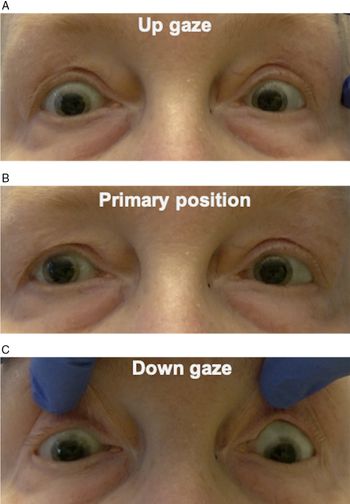
A 72-year-old woman was seen in consultation for new-onset intermittent binocular vertical diplopia. Her past medical history was significant for metastatic spindle cell carcinoma of the lung with multiple brain metastases. On examination, she was found to have a supranuclear upgaze and right infraduction palsy, consistent with a vertical one-and-a-half syndrome (Figure 1). Magnetic resonance imaging (MRI) of the brain with contrast was performed, and this revealed a new enhancing mass involving the right midbrain and diencephalon, consistent with a new metastasis (Figure 2). At 5-week follow-up, she had progressed to have both complete up- and downgaze supranuclear palsies.

Figure 1: Assessment of ocular motility revealed an upgaze palsy (A) and infraduction palsy in the right eye (C). There was no deviation in primary position (B). This was overcome with oculocephalic maneuvers, indicating that this was supranuclear in nature.

Figure 2: T1 MRI post-contrast demonstrates a metastatic lesion involving the right midbrain and diencephalon (arrow) most consistent with a metastasis.
Spindle cell carcinoma is a very rare form of lung cancer, representing only 0.2–0.3% of all primary pulmonary cancers.Reference Qi, Liu and Feng1 This cancer is highly malignant with rapid progression and poor prognosis. In addition, brainstem metastases are uncommon – representing only 5–7% of brain metastases in all malignancies – and carry a poor prognosis with a median survival of less than 1 year.Reference Yoo, Park, Kwon and Kim2 There are few existing case reports of brainstem metastases in patients with spindle cell carcinoma of the lung.Reference Li, Chen and Zhao3
Vertical one-and-a-half syndrome is an extremely rare finding, previously reported in patients with unilateral ischemic stroke of the meso-diencephalon. It is a result of disruption of the posterior commissure and decussating fibers to the oculomotor complex.Reference Bogousslavsky and Regli4 Although the pathways involved in vertical gaze are incompletely understood, it is hypothesized that fibers from the contralateral rostral interstitial nucleus of medial longitudinal fasciculus (riMLF) via the posterior commissure contribute to upgaze and fibers from the ipsilateral riMLF contribute to downgaze.Reference Sato, Takahashi and Matsumoto5 Therefore, a lesion involving the posterior commissure and ipsilateral riMLF could produce a vertical one-and-a-half syndrome.
Other horizontal one-and-a-half syndrome variants secondary to pontine metastases have been rarely described in the literature. These include reports of an isolated one-and-a-half syndrome or those in association with other cranial neuropathies.Reference Jackel, Gittinger, Smith and Passarelli6–Reference Choi, Kim and Chung9 To our knowledge, this is the first case to demonstrate that vertical one-and-a-half syndrome can result from metastatic disease. Therefore, new extraocular motor deficits presenting in patients with a history of cancer should prompt urgent neuroimaging to assess for new metastatic lesions.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
EC and JAM were involved in project conception, manuscript preparation, and editing.