years, non-vegan and non-smoker, regularly consuming breakfast, having no food allergies, not pregnant or breastfeeding, not dieting or trying to lose weight and being willing and able to undertake all study requirements. Participants were recruited using personal contacts, posters and online advertisements and through internal research volunteering platforms. To conceal our specific interest in sweet foods, the trial was described as a study of ‘Eating Behaviours’ with candidates advised that they would be required to modify specific aspects of their diet as instructed, although details of the modification were not given at this stage. In advance of participation, all interested candidates received study information and consent documents, and all participants provided written informed consent.
The trial was designed and conducted according to the guidelines laid down in the Declaration of Helsinki (1983), the Ethical Guidelines of the British Psychological Society and the Research Ethics Codes of Practice of Bournemouth University, UK, and the University of Bristol, UK. All procedures involving human participants were approved by the Research Ethics Committees of Bournemouth University (ID: 47051/48807/45568) and the University of Bristol (ID: 06121760961) prior to commencement. Risk assessments were carried out before data collection, with regular reviews undertaken throughout the trial and all risks addressed accordingly.
Intervention/control
Participants were allocated to one of three trial arms: ‘increase sweet food consumption’, ‘decrease sweet food consumption’ and ‘no diet change’ (control). In the ‘increase sweet food consumption’ arm, participants were instructed to increase their consumption of sweet foods and beverages with the instruction ‘Please increase your consumption of all sweet foods and drinks’. Participants were given examples of foods and beverages, taken from the Sensory-Diet database(Reference Lease, Hendrie and Poelman18), which would be suitable to consume at different meals, including fruit, some sweet vegetables (e.g. tomatoes, sweetcorn, carrots), low-calorie-sweetened foods and beverages and some sugar-sweetened foods and beverages. In the ‘decrease sweet food consumption’ arm, participants were instructed to decrease their consumption of sweet foods and beverages with the instruction ‘Please reduce your consumption of all sweet foods and drinks’ and were given examples of non-sweet foods and beverages that would be suitable to consume at different meals, as above. Importantly, the foods highlighted to participants in these two groups were given only as examples. In addition, each participant was encouraged to judge for themselves which foods would be appropriate for them to consume to adjust the taste of their diet as requested. The purpose of this procedure was to ensure that the intervention was experienced by each participant as intended (i.e. as sweet or not sweet). This avoided imposing the researchers’ assumptions about the foods that are experienced as tasting sweet v. not sweet by each individual. For those in the control arm, no dietary change was required. Participants were simply asked to ‘Continue consuming all foods and drinks that you were consuming last week’. Intervention instruction guides were provided to participants in written form for them to take away and refer to as they wished. In addition, on receipt of their instructions, participants were reminded that the aim of the study (as disclosed during consent procedures) was to investigate the effects of a dietary change and were asked to make this change as substantial as possible to enhance our chances of finding effects. The researcher in contact with participants was not aware of the specific instructions given, but contact details of an additional researcher were also given should questions arise during the course of the study. The instruction guides for the three conditions are given in the online Supplementary Materials. Participants were asked to undertake the intervention for 6 d (days 1–6) with outcomes assessed on day 0 and day 7.
Outcomes
Our primary outcomes were pleasantness and desire to eat for sweet and non-sweet foods and sweet food intake assessed at an ad libitum cold, buffet-style, breakfast meal. Secondary outcomes were perceived sweet taste intensity of the sweet and non-sweet foods, self-reported adherence to the allocated diet and measures of appetite.
Pleasantness and desire to eat
Pleasantness and desire to eat sweet and non-sweet foods were assessed on each test day using a taste perception test. Participants were instructed to taste and consume bite-sized portions of six different foods (see Table 1), comprised of both sweet and non-sweet items of a range of textures. Amounts provided are given in the online Supplementary Materials (Table SM1). For the one bite of each food, participants were asked to rate pleasantness and desire to eat on 100 mm visual analogue scales using paper and pen. The instructions for these scales were ‘How PLEASANT does this food taste to you right now?’ (response anchors: ‘not at all pleasant’, ‘extremely pleasant’) and ‘Now, rate how strong your DESIRE TO EAT more of this food is right now?’ (response anchors: ‘not at all strong’, ‘extremely strong’)(Reference Rogers and Hardman19). The foods were tasted in a pre-specified order, and participants were required to take a sip of water between each food item to limit the mixing of flavours. The bite-sized portions were consumed in full to avoid differential impacts on subsequent test meal intake measures. Food order varied between participants in a counterbalanced manner, but it remained the same on day 0 and day 7 for each individual.
Table 1. Foods served in the taste perception test and at the ad libitum cold buffet-style breakfast

* All foods were manufactured by Sainsbury’s Supermarkets Ltd., London, UK, with few exceptions: Madeline cake was manufactured by Bonne Maman, Gâteaux Bonne Maman, Contres, France; strawberry jam was manufactured by Hartley’s, Hain Celestial, Leeds, UK; butter was manufactured by Lurpak, Arla Foods Ltd, Leeds, UK; peanut butter was manufactured by Whole Earth, Kallo Foods Ltd, Surrey, UK; soft cheese was manufactured by Philadelphia, Uxbridge, UK, and bread was manufactured by KingsMill, Allied Bakeries, Maidenhead, UK.
