CLINICIAN CAPSULE
What is known about the topic?
The 2016 Canadian Triage and Acuity Scale updates introduced frailty as a level 3 first-order modifier to up-code frail patients with non-urgent presentations.
What did this study ask?
Is there a relationship between triage acuity and frailty, and are these measures associated with the same patient outcomes?
What did this study find?
Triage acuity and frailty are independent measures and are associated with different outcomes.
Why does this study matter to clinicians?
Comprehensive frailty assessment post-triage may further identify at-risk seniors that can benefit from additional geriatric assessment, intervention, and resources.
INTRODUCTION
The demographic shift has resulted in an increase of older adults seeking health care, with emergency departments (ED) acting as a conduit and a common access point for older people in search of medical attention.Reference Roberts, McKay and Shaffer1,Reference Hwang and Morrison2 As a result, EDs are counted upon to modify traditional models of care to meet the unique physical and psychosocial needs of older adults, who frequently present for care.Reference Perry, Macias Tejada and Melady3,Reference Carpenter, Bromley and Caterino4 The complexity of older ED patients warrants the need to identify those at risk for poor patient outcomes. Frailty screening has been proposed as a strategy to achieve this goal.Reference Carpenter, Bromley and Caterino4,Reference Jorgensen and Brabrand5 Frailty is a multifactorial syndrome characterized by a heightened vulnerability to adverse health events and a diminished physiologic reserve, inhibiting homeostatic recovery from stressors.Reference Fried, Tangen and Walston6,Reference Rockwood, Song and MacKnight7 When assessed in the ED, frailty has proven to be a consistent predictor of hospitalization, hospital length of stay, functional decline, and death.Reference Brousseau, Dent and Hubbard8–Reference Sirois, Griffith and Perry12
The 2016 Canadian Triage and Acuity Scale (CTAS) guidelines were updated based on expert consensus. Recommendations to enhance geriatric triage education and to incorporate a rapid frailty assessment within triage were endorsed to supplement decision making upon ED arrival. As standard practice in Canada, all patients presenting to the ED are assigned a CTAS score to prioritize and sort patients based on acuity of illness. The CTAS is a single-item Likert scale that ranges from one to five, with a score of one regarded as the most urgent and five the least urgent. The frailty modifier within CTAS is a level 3 first-order modifier designed to help identify frail patients with apparent non-urgent presentations who would otherwise have been assigned a CTAS level of 4 or 5. This is based on concerns that these patients may suffer more or deteriorate if subjected to prolonged waits for care.Reference Bullard, Musgrave and Warren13 Prior work has demonstrated the predictive and clinical utility of screening for frailty in the ED.Reference Jorgensen and Brabrand5 However, little is known about how frailty and triage acuity relate to one another. Identifying the relationship between frailty and triage acuity will help clarify the information value of frailty in triage, and whether frailty screening can further support clinical decision-making outside of triage.
We investigated the relationship between triage acuity and frailty scores in patients 75 years of age and older who presented to the ED before the implementation of the 2016 CTAS updates. We also compared their associations with patient outcomes, such as: hospitalization, hospital length of stay, and hospital recidivism. Bearing in mind that the CTAS is purposed to assess and prioritize medical acuity, whereas frailty screening is intended to highlight geriatric complexity and vulnerability, we hypothesized that there would be no relationship between these two measures. We also hypothesized and that these measures would be independently associated with different patient outcomes.
