CVD remains a major cause of death worldwide, and its prevalence is still increasing globally(Reference Roth, Mensah and Johnson1). Early detection of subclinical atherosclerosis is an opportunity to allow optimal prevention and control of risk factors(Reference Faggiano, Dasseni and Gaibazzi2–Reference Stein, Korcarz and Hurst4). Carotid intima-media thickness (cIMT) and coronary artery calcification (CAC) score are non-invasive measurements and established surrogate markers of subclinical atherosclerosis(Reference Hoffmann, Massaro and D’Agostino5,Reference Nezu, Hosomi and Aoki6) . cIMT is obtained through an ultrasound examination of carotid arteries that identifies and quantifies the distance between the lumen intima and media adventitia interfaces(Reference Pignoli, Tremoli and Poli7,Reference Bots, Hoes and Koudstaal8) , which is altered from the initial phases of atherosclerotic disease(Reference Kanters, Algra and van Leeuwen9), while CAC is conducted via non-contrast cardiac computed tomography and is the most common method applied to evaluate and identify subclinical atherosclerosis(Reference Hoffmann, Massaro and D’Agostino5). However, both cIMT and CAC are useful tools to predict CVD events(Reference Faggiano, Dasseni and Gaibazzi2,Reference Lorenz, Markus and Bots10) .
Lifestyle factors such as regular physical activity, non-smoking, non-alcoholic consumption and a healthy dietary pattern are pointed as modifiable risk factors for CVD(Reference Joseph, Leong and McKee11), including subclinical atherosclerosis. The relationship between specific dietary components and nutrients and CVD has been well explored in the scientific literature(Reference Zong, Gao and Hu12–Reference Micha and Mozaffarian14). However, overall diet should be considered to interpret the diet-health-related effects(Reference Hu15). Diet quality scores or indices are useful for this purpose, as they are tools to assess nutrient adequacy, the analysis of geographic disparities and temporal fluctuations in dietary patterns and the evaluation of adherence to established dietary recommendations(Reference Fransen and Ocké16,Reference Ocké17) .
Diet quality scores can be developed and tailored for a given population(Reference Waijers, Feskens and Ocké18). The Cardiovascular Health Diet Index (CHDI) was proposed(Reference Cacau, Marcadenti and Bersch-Ferreira19), based on the dietary recommendations for a healthy diet to prevent CVD and promote cardiovascular health advocated by the American Heart Association (AHA)(Reference Benjamin, Virani and Callaway20), and includes other food groups relevant to cardiovascular health, such as legumes and dairy products, and food groups related to risk for CVD, such as red meat and ultra-processed foods. In this manner, the CHDI incorporates the most recent scientific findings pertaining to CVD prevention, aligning itself with the latest dietary recommendations from both the Dietary Guidelines for the Brazilian Population(21) and the recommendations of the AHA recommendations(Reference Lichtenstein, Appel and Vadiveloo22).
Although the CHDI score has demonstrated good relative validity and reliability parameters, its predictive criteria validity remains unexplored. Therefore, the primary objective of this study is to assess the association between the CHDI score and subclinical atherosclerosis, as determined by CAC over a 4-year period and cIMT over an 8-year period. Additionally, we aim to compare these associations with those obtained using the Healthy Eating Index-2015 (HEI-2015)(Reference Krebs-Smith, Pannucci and Subar23), a well-established diet quality score.
Material and methods
Study design and population
The Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) is a multicentre ongoing cohort of 15 105 male and female civil servants, who were active and retired workers from six institutions (five public universities and one public research institute) located in six different Brazilian cities from three major Brazilian regions (Northeast, Southeast and South). Briefly, the ELSA-Brasil study aimed to investigate the incidence and risk factors for CVD and diabetes in Brasil. All active or retired employees from the aforementioned institutions, aged between 34 and 74 years, were eligible for the study. The exclusion criteria were those with cognitive or communication disabilities, current or recent (< 4 months prior to the first interview) pregnancy and intention to quit work at the institution in the near future for reasons not related to retirement and if retired with the residence outside the corresponding metropolitan area of a study centre. Baseline data from ELSA-Brasil were collected by trained and certified personnel under strict quality control between August 2008 and December 2010 (n 15 105). The second visit of interviews and exams was between 2012 and 2014 (n 14 104), and the third wave took place between 2017 and 2019 (n 12 636). More details of the sample and data collection methods of this cohort study have been previously published(Reference Schmidt, Duncan and Mill24).