Sweet food intake
Sweet food intake was assessed using an ad libitum cold buffet-style breakfast(Reference Hill, Rogers and Blundell20). Participants were presented with a variety of sweet and non-sweet foods and invited to consume as much or as little as they desired. The foods served, including their taste profiles and texture, are listed in Table 1, with amounts provided in the online Supplementary Materials (Table SM2). All foods are commonly consumed in the UK and have been used in a previous study to illustrate changes in intake over time(Reference Appleton, Rajska and Warwick13). For each participant, foods were individually weighed before and after breakfast to allow calculations of the percentage weight consumed from sweet foods and sweet foods and beverages, percentage of energy consumed from sweet foods and sweet foods and beverages, the weight of sugar consumed from foods and from foods and beverages and percentage of energy consumed from sugar from foods and from foods and beverages. Due to the lack of agreement regarding the most appropriate metric for assessing dietary sweet food intake(Reference Trumbo, Appleton and De Graaf21), several measures of intake were employed.
Sweet taste intensity
Sweet taste intensity was assessed on each test day in the taste perception test as above. For each of the six foods provided participants were also asked to rate sweet taste intensity on paper and pen 100 mm visual analogue scales, using the instruction ‘How SWEET does this food taste to you right now?’ (response anchors: ‘not at all sweet’, ‘extremely sweet’).
Adherence
Adherence to the intervention instructions was assessed at the end of the intervention period. Participants were asked how well they adhered to their allocated diet (‘How well did you adhere (manage to keep) to your allocated diet?’, response anchors: ‘not at all’, ‘extremely’), how difficult they found it to adhere to their allocated diet (‘How difficult did you find it to adhere (manage to keep) to your allocated diet?’, response anchors: ‘not at all’, ‘extremely’) and how different their allocated diet was from their usual diet (‘How different was your allocated diet from your usual diet?’, response anchors: ‘not at all’, ‘extremely’). Responses were made using paper and pen 100 mm visual analogue scales and were verified using records of sweet food consumption over the previous day and verbal reports of difficulties over the intervention week.
Appetite
Ratings of hunger, fullness and thirst were also undertaken using paper and pen 100 mm visual analogue scales at the start of each test session to allow for differences in appetite on each test day. Participant age and sex were also collected for descriptive purposes.
Procedure
The study was run from both the University of Bristol, UK (February 2018–May 2018), and from Bournemouth University (January 2023–May 2023, October 2023–March 2024). The initial study began at the University of Bristol and, following disruptions due to COVID-19, was continued later at Bournemouth University.
Data collection was carried out at the Nutrition and Behaviour Unit at the University of Bristol and the Eating Behaviours Laboratory at Bournemouth University. Participants visited the testing site fasted and rested on day 0 and day 7 during pre-booked time slots. Visits were scheduled between 08.00 and 11.00, and the timeslots remained the same on both occasions. Upon arrival, participants were seated individually at a table where they were presented with the taste perception test. After completing this test, participants received their cold buffet-style breakfast. The entire procedure lasted approximately 30 min and was repeated exactly on both testing occasions, with three exceptions. At the end of day 0 following all data collection, participants were provided with their dietary intervention. On day 7, participants also completed the adherence questions before the taste perception test, and they were asked about any difficulties experienced over the intervention period. After their breakfast, they were also debriefed about the purpose of the research and thanked for participating in the study.
To maintain a researcher-blinded study design, an independent researcher with no contact with participants randomised participants to one of the trial arms using a random number generator. Participants were randomised at a ratio of 1 (increase): 1 (decrease) at the University of Bristol and subsequently at a ratio of 1 (increase): 1 (decrease): 1 (no change) at Bournemouth University, to result in a final sample with a ratio of 2 (increase): 2 (decrease): 1 (no change). Group allocation was concealed using white sealed, opaque envelopes, and throughout the trial, the researcher in direct contact with participants remained unaware of each participant’s group allocation. To support the blinding, participants were asked not to disclose any information about the instructions they received to the researcher conducting the testing. Although it was impossible to blind the participants to their group allocation, they were unaware of the true aim of the trial and the instructions received by other participants.
Prior to commencement, the study was registered on Clinicaltrials.gov (Initial Study ID: NCT03427658, registration on 9 February 2018, Complete Study ID: NCT05672017, registration on 5 January 2023). We adhered to our trial registrations in all aspects with the exception that sweet food intake was measured only at breakfast rather than at breakfast and lunch as proposed in the registration for the initial study. The study was run using identical interventions and measures in both locations, with the exception that in Bristol, participants discussed their dietary change with a (independent) researcher and were given the written instruction guide, while in Bournemouth, participants were only provided with the written instruction guide, which included a contact to ask questions.
Analysis
Data for all outcome measures were carefully processed and collated using Microsoft Excel. Data from the University of Bristol and Bournemouth University were combined and analysed together to enhance power. At this stage, the researcher handling the data was not aware of the exposure group to which each participant had been allocated.
Following unblinding, data were described and analysed. Ratings for pleasantness, desire to eat and sweet taste intensity were averaged across all sweet foods and, separately, across all non-sweet foods tested, resulting in two scores per outcome measure, one for sweet and one for non-sweet foods. These were then analysed using 3 (increase sweet food consumption, decrease sweet food consumption, no diet change) × 2 (day 0, day 7) × 2 (sweet foods, non-sweet foods) repeated-measures ANOVA. For the sweet food intake measures, the weight of sweet foods and beverages consumed, in grams, was calculated by subtracting the weight of sweet foods and beverages returned to the kitchen from the amount served at breakfast, consequently allowing calculations of the percentage weight consumed from sweet foods and beverages. Manufacturer’s information was then used to calculate the percentage of energy consumed from sweet foods and beverages, weight of sugar consumed and percentage of energy consumed from sugar. Calculations were made for foods only, that is, for the amount of food consumed in the meal regardless of beverages consumed and the percentage of this that was consumed from sweet foods, and for foods and beverages together, where the percentage of sweet foods and beverages consumed was calculated from total foods and beverages consumed. Intake was then analysed using 3 (increase sweet food consumption, decrease sweet food consumption, no diet change) × 2 (day 0, day 7) repeated-measures ANOVA. Adherence and appetite were analysed using 3 (increase sweet food consumption, decrease sweet food consumption, no diet change) × 2 (day 0, day 7) repeated-measures ANOVA. Correlations between outcomes in the taste perception test and food intake measures were also conducted.