METHODS
Study design
We conducted a secondary analysis of the Canadian data from a multi-site, multinational prospective cohort study, the interRAI Multinational ED study.Reference Costa, Hirdes and Heckman14,Reference Gray, Peel and Costa15
Study setting and population
Data were collected from eight ED sites across five provinces in Canada (e.g., Ontario, Nova Scotia, Manitoba, Saskatchewan, and British Columbia) between November 2009 and April 2012.Reference Costa16 Patients 75 years of age and older were recruited during ED registration. Patients were excluded if: they were in severe medical distress, they were expected to die within 24 hours of arrival as determined by the nurse assessor, or they did not speak English and/or did not have a valid interpreter. Data were collected by research nurses or allied health professionals during day time hours (8 am to 7 pm) based on staff availability and extant literature reporting high day time usage by older adults.Reference Downing and Wilson17 Ethics approval was obtained from the respective academic institutions and research ethics boards of all participating hospitals.Reference Costa16
Measurement and variables
Upon study enrolment, all patients received a formal geriatric assessment by a nurse or allied health professional using the interRAI ED Contact Assessment. All assessors were trained on the ED Contact Assessment and its supplementary software.Reference Costa16 The ED Contact Assessment is a brief assessment and a standardized clinical decision support tool to inform diagnostic, treatment, and discharge decision-making in the ED, and to improve communication and continuity postdischarge.Reference Costa AP and Arino-Blasco S18 The items of the ED Contact Assessment have established test content validity in acute care,Reference Wellens, Deschodt and Boonen19 inter-rater reliability,Reference Hirdes, Ljunggren and Morris20,Reference Wellens, Van Lancker and Flamaing21 and predictive validity across a series of outcomes in the ED setting.Reference Brousseau, Dent and Hubbard8,Reference Costa, Hirdes and Heckman14 After the initial assessment, a standardized follow-up was conducted at 90 days post ED or hospital discharge to determine hospital length of stay and post-discharge outcomes. Those admitted for in-patient services received follow-up by means of manual chart reviews or a secondary analysis of electronic medical records. Those discharged from the ED were contacted by means of telephone. Hospital medical and/or mortality records were reviewed if the telephone follow-up was unsuccessful.
The ED frailty index was created by Brousseau et al.Reference Brousseau, Dent and Hubbard8 using the items of the ED Contact Assessment to gauge the number of health deficits present at the time of ED assessment. A cumulative health deficit model was used to create the frailty index with guidance from methods proposed by Searle et al.Reference Searle, Mitnitski, Gahbauer, Gill and Rockwood22 In the general population, older adults deemed to be frail using a cumulative health deficit model have a median index score of 0.4.Reference Rockwood, Andrew and Mitnitski23 The ED frailty index is presented as a fraction, with the numerator being the number of health deficits present and the denominator being the total number of deficits possible in the ED Contact assessment. The ED frailty index has demonstrated predictive validity in both Canadian and international cohorts.Reference Brousseau, Dent and Hubbard8 In our study, frailty was operationalized using the ED frailty index scores assigned to patients during their ED visit, and triage acuity was based on the CTAS score assigned to patients upon presentation to the ED. Data were collected before the introduction of the frailty modifier and enhanced triage nurse geriatric education. As a result, the CTAS scores examined in this study reflect practice before the 2016 CTAS revisions, preventing contamination between the CTAS and frailty scores assigned.
The primary outcome measure for this study was hospital admission resulting from the index ED visit. Hospital length of stay, future hospitalization, and repeat ED visitation were also of interest. Hospital length of stay was dichotomized to parallel the figures reported by provincial governing bodies. An extended in-patient length of stay was defined as patients who experienced a hospital length of stay greater than the 90th percentile. Future hospitalization was defined as any hospital stay that occurred within 90 days of discharge from the index hospital presentation. Repeat ED visitation was defined as any ED visit that occurred within 30 days of discharge from the index hospital presentation. Patients who died in hospital were excluded from outcomes concerning hospital recidivism.