For the present study, two main outcomes were evaluated to define subclinical atherosclerosis: CAC and cIMT. For the analysis with CAC as the outcome, participants from the baseline and second wave were eligible. In brief, from the 15 105 participants in the baseline, only a sub-sample (n 5061) from the São Paulo Research Center underwent non-contrast computed tomography for CAC measurement at two different periods throughout the study. Individuals with no CAC measure at the baseline and follow-up, a history of CVD (myocardial infarction, stroke or coronary revascularization), no dietary data and no information on covariates (sociodemographic and lifestyle factors) were excluded. For the analysis with cIMT as the outcome, participants from the baseline and third wave were eligible. The same exclusion criteria described above for CAC analysis were also applied. The flow chart of the included participants is described in Fig. 1.

Figure 1. Flow chart presenting the study population from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) who were eligible for statistical analyses in this present study according to coronary artery calcification (CAC) incidence, CAC progression and carotid intima-media thickness (cIMT) changes over time.
The ELSA-Brasil study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures were approved by the research ethics committees of all research centres. All participants volunteered and signed an informed consent form. In addition, the present study was also approved by the research ethics committee of the School of Public Health of the University of São Paulo (no. 3.970.703).
Coronary artery calcification measurement
The CAC measurements were performed using a 64-slice multidetector computed tomography scanner (Brilliance 64, Phillips Healthcare) with a standard technique for CAC scoring, including prospective acquisition in mid-diastole, 120 kVp tube voltage and variable current based on BMI(Reference Bensenor, Goulart and Santos25). The CAC was expressed in Agatston units(Reference Agatston, Janowitz and Hildner26), and the percentile was evaluated in a blinded fashion by an experienced cardiologist using semiautomatic software (Calcium Scoring, Philip Workstation). CAC incidence was defined as a CAC of zero (CAC = 0) at the baseline followed by a CAC greater than zero (CAC > 0) at the follow-up. To compute the CAC incidence, 2224 individuals with CAC = 0 at the baseline were considered. CAC progression was defined according to the Hokanson method for those individuals who had a CAC > 0 at the baseline. To compute CAC progression, we considered 725 individuals with CAC > 0 at baseline. The difference between the follow-up square root transformed CAC measure and the baseline square root transformed CAC measure was calculated for each individual, and those who presented a change greater than 2·5 were classified with CAC progression(Reference Hokanson, MacKenzie and Kinney27) (Fig. 1).
Carotid intima-media thickness measurement
The cIMT measurement protocol was previously described(Reference Santos, Bittencourt and Oliveira28). Briefly, the ELSA-Brasil study acquired cIMT images in accordance with guidelines from the American and Brazilian Societies of Echocardiography. Images were captured using Toshiba Aplio XG ultrasound machines equipped with a 7·5 MHz linear transducer and then sent to the centralised reading centre in São Paulo for analysis. The ELSA-Brasil study used MIA software (Medical Imaging Applications) to standardise the reading and interpretation of carotid scans as previously described. For cIMT measurement, the common carotid artery was identified along its longitudinal axis with standard brightness and contrast settings. Measurements focused on the proximal far wall of the common carotid artery, specifically 1 cm proximal to the carotid bifurcation over a 1 cm segment, and both mean and maximum values were recorded for each common carotid artery.
Images were considered valid when clearly visualised left on the and right sides: (1) the anatomical guides for the common carotid artery, (2) interfaces between the lumen and the distant vessel wall and (3) interfaces between the media and the adventitious layers of the vessel wall. All patients were examined by technicians and/or physicians who had previously been trained and certified for this protocol. The intra- and interobserver variations were previously evaluated in the ELSA-Brasil study, and the results show excellent intra- and interobserver reproducibility for the mean cIMT measurements in the ELSA-Brasil study.
In this paper, we defined cIMT as the average between the mean left and the mean right cIMT values. The average values in millimetres (mm) from the measurements of left and right cIMT at baseline and 8-year follow-up were considered for analysis (Fig. 1).