Analyses were undertaken on an intention-to-treat basis, with missing data imputed using models based on sex, age and baseline data. Regression models were also run in addition to the analyses above to account for individual differences in self-reported adherence to the interventions. Regression analyses were chosen rather than per-protocol analyses to avoid the use of an arbitrary cut-off to determine adequate adherence/non-adherence and allowed for differences at baseline between participants and a fuller exploration of the available data. These analyses sought to predict taste perceptions and sweet food intake on day 7 based on group allocation, self-reported adherence, self-reported difficulty, self-reported difference from usual diet, sex, age, location (Bristol, Bournemouth), outcome measure on day 0 and self-reported hunger and thirst on day 7. For models predicting pleasantness, desire to eat and sweet taste intensity, a cluster regression model accounted for clustering by ID and included a food type predictor to allow for the consideration of perceptions of both sweet and non-sweet foods in the same model. Exploratory ANOVA analyses were also repeated, as above, to investigate differences between the two intervention groups (increase sweet food consumption, decrease sweet food consumption) to ensure any effects were not masked by the inclusion of the usual diet control group.
Main analyses were conducted in SPSS (version 28.0.0.0), and regression analyses were conducted in Stata (version 15). Significance was set at P = 0·05.
Results
Participants
One hundred and four participants were recruited in total, with thirty-six participants in Bristol and sixty-eight participants in Bournemouth. Forty participants were randomised to increase their sweet food consumption, forty-three were randomised to decrease their sweet food consumption and twenty-one were randomised to maintain their usual sweet food intake (no diet change). Participant flow through the study is illustrated in Fig. 1.

Figure 1. CONSORT diagram, illustrating participant flow.
Participant characteristics are given in Table 2. The three groups were comparable for sex, but participants in the no diet change condition were younger than those in the other two conditions. As the average age for all groups falls within the young adult category, and mainstream dietary recommendations apply to adults aged 18–65 years, we considered these differences unlikely to be relevant to our research question.
Table 2. Baseline statistics for all participants in the increase sweet food consumption (n 40), decrease sweet food consumption (n 43) and no diet change (n 21) groups (Numbers and percentages; mean values and standard deviations)

Adherence
All 104 participants completed baseline measures, and 102 (98 %) participants completed testing on day 7. Two participants, both in the no diet change group, dropped out due to changes in personal circumstances that were unrelated to the study. Adherence outcomes across the three groups are given in Fig. 2 (with data provided in online Supplementary Materials Table SM3). Participants in the no diet change group reported significantly greater adherence to the study instructions, greater ease in following these instructions and less deviation from their usual diet compared with participants in the increase and decrease sweet food consumption groups (smallest t(59) = 2·50, P = 0·02). No significant differences in self-reported adherence or in deviation from usual diet were found between the two sweet taste intervention groups (largest t(81) = 1·27, P = 0·21); however, participants asked to reduce their sweet food consumption reported it to be significantly more difficult to adhere to their allocated diet than participants asked to increase their sweet food consumption (t(81) = 2·45, P = 0·02, M diff = 14 mm, se = 6). Adherence was negatively correlated with difficulty (r = –0·20, P = 0·04) and with deviation from the usual diet (r = –0·32, P < 0·01), and difficulty was positively correlated with deviation from the usual diet (r = 0·51, P < 0·01).

Figure 2. Adherence to the allocated diet for all participants in the sweet food increase (n 40), sweet food decrease (n 43) and no diet change (n 21) exposure groups (mean and standard error, letters demonstrate significant differences within each measure: a v. b v. c, P < 0·05). VAS, visual analogue scales.
Pleasantness and desire to eat
Ratings for pleasantness and desire to eat on day 0 and day 7 are shown in Fig. 3. Data are given in online Supplementary Materials Table SM4.

Figure 3. Pleasantness and desire to eat the sweet foods and non-sweet foods in the taste perception test in the sweet food increase (n 40), sweet food decrease (n 43) and no diet change (n 21) exposure groups (mean and standard error, letters demonstrate significant differences: a v. b, c v. d, P < 0·05). VAS, visual analogue scales.
Pleasantness
Sweet foods were rated as more pleasant than non-sweet foods (F(1, 101) = 48·27, P < 0·001, np 2 = 0·32; M diff = 14 mm, se = 1·6). Pleasantness ratings for all foods also decreased from day 0 to day 7 (F(1, 101) = 11·43, P = 0·001, np 2 = 0·10, M diff = 4 mm, se = 1·4). No statistically significant dietary exposure group × time interactions (largest F(2, 101) = 1·25, P = 0·29, np 2 = 0·02) or group × time × food type interactions (F(2, 101) = 1·32, P = 0·27, np 2 = 0·03) were found.