Data analysis
Descriptive statistics were reported using general measures of frequency and central tendency. Spearman rank was conducted to examine the relationship between CTAS and ED frailty index scores. Frailty and triage acuity were dichotomized with the top 33% of frailty scores deemed to be the most frail, and those with a CTAS of three or less deemed to be higher acuity. A series of chi-square tests were conducted to compare the proportion of post-disposition outcomes across patients with varying frailty and CTAS scores. Multiple logistic regression was performed to determine the adjusted observed relationships between the ED frailty index, CTAS, age, and gender, in relation to the outcome measures. For multivariable models, frailty was analyzed as a continuous variable to retain information, and also as quintiles to match the split of the CTAS and to provide a paralleled comparison. Cases with missing data were deleted within each analysis. Analyses were performed using SAS 9.4 (SAS institute Inc, Car, NC, USA), and sample size calculations were performed using G*Power 3.1.9.4. The required sample size was 1,046 patients based on a conservative correlation coefficient of 0.1, assuming 90% power and a two tailed-alpha of .05.Reference Faul, Erdfelder, Lang and Buchner24
RESULTS
The cohort contained 2,153 older adults who presented to the ED for care. Overall, 1,119 (51.9%) of ED visits resulted in hospitalization, with 139 patients (6.4%) dying in hospital. The mean age of all patients was 82.2 (SD ± 7.3), 60.7% were female, 37.3% lived alone, 41.3% had used the ED in the previous 90 days, and 80.1% of the sample received an urgent triage score (CTAS 1–3). ED frailty index scores were calculated for 89% (n = 1,916) of all observations, with a mean index score of 0.3 (range = 0–0.8).Reference Rockwood, Andrew and Mitnitski23 Missing data were minimal with a range of 0–3.8% (mean of 0.71%) across all variables examined. Additional patient demographics can be found in Table 1. We found no evidence of an association between the CTAS and ED frailty index scores assigned to patients within the ED (r = .001; p = 0.99).
Table 1. Patient characteristics
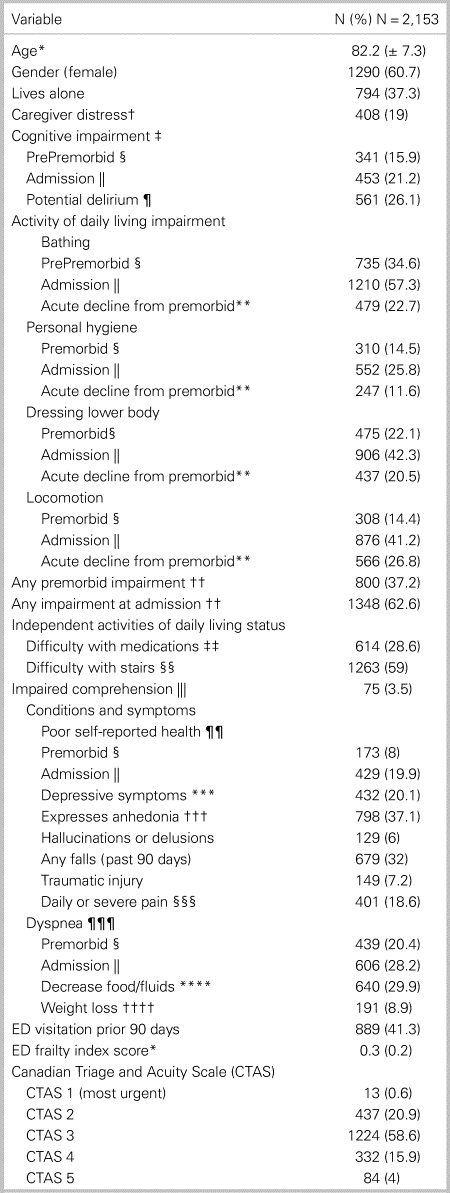
ED = emergency department.
*Data are reported as a mean and standard deviation.
† Primary informal helper(s) expresses feelings of distress, anger, or depression.
‡ Modified independent or any impairment in making decisions regarding tasks of daily living.
§Premorbid: the 3-day period before the onset of the current acute illness or episode.
|| Admission: the past 24 hours or time since acute illness or episode that prompted the ED visit.
¶ Acute change in mental status from person's usual functioning (e.g., restlessness, lethargy, difficult to arouse, altered environmental perception).
** Acute decline from premorbid: at admission, new impairment relative to premorbid.
†† Any supervision or any physical assistance in bathing, personal hygiene, dressing lower body, and locomotion.
‡‡ Difficulty remembering to take medicines, opening bottles, taking correct drug dosages, giving injections, or applying ointments.
§§Supervision or any assistance during full flight of stairs (12 to 14 stairs).
||| Sometimes, rarely, or never understands direct communication.
¶¶ When asked, “In general, how would you rate your health?” person responds “Poor.”
*** When asked, patient reports feeling sad, depressed, or hopeless in past 3 days.
††† When asked, patient reports little interest or pleasure in things they normally enjoy.