Dietary assessment
Food consumption was assessed using a previously developed and validated semi-quantitative FFQ with 114 food items(Reference Molina, Faria and Cardoso29,Reference Molina, Benseñor and Cardoso30) . This FFQ comprises the past 12 months, and the questions are structured into three sections: (1) food products/food preparations, (2) measures of consumed products and (3) consumption frequencies with eight response options (more than 3 times/d, 2–3 times/d, once a day, 5–6 times a week, 2–4 times a week, once a week, 1–3 times a month and never/almost never). The daily consumption of each FFQ item (in g/d) was obtained by multiplying the portion size by the corresponding frequency.
Cardiovascular Health Diet Index computation
The CHDI was developed based on the AHA’s guidelines for a cardiovascular-healthy diet(Reference Cacau, Marcadenti and Bersch-Ferreira19). In summary, the AHA recommends the regular consumption of fruits and vegetables, fish and seafood, whole-grain cereals, nuts and legumes, while advising a reduced intake of sodium, sugar-sweetened beverages (SSB), processed meats and saturated fats. In creating the CHDI, the emphasis was placed on dietary patterns, focusing on food groups rather than specific nutrients. Additionally, other food groups were included in the CHDI, such as dairy products, due to their association with a lower risk of CVD(Reference Dehghan, Mente and Rangarajan31). Red meat was incorporated due to its connection with CVD(Reference Micha, Michas and Mozaffarian32), and ultra-processed foods were added because of their strong links to CVD, diabetes, hypertension and overall mortality(Reference Lane, Gamage and Du33). Thus, the CHDI recommends the consumption of fruits, vegetables, nuts, whole grains, legumes, fish, seafood and dairy products, while advising the reduction or avoidance of processed meats, SSB, red meat and ultra-processed foods for better cardiovascular health. In this study, ultra-processed foods were classified according to the Nova food classification system(Reference Monteiro, Cannon and Levy34). More detail regarding the development and validation of the CHDI process, including the components, cut-off points and validity results, is described elsewhere(Reference Cacau, Marcadenti and Bersch-Ferreira19).
For components such as fruits, vegetables, fish and seafood, whole grains, nuts, beans and dairy products, participants received a maximum score of 10 points if their consumption met or exceeded the recommended levels and a minimum score of 0 points if there was no consumption. Intermediate scores were assigned proportionally. Conversely, for components like SSB, red meat, processed meat and ultra-processed foods, the scoring process was reversed, with a minimum score of 0 points given for consumption meeting or exceeding the recommended values and a maximum score of 10 points awarded when there was no consumption. Intermediate scores were applied proportionally. The final score ranges from zero to 110 points, and the higher the score, the better the diet quality. Table 1 describes the components, cut-off points and score system. Online Supplementary Table S1 describes examples of foods components. More details on the development and validation process of the CHDI score can be found elsewhere(Reference Cacau, Marcadenti and Bersch-Ferreira19).
Table 1. Cardiovascular Health Diet Index (CHDI): components, cut-off points and scoring system
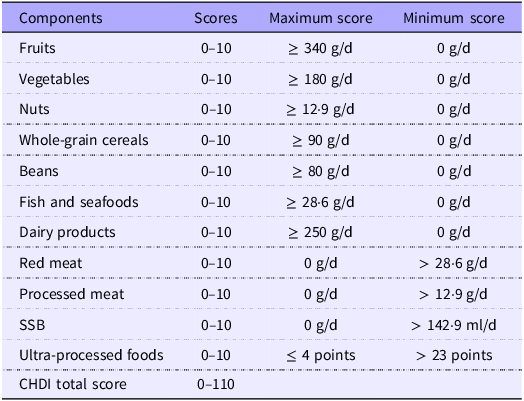
SSB, sugar-sweetened beverages.
Covariates
The sociodemographic characteristics and lifestyle habits were used as covariates. All the covariates included in this analysis were self-reported through standardised questionnaires performed by trained personnel under strict quality control at ELSA-Brasil assessment(Reference Bensenor, Griep and Pinto35). Participants were classified according to sex (male and female) and according to age as adults (34–59 years) and elderly (≥ 60 years). Self-reported race was classified into white, brown, black or Asian and Indigenous. Per capita family income, also based on self-report, was calculated as the total family monthly income divided by the number of family members and then divided in tertiles. Smoking was stratified as non-smokers (including ex-smokers) and current smokers. Alcohol consumption was obtained according to the amount ingested per week (male ≥ 210 g; female ≥ 140 g) and then dichotomised into high alcohol consumption (yes or no). Physical activity level during leisure time was classified as low (no or less than moderate category), moderate (> 150 min/week of moderate activity) or vigorous (≥ 75 min/week of vigorous activity) according to the International Physical Activity Questionnaire(Reference Craig, Marshall and Sjöström36).