Desire to eat
Desire to eat for sweet foods was higher than for non-sweet foods (F(1, 101) = 24·05, P < 0·001, np 2 = 0·19; M diff = 11 mm, se = 1·7), and desire to eat all foods decreased from day 0 to day 7 (F(1, 101) = 5·22, P = 0·02, np 2 = 0·05, M diff = 3 mm, se = 1·4). There were no statistically significant dietary exposure group × time interactions (largest F(2, 101) = 2·22, P = 0·11, np 2 = 0·04) or group × time × food type interactions (F(2, 101) = 1·60, P = 0·21, np 2 = 0·03).
Sweet food intakes
Participants consumed a mean (sd) 260 (170) g foods, 603 (278) g foods and beverages and 2334 (1483) kJ foods, 2441 (1489) kJ food and beverages at the breakfast meal, with a mean (sd) 33·2 (23·1) (range 0–100) % food weight from sweet foods, 30·0 (16·7) (0–64·1) % food and beverage weight from sweet foods and beverages, 28·2 (20·3) (0–100) % food energy from sweet foods and 37·2 (22·0) (0–100 %) % food and beverage energy from sweet foods and beverages. All sweet food and beverage intake outcomes on day 0 and day 7 per exposure group are given in Fig. 4 and in online Supplementary Materials Table SM5. No statistically significant effects of time were observed either in foods only or in foods and beverages (largest F(1, 101) = 2·14, P = 0·15, np 2 = 0·02). No statistically significant dietary exposure × time interactions were observed either in foods only or in foods and beverages (largest F(2101) = 2·53, P = 0·09, np 2 = 0·05).

Figure 4. Sweet food and beverage consumption in the buffet-style breakfast meal in the sweet food increase (n 40), sweet food decrease (n 43) and no diet change (n 21) exposure groups (mean and standard error, no significant differences, P < 0·05).
Sweet taste intensity
Sweet foods were rated as sweeter than non-sweet foods (F(1, 101) = 835·21, P < 0·001, np 2 = 0·89; M diff = 48 mm, se = 2), and there was a significant food type × time interaction (F(1, 101) = 7·59, P = 0·007, np 2 = 0·07), where non-sweet foods were rated as sweeter on day 7 compared with day 0 (t(103) = 3·40, P < 0·01), but there was no change in sweet taste intensity for the sweet foods (t(103) = 0·73, P = 0·47). A significant dietary exposure group × time interaction was also found (F(1, 101) = 4·13, P = 0·02 np 2 = 0·08). Participants in the decreased sweet food consumption group reported all foods as more sweet on day 7 compared with day 0 (t(42) = 3·36, P < 0·01, M diff = 6 mm, se = 2), but no changes were found in the other two groups (largest t(39) = 0·38, P = 0·70, M diff = 1 mm, se = 2). Data are pictured in Fig. 5 and are included in online Supplementary Materials Table SM4.
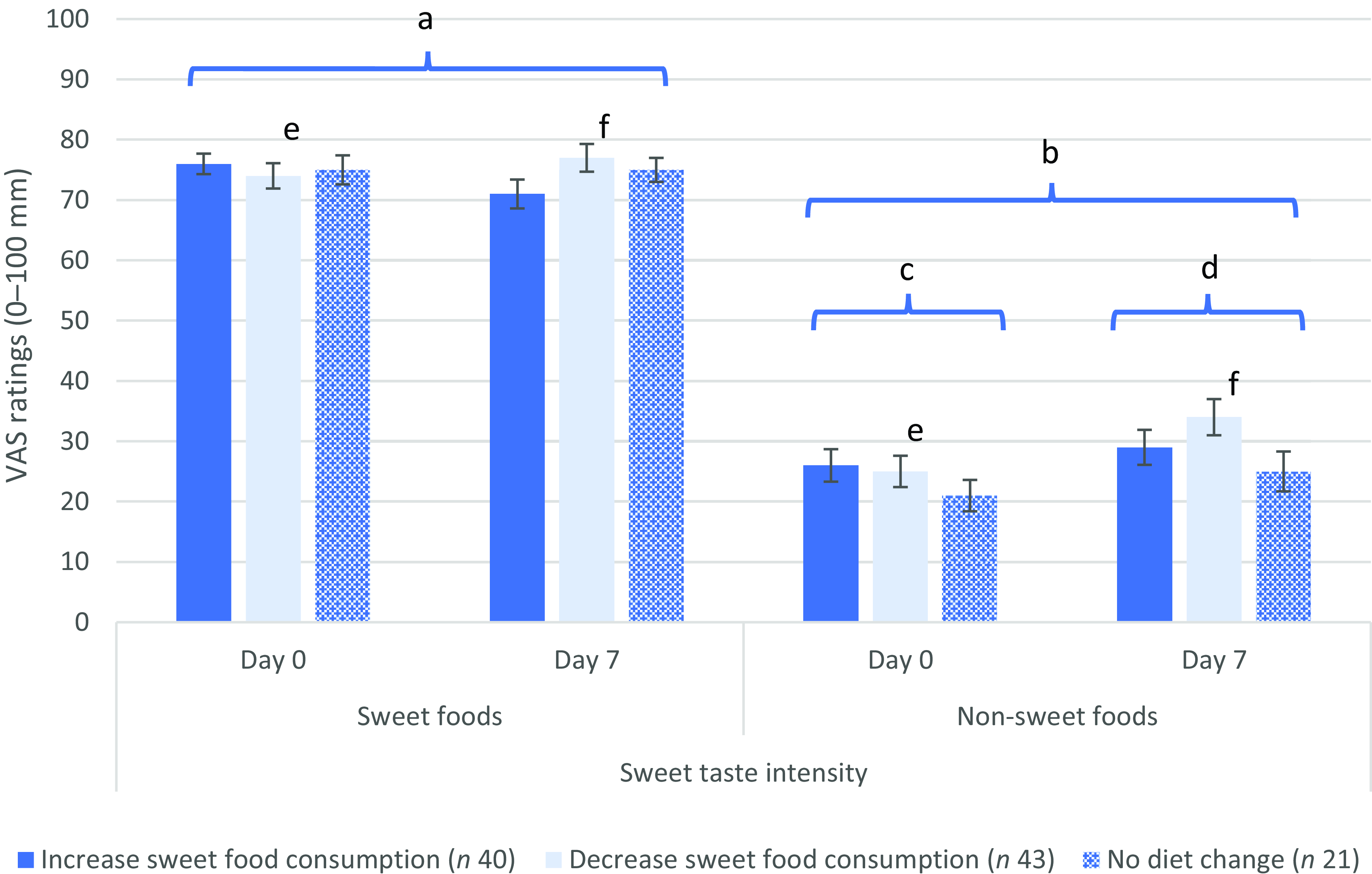
Figure 5. Sweet taste intensity for the sweet foods and non-sweet foods in the taste perception test in the sweet food increase (n 40), sweet food decrease (n 43) and no diet change (n 21) exposure groups (mean and standard error, letters demonstrate significant differences: a v. b, c v. d, e v. f, P < 0·05). VAS, visual analogue scales.