§§§ Pain that is severe or excruciating in past 3 days.
¶¶¶ Dyspnea at rest or present when performing normal day-to-day activities.
**** Noticeable decrease in the amount of food usually eaten or fluids usually consumed.
†††† Weight loss of 5% or more in last 30 days, or 10% or more in past 180 days.
Table 2 displays a combined assessment of triage acuity and frailty across post-disposition outcomes. Older adults considered to be both frail and of high acuity were most likely to be admitted for in-patient care (67.3%; p = < 0.001). Those deemed to be frail but who lacked medical acuity were most likely to experience an extended hospital length of stay (20.8%; p = < 0.001), or a hospitalization within 90 days of discharge from the index hospital presentation (28.5%; p = 0.04). For a comprehensive display of frailty and triage acuity across all prognostic factors, refer to appendix A.
Table 2. Comparison of Frailty and Triage Acuity (CTAS) across patient putcomes
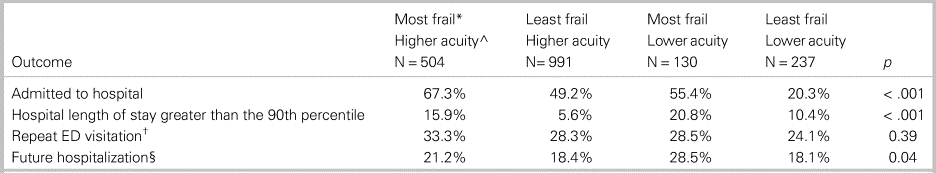
ED = emergency department.
* Most Frail = Top 33% of ED Frailty Index scores, Least Frail = Bottom 66% of ED Frailty Index scores.
^ Higher Acuity = Canadian Triage Acuity Scale 1–3, Lower Acuity = Canadian Triage Acuity Scale 4–5
† Returned to an ED within 30 days of the index ED presentation.
§ Admitted to a hospital within 90 days of the index ED presentation.
After adjusting for triage acuity, age, and gender, multivariable logistic regression determined that a 0.1 unit increase in the ED frailty index score is associated with hospital admission (odds ratio [OR] = 1.5; 95% confidence interval [CI] = 1.4–1.6), an extended hospital length of stay (OR = 1.4; 95% CI = 1.2–1.6), future hospitalization (OR = 1.2; 95% CI = 1.1–1.3), and repeat ED use (OR = 1.1; 95% CI = 1.04–1.2). The CTAS was only associated with hospital admission, with patients assigned a score of one (OR = 4.9; 95% CI = 1.02–27.9), two (OR = 6; 95% CI = 3.3–11.4), or three (OR = 3.6; 95% CI = 2.1–6.7) at greater risk for admission when compared with a non-urgent CTAS score of five. Table 3 displays a multivariable model with frailty divided into quintiles to match the split of the CTAS.
Table 3. Adjusted odds ratio for frailty and triage acuity across ED disposition outcomes

ED = emergency department; CTAS = Canadian Triage Acuity Scale.
Sample sizes vary due to missing data.
DISCUSSION
Interpretation of findings
To our knowledge, this is the first study to examine the relationship between triage acuity and frailty, and to compare their associations across several outcomes. We found that frailty and triage acuity are independent measures; however, both have clinical utility and are important for driving separate outcomes. Our findings demonstrated that frailty is associated with hospital admission, an extended hospital length of stay, repeat ED visitation, and future hospitalization, for older adults seeking emergency care. The CTAS was only associated with hospital admission. Finally, we identified a distinct cohort of frail older adults who presented for non-urgent medical attention. This group experienced the greatest number of hospitalized days per patient, and the highest rates of hospitalization post-discharge.