Statistical analyses
Descriptive analysis was performed using proportions and means with standard deviation (sd) for categorical and continuous variables, respectively.
Poisson’s regression models with robust variance were performed to estimate the association between the CHDI score and CAC incidence (CACbaseline = 0 v. CACfollow-up > 0) and CAC progression dichotomous (CAC square root method > 2·5). In these models, the time between two measures (years) was considered using the option exposure on Stata. Linear regression models were fitted to evaluate the association between CHDI score with CAC progression as a continuous variable (square root method).
Linear mixed-effects regression was fitted to estimate the association between the CHDI score with longitudinal changes in the cIMT in the follow-up period. To explore whether an annual change in cIMT related to the CHDI score existed, that is, whether the association between the CHDI score with cIMT differed across the follow-up time, a CHDI score × time interaction term was added.
Crude models were fitted with the CHDI score as exposure and the cIMT or CAC as outcomes. All models (i.e. linear mixed and Poisson) were adjusted for potential confounders, including sex (male, female), age group (adults, elderly), self-reported race (white, brown, black or Asian and Indigenous), per capita income (tertiles), smoking status (non-smokers, current smokers), sporadic alcohol consumption (yes, no), physical activity level (low, moderate or vigorous) and total energy intake (kcal). In the analyses with cIMT, the statin and dyslipidaemia presence were included in the models, as they can influence the reduction of cIMT.
While the main analyses treated the CHDI score as a 10-point increase, additional analyses categorised it into tertiles. In addition, as the CHDI score is a diet quality score based on specific recommendations for cardiovascular health, we built regression models using the HEI-2015 as an alternative index of overall diet quality as an additional analysis. HEI-2015 is a diet quality score with thirteen components (total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy products, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars and saturated fats) that can range from 0 to 100 points(Reference Krebs-Smith, Pannucci and Subar23). The same models were built (i.e. linear mixed models and Poisson model), with the same adjustment variables.
All statistical analyses were performed using Stata (StataCorp), version 14.2, and the P-value < 0·05 was considered statistically significant.
Results
Descriptive results
Among the individuals with no presence of CAC at the baseline (n 2224), 331 exhibited CAC greater than zero during follow-up (14·9 %). The baseline CHDI scores for those included in the CAC incidence analyses ranged from 18·5 to 105·8 points, with a mean score of 54·6 points. Conversely, among those with CAC greater than zero at baseline (n 725), 442 displayed CAC progression during follow-up (61·0 %). For participants included in the CAC progression analyses, the baseline CHDI scores varied from 18·6 to 97·3 points, with a mean score of 57·4 points. Online Supplementary Tables S2 and S3 present the baseline characteristics of individuals in relation to CAC incidence and progression.
At baseline, the average cIMT measurement was 0·600 mm, while the baseline CHDI scores for participants included in the cIMT changes analyses ranged from 12·0 to 106·5 points, with an average score of 56·6 points. Detailed baseline characteristics related to cIMT can be found in online Supplementary Table S4.
Diet quality and coronary artery calcification incidence and progression
The mean follow-up period was 4·2 years. Table 2 presents the incidence risk ratio with their respective 95 % CI of the association between CAC incidence and each 10-point increase in the CHDI score. No association was observed after a 4-year follow-up, neither in the unadjusted nor in the fully adjusted model, indicating that higher scores in the CHDI had no effect on the CAC incidence. Accordingly, no association was observed between a 10-point increase in the CHDI score with CAC progression (Table 3). Furthermore, there was no observed significant association when evaluating the CHDI components in relation to either CAC incidence or progression or when the CHDI was evaluated in tertiles (data not presented).