Appetite
Hunger, fullness and thirst ratings did not change over time (largest F(1, 101) = 2·60, P = 0·11, np 2 = 0·03), and no statistically significant dietary exposure group × time interactions were detected for any of these measures (largest F(2, 101) = 1·27, P = 0·29, np 2 = 0·03).
Associations between pleasantness, desire to eat, sweet taste intensity and sweet food intakes
Pleasantness and desire to eat ratings were highly positively correlated (smallest r = 0·73, P < 0·01), and both pleasantness and desire to eat for all foods were correlated with rated sweet taste intensity (smallest r = 0·23, P = 0·02). Pleasantness and desire to eating ratings for sweet foods were also positively correlated with all percentage measures of sweet food intake (smallest r = 0·17, P = 0·02).
All sweet food intake measures were correlated (smallest r = 0·17, P = 0·01), with the exception of measures for sugar consumed from foods and from foods and beverages. Sugar consumed from foods was associated with sugar consumed from foods and beverages (r = 0·45, P < 0·01), percentage of food weight consumed from sweet foods, percentage of food energy consumed from sweet foods and percentage of energy consumed from sugars from foods (smallest r = 0·30, P < 0·01). Sugar consumed from foods and beverages was associated only with the percentage of food and beverage weight consumed from sweet food and beverages (r = 0·24, P < 0·01). Neither pleasantness ratings nor desire to eat ratings were correlated with sugar consumed from foods or from foods and beverages (largest r = 0·10, P = 0·16). Sugar consumed from foods and from foods and beverages was instead associated with the total amount consumed both in weight and energy (smallest r = 0·36, P < 0·01). Total weight and energy consumed were correlated (r = 0·41, P < 0·01). Ratings of hunger and thirst were correlated (r = 0·14, P = 0·04). Hunger was also negatively associated with sugar consumed from foods and beverages (r = –0·16, P = 0·02), and thirst was negatively associated with the weight of foods consumed, sugars consumed from foods and from foods and beverages and percentage of energy consumed from sugars from foods (smallest r = 0·18, P = 0·01). Sweet taste intensity ratings were not correlated with any of the sweet taste intake measures (largest r = 0·10, P = 0·15).
Regression analyses
The findings above from ANOVA were confirmed by the regression models. Full results from all regression analyses are provided in the online Supplementary Materials (Tables SM6 and SM7). All taste ratings at day 7 were predicted by the regression models (smallest F(11 103) = 15·16, P < 0·01, R 2 = 0·40). Higher pleasantness and higher desire to eat ratings for all foods on day 7 were associated with higher ratings for pleasantness and desire to eat, respectively, on day 0 (smallest B = 0·562, P < 0·01), and consideration of sweet v. non-sweet foods (smallest B = −5·193, P = 0·03). Desire to eat was also associated with increased adherence to the intervention (B = 0·151, P = 0·02), with a similar trend in pleasantness ratings (B = 0·116, P = 0·06). No associations were found with intervention group (largest B = −1·525, P = 0·25).
All sweet food intake measures at day 7 were predicted by the regression models (smallest F(10, 103) = 3·65, P < 0·01, R 2 = 0·28, adjusted R 2 = 0·20), and no associations with intervention group were found (largest B = 4·292, P = 0·06). All intakes at day 7 were associated with the same measure at day 0 (smallest B = 0·311, P < 0·01). The marginal effect of group was found in the percentage of food and beverage weight consumed from sweet foods and beverages (B = 4·292, P = 0·06), but effects in the percentage of food weight consumed from sweet foods were very different (B = 0·492, P = 0·85), and effects of the intervention group in all other intake measures were also small (largest B = 1·348, P = 0·55). Effects in foods and beverages but not in foods only would suggest the effects of the group to result from the beverage consumption (apple juice and water) and the relative proportion of the beverages consumed. Considering water consumption was required as part of the taste test procedure and apple juice was the only other beverage available and that this may have been consumed, or not, for many reasons other than its sweet taste, including flavour liking and perceptions of healthiness, we think these findings more likely reflect the test situation rather than sweet food choices in the real world. The percentage of energy consumed from sweet foods and beverages and percentage of energy consumed from sweet foods were also negatively associated with age (smallest B = −1·015, P = 0·02), and the percentage of energy consumed from sugars from foods was also associated with being male (B = −3·951, P = 0·04) and having a lower thirst (B = –0·080, P = 0·04).