Comparison to previous studies
Our findings are consistent with existing literature examining the predictive utility of frailty screening in the ED.Reference Brousseau, Dent and Hubbard8–Reference Salvi, Morichi and Grilli10 Despite the heterogeneity of instrumentation used to measure frailty across different emergency settings, studies examining similar outcomes consistently produced paralleled results. Little is known about the predictive utility of the CTAS for older adults in Canada. Bearing in mind that the CTAS was not purposed to predict patient outcomes, prior studies have demonstrated that the CTAS score assigned is associated with hospital admission, length of stay, and resource usage among the general Canadian population.Reference Dong, Bullard and Meurer25–Reference Murray and Levis28 Studies outside of Canada have demonstrated that triage acuity is predictive of the same outcomes for older ED patients.Reference Baumann and Strout29,Reference Lee, Oh and Peck30
Clinical implications
Acuity is the primary function of the ED, and assigning a triage score to patients upon ED presentation is the standard of care. However, frailty and other geriatric syndromes are commonly overlooked by ED clinicians and processes.Reference Rutschmann, Chevalley, Zumwald, Luthy, Vermeulen and Sarasin31,Reference Carpenter, Griffey, Stark, Coopersmith and Gage32 We support the decision of CTAS to up-code frail patients presenting for non-urgent complaints, given their increased risk for under-triage and decompensation while waiting for treatment.Reference Platts-Mills, Travers and Biese33,Reference Grossmann, Zumbrunn, Frauchiger, Delport, Bingisser and Nickel34 However, the lack of collinearity between triage acuity and frailty suggests that there is further information to be gained from measuring frailty, above and beyond the CTAS score assigned. The high rates of hospital admissions, recidivism, and health service use by frail older ED patients presenting with low medical acuity underscores the value of frailty screening. Evaluating frailty as a measure encapsulated within triage acuity is likely to omit the geriatric complexity that drives health service use. Assessing frailty through a distinct lens may further highlight the unique needs and geriatric syndromes of frail older adults, information that is not apparent upon the review of a triage score.
Time constraints in triage along with the complex and multifaceted nature of frailty screening suggest that triage is a suboptimal environment to support an inclusive frailty assessment. A second and more comprehensive frailty screening during clinical treatment may be useful for case-finding to further identify seniors who could benefit from additional geriatric assessment, and targeted senior friendly pathways. The interRAI ED screener and the Identification of Seniors at Risk (ISAR) tool recommended by the geriatric ED guidelines are key examples of case-finding instruments currently embedded as the standard of care in many EDs.Reference Costa AP and Arino-Blasco S18,35 A common trait of these screening systems is that they produce an exclusive frailty score to supplement decision-making during clinical treatment. To obtain a similar effect with the CTAS modifier, and to prevent a loss of information during the transition of care from triage to treatment, ED clinicians should be made aware of patients who screen positive for frailty in triage. This information can be used to help guide emergency treatment and post-discharge follow-up. Cognizant of the limited resources and staffing available within the ED, comprehensive screening post-triage may be best suited to older ED patients who present with high geriatric complexity but low medical acuity.
Strengths and limitations
Our study is one of the few that used data with a comprehensive set of functional and geriatric syndromes not typically available in ED medical records. The secondary nature of the study limited our analyses to only those available in the archived data. Diagnostic information would have provided supplementary information to assist in understanding the clinical reasoning behind the ED disposition outcomes. Similarly, data were only collected during daytime hours; patient and visit characteristics may differ during night-time visitation. Finally, due to a low mortality event rate during the study period, we were unable to analyze mortality as an outcome.
Our findings are hypothesis generating, and future research is needed to determine the optimal timing of comprehensive frailty screening in the ED, and how to adapt traditional emergency management pathways to incorporate this practice post-triage. Given the recommendation for the CTAS frailty modifier, future studies should aim to examine the impact of the frailty modifier on time-to-treatment and other important patient outcomes. Finally, our study identified a unique subgroup of older adults with high frailty and low medical acuity driving health service use. Future research is needed to further characterize this distinct cohort.
CONCLUSION
We demonstrated that triage acuity and frailty are two distinct but clinically important constructs found to be associated with different outcomes for older ED patients. Frailty was associated with hospitalization, extended hospital length of stay, and hospital recidivism, demonstrating that this measure can be used to guide clinical decision-making post-triage. Frail older adults presenting to the ED with low medical acuity were identified as a subgroup of patients driving health service use.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/cem.2019.432.
Acknowledgements
The authors acknowledge and thank Dr. Michael Bullard for his review of this paper and guidance regarding the CTAS content.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
None declared.