Table 2. Poisson regression models of the association between each 10-point increase in the Cardiovascular Health Diet Index score with longitudinal coronary artery calcification (CAC) score. ELSA-Brasil, 2008–2010 to 2012–2014
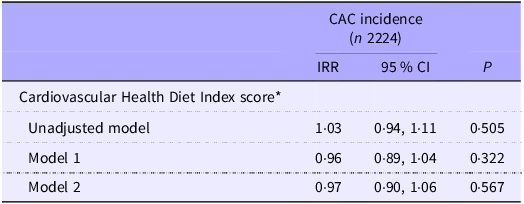
IRR, incidence risk ratio.
* As each 10-point increase. Model 1 adjusted by age, sex, self-reported race and per capita income. Model 2 adjusted by Model 1 plus smoking status, alcohol consumption, physical activity level and total energy intake.
Table 3. Poisson regression models of the association between each 10-point increase in the Cardiovascular Health Diet Index score with CAC progression. ELSA-Brasil, 2008–2010 to 2012–2014
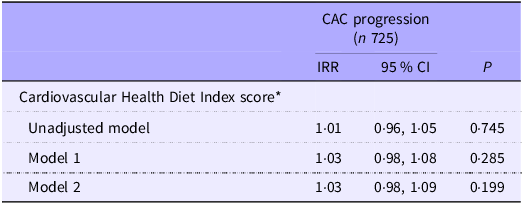
CAC, coronary artery calcification; IRR, incidence risk ratio.
* As each 10-point increase. Model 1 adjusted by age, sex, self-reported race and per capita income. Model 2 adjusted by Model 1 plus smoking status, alcohol consumption, physical activity level and total energy intake.
Diet quality and carotid intima-media thickness changes
After multivariate adjustments, each 10-point increase in the CHDI score was associated with –0·002 mm (95 % CI –0·005, –0·001) in the cIMT over the median follow-up time of 8·0 years (Table 4). Notably, we observed an inverse association in the interaction terms between the CHDI score and time, suggesting that the diet’s impact on cIMT diminishes each year throughout the follow-up period. When evaluating the association between each CHDI component with cIMT across the follow-up period, we observed that higher scores in the whole-grain cereals and nuts components (indicating higher consumption of these foods) were inversely associated with cIMT over time. Conversely, higher scores in the SSB, processed meat and ultra-processed foods (indicating lower consumption of these foods) were inversely associated with cIMT over time (online Supplementary Table S5). Online Supplementary Fig. S1 demonstrates that individuals in the third tertile of the CHDI had a smaller increase in cIMT compared with those in the first tertile, as they showed a reduced increase of −0·013 mm (95 % CI −0·019, −0·007) in cIMT over the follow-up period in the adjusted models.
Table 4. Linear mixed-effects regressions between each 10-point increase in the Cardiovascular Health Diet Index score with longitudinal carotid intima-media thickness (cIMT). ELSA-Brasil, 2008–2010 to 2017–2019
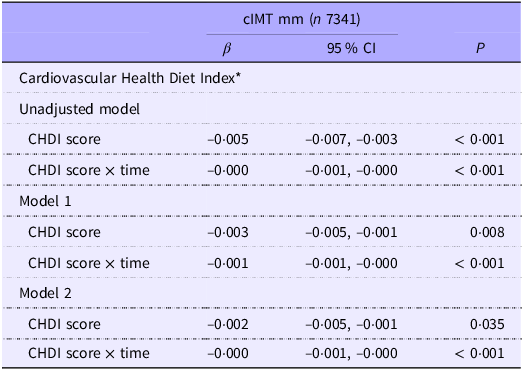
CHDI, Cardiovascular Health Diet Index.
* As each 10-point increase. Values are regression coefficients (β) 95 % CI based on linear mixed models and reflect differences in cIMT averaged across a median follow-up of 8·2 years per 10 points higher score in the diet quality scores. cIMT, carotid intima-media thickness. Model 1: unadjusted. Model 1: age, sex, self-reported race and per capita income. Model 2: model 1 plus smoking status, alcohol consumption, physical activity level, total energy intake and presence of dyslipidaemia and statin use.