Higher ratings for sweet taste intensity for all foods on day 7 were associated with higher ratings for sweet taste intensity on day 0 (B = 0·581, P < 0·01), consideration of the sweet v. non-sweet foods (B = −14·520, P < 0·01) and being in the decrease sweet food consumption group (B = −3·184, P = 0·01).
Exploratory analyses
Exploratory ANOVA analyses to investigate differences between the two intervention groups (increase sweet food consumption, decrease sweet food consumption) without consideration of the control group are provided in the online Supplementary Materials. These analyses demonstrate the same effects as are reported above.
Discussion
This study investigated the effects of repeated whole-diet sweet taste exposure on the subsequent pleasantness, desire for, sweet taste intensity and intake of sweet foods and beverages. One hundred and four participants were randomised to increase, decrease or make no change to their consumption of sweet foods and beverages for a period of 6 d, and outcomes were measured in a laboratory test day on days 0 and 7. One hundred and two (98 %) participants completed the study, and self-reported adherence with the dietary intervention was moderate to good. We found statistically significant effects of dietary exposure on perceived sweet taste intensity but no effects for pleasantness, desire to eat or any of the sweet food intake measures. Regression analyses taking the degree of self-reported adherence into account confirmed these findings. We also found differences in self-reported difficulty with adherence to the allocated diets.
In relation to sweet taste intensity, participants who were instructed to reduce their consumption of sweet foods and beverages reported higher sweet taste intensity for the study foods after the intervention compared with before. In contrast, there were minimal effects on perceived sweet taste intensity for participants who increased or did not change their dietary exposure to sweet taste. Our findings are consistent with other studies that report an increased sweet taste intensity perception for sweet foods and/or beverages following a reduction in the consumption of sweet foods and/or beverages(Reference Ebbeling, Feldman and Steltz9,Reference Wise, Nattress and Flammer16) . Ebbeling et al. (Reference Ebbeling, Feldman and Steltz9) found increased sweet taste intensity ratings for sweet solutions in those replacing sugar-sweetened beverages with unsweetened beverages, while no effects were found for those replacing sugar-sweetened beverages with artificially sweetened beverages, and Wise et al. (Reference Wise, Nattress and Flammer16) found increased sweet taste intensity ratings for sweet puddings and beverages following 3 months on a low sugar compared with a usual diet. In our study, this effect is most plausibly explained as a contrast effect(Reference Appleton, Tuorila and Bertenshaw8), where the perceived sweet taste intensity of the tested items is heightened compared with the low sweet taste of the background diet. Alternative mechanisms where changes in sweet taste intensity may occur, for example, as a result of an increased sensitivity in sweet taste receptors(Reference Wise, Nattress and Flammer16), seem unlikely given the short nature of our intervention compared with the likely time needed to observe changes in taste receptor physiology or activity(Reference Perea-Martinez, Nagai and Chaudhari22–Reference Sung, Vaziri and Wilinski24).
While effects in sweet taste intensity were found, we found little evidence for an effect of dietary sweet taste exposure on ratings for pleasantness or desire to eat or in our sweet food intake measures. These findings are consistent with similar studies where sweet taste exposure is modified for an extended period(Reference Mela and Risso7,Reference Appleton, Tuorila and Bertenshaw8) . Several studies using dietary sweet taste modification now report no effects on various measures of taste hedonics(Reference Appleton, Rajska and Warwick13,Reference Carroll, Chen and Templeman14,Reference Wise, Nattress and Flammer16,Reference Thanarajah, DiFeliceantonio and Albus25) or sweet food intakes(Reference Fantino, Fantino and Matray10,Reference Appleton, Rajska and Warwick13,Reference Carroll, Chen and Templeman14,Reference Appleton26) . Very short-term effects of sweet taste exposure have been reported; for example, Griffioen-Roose et al. (Reference Griffioen-Roose, Hogenkamp and Mars15) report reduced sweet food preferences and intakes immediately following 24 h consumption of a solely sweet diet, and various single exposure studies report similar effects(Reference Appleton, Rogers and Blundell27–Reference Rogers, Ferriday and Irani29). These effects can be explained as a result of sensory-specific satiety – satiation for a specific taste as a result of prior consumption of that taste(Reference Rolls, Rolls and Rowe30), but importantly, these effects are only found immediately or very shortly (< 2 h) after the prior taste experience(Reference Rogers, Ferriday and Irani29). In studies where preference and/or testing takes place after 2 h or after an overnight fast, these sensory-specific satiety effects are not found(Reference Fantino, Fantino and Matray10,Reference Appleton, Rajska and Warwick13,Reference Carroll, Chen and Templeman14) . In such studies by Ebbeling et al. (Reference Ebbeling, Feldman and Steltz9) and Kendig et al. (Reference Kendig, Chow and Martire11), some limited effects were reported in preference measures, where reduced sweet taste exposure is reported to result in reduced preferences for sweet solutions and reduced liking for highly sweet solutions, respectively. These studies were notably longer than the one reported here, with interventions lasting for 12 months(Reference Ebbeling, Feldman and Steltz9) and 12 weeks(Reference Kendig, Chow and Martire11); thus, maybe the 1-week duration is simply not long enough for effects to develop. Other studies where sweet food items, sugar-sweetened beverages specifically, have been replaced within the diet for 6-month periods also report some changes in intakes of other sweet foods(Reference Hedrick, Davy and You31,Reference Piernas, Tate and Wang32) , but effects are somewhat inconsistent(Reference Mela and Risso7,Reference Appleton, Tuorila and Bertenshaw8) . Studies using long interventions, for example, a 6-month whole-diet intervention tested by Čad et al. (Reference Čad, Tang and de Jong33) and a 10-month intervention tested by Kjølbæk et al. (Reference Kjølbæk, Manios and Blaak34), will contribute significantly to questions on the stability and/or flexibility of sweet taste preferences and subsequent impacts on sweet food intakes.