Additional analyses
For the HEI-2015, the baseline score ranged from 25·8 to 96·5, with a mean score of 60·2 points for the entire population, and ranged from 26·4 to 94·6 for the sub-cohort sample with a mean score of 59·2 points. The HEI-2015 was correlated with the CHDI score (r 0·66, P < 0·001). No associations were observed when using the HEI-2015 score with CAC incidence or progression either in the unadjusted or in the fully adjusted models (online Supplementary Tables S6 and S7). In the unadjusted model, a 10-point increase in the HEI-2015 score was associated with –0·005 mm (95 % CI –0·008, –0·002) in the cIMT over the median follow-up time of 8·0 years. However, these results did not persist after adjusting for the covariables (online Supplementary Table S8).
Discussion
In this large Brazilian cohort study with middle-aged individuals without overt CVD, higher diet quality – evaluated through the CHDI – was prospectively associated with a slight decrease in cIMT values. Furthermore, higher consumption of whole-grain cereals and nuts led to a reduction in cIMT, while lower consumption of processed meat, SSB and ultra-processed foods also contributed to a reduction in this outcome after an 8-year follow-up period. However, no association was observed between the diet quality score and CAC incidence and progression after 4 years of follow-up.
The prospective association between diet quality scores and subclinical atherosclerosis evaluated throughout cIMT and CAC score has been hardly studied. Maddock et al. (Reference Maddock, Ziauddeen and Ambrosini37) observed that long-term adherence (24–28-year period for each individual) to the Dietary Approaches to Stop Hypertension score was associated with decreasing cIMT in participants from a British birth cohort study. Petersen et al. (Reference Petersen, Keogh and Lister38) observed that higher scores in the adapted Healthy Eating Index were inversely associated with cIMT values after 2 years of follow-up period in eighty-seven individuals diagnosed with diabetes. These results, in alignment with our findings, suggest that higher diet quality might slow down the increase in cIMT over time.
Consistent with our lack of association between the diet quality scores and CAC, Richardson et al. (Reference Richardson, Basu and Chien39) observed that a Mediterranean-style dietary pattern score was not associated with CAC in a case–control study with individuals from the USA with and without type 1 diabetes. In alignment, the same authors found no association in a prospective analysis between the MedDiet score and Dietary Approaches to Stop Hypertension score with CAC progression(Reference Richardson, Basu and Chien40). However, Gao et al. (Reference Gao, Hao and Zhang41), using data from the CARDIA study, observed that individuals with animal-based low-carbohydrate diet score was associated with higher risk of CAC progression after a follow-up period of 8·3 years.
In previous cross-sectional studies, no association was observed between diet quality scores and cIMT or CAC. Recio-Rodriguez et al. (Reference Recio-Rodriguez, Garcia-Yu and Alonso-Dominguez42) found no association between higher scores in the diet quality score – a diet score that includes eighteen food groups and can range from 18 to 54 points – with cIMT in middle-aged Spanish adults with intermediate cardiovascular risk. Furthermore, Hoebeeck et al. (Reference Hoebeeck, Rietzschel and Langlois43) found no statistical significance between an overall dietary score (composed of the sum of the dietary quality score, dietary diversity score and dietary equilibrium score) with cIMT and plaques in Belgian individuals aged 35–55 years. In the same direction, Gardener et al. (Reference Gardener, Wright and Cabral44) found no association between adherence to the Mediterranean diet assessed through the Mediterranean-style diet score with cIMT, in individuals from New York, USA, although they observed a slight decrease in the carotid plaque. In a cross-sectional analysis with data from the Multi-Ethnic Study of Atherosclerosis (MESA) study, Nettleton et al. (Reference Nettleton, Schulze and Jiang45) found an inverse association between higher scores in the Healthy Dietary Pattern score and cIMT, but the association did not withstand after adjustments for waist circumference. According to Nettleton et al. (Reference Nettleton, Schulze and Jiang45), no association was observed between the Healthy Dietary Pattern and CAC in participants from the MESA study. However, in a study with 172 individuals from Canada diagnosed with hypercholesterolaemia, lower adapted Healthy Eating Index scores were associated with CAC presence, after controlling for multiple factors(Reference Drouin-Chartier, Tremblay and Godbout46).