Interestingly, also within our data, while we find effects of exposure in ratings of sweet taste intensity and no effects in ratings of pleasantness or desire to eat, we do find positive correlations between these measures. We also find positive associations between pleasantness and desire to eat sweet foods and all percentage measures of sweet food intake, although we find no associations between sweet taste intensity ratings and percentage of sweet food intakes, and we find no associations between any of the perception measures and sugar intakes. Positive associations between the hedonic and intensity ratings are likely a reflection of high innate preferences for sweet taste(Reference Beauchamp35) and an often greater proportion of sweet likers than sweet dislikers in the general population (e.g. (Reference Garneau, Nuessle and Mendelsberg36, Reference Iatridi, Hayes and Yeomans37)) – an effect that was most plausibly demonstrated here as a result of our use of commercially available foods in the taste test, with a limited range of sweet taste intensities. Standard investigations of sweet taste preferences for a range of concentrations of sweet taste often result in an inverted U-shaped function around a central optimal sweet taste concentration (e.g. (Reference Cad, Tang and Mars38)), but these studies typically use extreme (high and low) concentrations of a sweet tastant, while our effects are limited to those in the central section of this range. It was the hedonic ratings, however, not the intensity ratings, that were associated with sweet food intake. These findings confirm an independence between the sweet taste hedonic and intensity constructs(Reference Garneau, Nuessle and Mendelsberg36–Reference Tan and Tucker39), as is also shown in other studies where effects are found in one measure and not in the other (e.g. (Reference Wise, Nattress and Flammer16)). Our findings also suggest that sweet food consumption is more determined by liking for the sweet taste rather than by the perception of high sweet taste intensity. This conclusion is also reported in a recent systematic review(Reference Tan and Tucker39), where hedonic evaluations, specifically preferences and liking for sweet taste, were more predictive of dietary sweet food and beverage intakes compared with perceived sweet taste intensities. Heterogeneity, however, was also found, due to differences in the study methods and measures used, and may depend on the population studied(Reference Tan and Tucker39). In a study population of mostly sweet likers, sweet taste intensity, liking and intake will all probably be positively correlated, while in a study population of mostly sweet dislikers, sweet taste intensity will probably be negatively correlated with sweet taste liking, while liking and intake may remain positively associated.
The dissociation between the hedonic ratings, the percentage of sweet food intakes and the measures of sugar consumed is also noteworthy. The amount of sugar consumed in fact appears to be more a reflection of total consumption at the breakfast meal. These findings demonstrate the value of distinguishing sweet food consumption from sugar intakes. While sweet foods are likely to contain sugar, the two concepts are easily dissociated through the consumption of non-sugar-sweetened (low-calorie-sweetened) sweet foods and beverages(Reference Carocho, Morales and Ferreira40) or the consumption of foods containing sugar that may not usually be classified as sweet, including bread, cereal products, savoury sauces, processed snack products and ready meals (see (41)). The association between sweet taste and sugar content will necessarily differ in specific foods, but the absence of a strong association in this study suggests that greater consideration of these differences may be needed in advice aimed at reducing free sugar intakes. Many public health agencies currently link sweet food consumption directly with sugar intakes and subsequently with overweight and obesity(4–6). Data such as ours however demonstrate inconsistent associations between sweet food consumption and sugar intakes. Systematic reviews now also demonstrate limited relationships between sweet food consumption and body weight, overweight or obesity, where sweet food consumption has been assessed using dietary taste profiles(Reference Cox, Hendrie and Carty42) or where sweet taste v. no sweet taste is provided from low-calorie sweeteners(Reference Laviada-Molina, Molina-Segui and Pérez-Gaxiola43–Reference Rogers and Appleton45).
From a public health perspective, another important finding from our study is that those asked to reduce their sweet food and beverage intake reported this as more difficult than those asked to increase their sweet food and beverage intake or maintain their usual diet. Considering the innate pleasure provided by sweet taste, at least for a majority of people(Reference Beauchamp35–Reference Iatridi, Hayes and Yeomans37), it may be unsurprising that the removal or restriction of this source of pleasure will be difficult. Many treat foods, even for adults, are sweet tasting(Reference Beauchamp35), and suggestions that such pleasures and treats should be forgone have been reported as undesirable(Reference Appleton and McGowan46–Reference Tang, Mars and James49). Strategies to reduce free sugar intakes where the sweet taste of the diet is retained may be more acceptable and more likely to achieve success, particularly over the longer term.
We also detected a significant reduction in pleasantness and desire to eat for all dietary items in the taste test over the intervention period. As this was observed for both sweet and non-sweet foods, we assume that repeated exposure to the same dietary items over the two test days caused this reduction, possibly due to boredom or monotony(Reference Dalenberg, Nanetti and Renken50,Reference Essed, van Staveren and Kok51) . This same effect was found in our previous study using the same taste test and test meal(Reference Appleton, Rajska and Warwick13).
The present study provides significant contributions to the limited body of evidence regarding the impact of repeated dietary sweet taste exposure on pleasantness, desire to eat and actual consumption of sweet-tasting foods and beverages. The study was of a moderately large sample size and incorporated various measures of relevance to sweet food intake. Our whole-diet modification approach for an extended period is a unique feature of the study, making it the first to directly reflect the public health recommendations for effects on free sugar intakes(4–6) and test their real-world application. Importantly, participants were also explicitly asked to increase or decrease their sweet food consumption, rather than their consumption of specific foods or sugars; thus, the study is a genuine test of exposure to a taste defined as sweet by those experiencing it. Our use of a participant-centred intervention and our specific methods to assess our outcomes increase the ecological validity of our study. Some limitations must also be noted. First, we investigated effects at a taste test and in a cold buffet-style breakfast meal. For our taste test, we used three sweet and three non-sweet commercially available foods, at only one (familiar) concentration of sweet taste intensity. Standard sensory testing where different levels of a tastant are provided in multiple versions of the same product would have extended our measurements and may have resulted in increased sensitivity(Reference Trumbo, Appleton and De Graaf21,Reference Cad, Tang and Mars38) . Our use of familiar food items also potentially limited our chances of finding effects(Reference Cad, Tang and Mars38). The breakfast buffet meal similarly may have lessened our chances of detecting effects as a result of the usual unvaried nature of food choice at breakfast. However, the breakfast meal provided an extensive choice, and our methods allowed the detection of small changes, for example, to the amount of butter or preserves consumed. Both our taste test and buffet meal were intended to assess pleasantness, desire to eat and food intake in a realistic and generalisable scenario(Reference Hill, Rogers and Blundell20,Reference Trumbo, Appleton and De Graaf21,Reference Venditti, Musa-Veloso and Lee52) . Another important limitation was that participants undertook the dietary intervention in their own homes, and although we have self-report measures of adherence, we have no certainty that the interventions were undertaken as requested. We also have no indication of the extent to which the interventions were undertaken, that is, the degree to which participants increased or decreased their sweet food intake. All participants agreed to change their diet as requested prior to signing up for the study, the instructions for the intervention were clear (no questions were asked, and no difficulties were reported), and our aim was to mimic the everyday public health scenario, but closer supervision or the provision of suitable foods for the 6-d intervention period(Reference Čad, Tang and de Jong33) would have increased intervention fidelity and reduced these concerns. Lastly, while the popular discourse in sweet food reduction recommendations is about preferences(4–6), we did not measure preference per se, using a forced choice scenario(Reference Trumbo, Appleton and De Graaf21), but instead measured pleasantness and desire to eat. Subtle differences between these measures have been reported(Reference Rogers and Hardman19,Reference Trumbo, Appleton and De Graaf21,Reference Iatridi, Hayes and Yeomans37–Reference Tan and Tucker39) .
In conclusion, we found limited effects of whole-diet sweet taste exposure for 6 consecutive days on the pleasantness, desire for or the consumption of other sweet-tasting foods and beverages. Changes in perceived sweet taste intensity were detected, such that reduced sweet taste exposure resulted in increased perceived sweet taste intensity; however, this measure does not seem to be associated with the consumption of sweet-tasting foods and beverages. Together with the current literature, our findings suggest that regular exposure to sweet taste does not significantly affect the hedonic evaluation or intake of sweet-tasting foods and beverages. These conclusions suggest that public health recommendations that propose that limiting the consumption of sweet-tasting foods and beverages will reduce sweet taste preferences may require revision.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524003209.
Acknowledgements
This project was supported by Bournemouth University, UK, and the University of Bristol, UK. Grateful thanks are also extended to Louisa-Katharina Hommels, Sophie Peel and Elena Sundle, University of Bristol, and to Nicole Durnhoefer and Cameron Stacey, Bournemouth University, for their help with data collection. Data are available from the corresponding author on reasonable request.
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
A. D. B.: formal analysis; investigation; writing – original draft; writing – review and editing; P. J. R.: conceptualisation; methodology; supervision; writing – review and editing; K. M. A.: conceptualisation; formal analysis; methodology; supervision; writing – review and editing.
A. D. B.: There are no conflicts of interest. P. J. R.: P. J. R. has received funding for research from Sugar Nutrition UK, provided consultancy services for Coca-Cola Great Britain and received speaker’s fees from the Global Stevia Research Institute, ILSI (International Life Sciences Institute)-Brasil, ILSI-Europe, ILSI-India and the International Sweeteners Association and other support from industry for travel expenses for workshops and conferences where he presented research on sugar and low-calorie sweeteners. K. M. A.: For work in the area of sweet taste and low-calorie sweeteners, K. M. A. has previously received research funding from Unilever R&D Vlaardingen, NL; ILSI-North America, USA; and the International Sweeteners Association, BE. She has current funding from a consortium of the American Beverage Association, Arla Foods, Cargill R&D Centre Europe BVBA, DSM-Firmenich SA, International Sweeteners Association, SinoSweet Co. Ltd, Cosun Nutrition Center and Unilever Foods Innovation Centre Wageningen and from the Coca-Cola Company, USA. She has received speaker’s expenses from the International Sweeteners Association, BE; PepsiCo, USA; ILSI-North America, USA; the CBC group, Israel; and EatWell Global.