Notably, in our study, the consumption of whole grains and nuts emerged as influential factors in reducing cIMT. Plant-based diets are posited as pathways to prevent and reduce CVD(Reference Martínez-González, Gea and Ruiz-Canela47,Reference Cacau, Benseñor and Goulart48) . According to Mellen et al. (Reference Mellen, Liese and Tooze49), higher whole-grain intake was prospectively associated with lower cIMT values in 1178 individuals from the Insulin Resistance Atherosclerosis Study (IRAS), after 5 years of follow-up. Accordingly, Steffen et al. (Reference Steffen, Jacobs and Stevens50) observed that higher intake of whole grain was associated with a lower risk of incidence of coronary artery disease and total mortality after an 11-year follow-up among 11 940 middle-aged participants from the Atherosclerosis Risk in Communities (ARIC) Study. In a randomised clinical trial with 175 subjects from the PREDIMED study (Prevención con Dieta Mediterránea), Sala-Vila et al. (Reference Sala-Vila, Romero-Mamani and Gilabert51) observed that those group who followed a Mediterranean diet supplemented with 30 g/d of mixed nuts (15 g walnuts, 7·5 g hazelnuts and 7·5 g almonds) had a regression in intima-media thickness and delayed the progression of intima-media thickness and carotid plaque, after a mean of 2·4 years, as compared with those who followed a low-fat diet for the same period.
On the other hand, the adoption of dietary patterns characterised by higher intakes of processed meat, SSB and ultra-processed foods contributed to an unfavourable increase in cIMT over time as observed in our study. The negative effects of ultra-processed foods on cardiovascular health have been widely debated, and systematic reviews with meta-analyses suggest that ultra-processed food intake is associated with risk for CVD(Reference Pagliai, Dinu and Madarena52,Reference Lane, Davis and Beattie53) . Riccardi et al. (Reference Riccardi, Giosuè and Calabrese54) in a recent review reported that meta-analyses of prospective observational studies observed that higher intake of processed meat and SSB has been associated with increasing risk of carotid heart disease incidence.
Several factors may contribute to the differences observed in studies utilising various diet quality scores. Many of the mentioned studies employed general and non-specific diet quality scores when assessing their association with subclinical atherosclerosis, and a majority of them limited their analysis to cross-sectional designs. In our study, we adopted a diet quality score specifically tailored for the Brazilian population, which is rooted in the recommendations for a heart-healthy diet as endorsed by the AHA. This diet quality score incorporates foods that hold significance in the Brazilian food culture, such as red meat and beans. We also integrated ultra-processed foods as a component of this index, recognising their link to CVD risk(Reference Pagliai, Dinu and Madarena52,Reference Nilson, Ferrari and Louzada55) . Our findings revealed a prospective association between the CHDI score and subclinical atherosclerosis, as assessed by cIMT. However, when we examined the relationship between the HEI-2015 and the same outcome, we did not identify a statistically significant association. Hence, it appears that a diet quality score specifically designed to target cardiovascular health may offer more valuable insights when evaluating cardiovascular outcomes.
Despite this, we were unable to identify a significant relationship between diet quality scores and CAC. However, it’s worth noting that our findings align with existing literature(Reference Richardson, Basu and Chien39,Reference Richardson, Basu and Chien40,Reference Nettleton, Schulze and Jiang45) . While CAC and cIMT are widely recognised tools for detecting subclinical atherosclerosis and assessing CVD risk, some important points should be addressed. For instance, the correlation between these two diagnostic tools appears to be weak and one possible explanation is that CAC may represent a more advanced stage of vascular alterations(Reference Oei, Vliegenthart and Hak56). Lester et al. (Reference Lester, Eleid and Khandheria57) have shown that individuals without clinically apparent atherosclerosis, but with a CAC score of zero, still exhibit atherosclerotic changes as revealed by cIMT assessments. This suggests that cIMT might be more sensitive than CAC in detecting subclinical atherosclerosis, particularly among middle-aged adults. Nonetheless, the lack of association with CAC in our study may be partly attributed to the relatively short follow-up period, which was limited to 4 years, in contrast to the average 8-year follow-up period for cIMT assessments. Future research efforts should explore the relationship between CHDI and CAC using longer follow-up periods to provide a more comprehensive understanding of these associations.
Our study addressed the prospective association between a diet quality score and subclinical atherosclerosis – assessed using the CAC score and cIMT – in a large sample of Brazilian individuals without overt CVD. Besides that, the ELSA-Brasil followed a strict protocol when measuring the cIMT and the CAC score. We used a validated diet quality score that considers the Brazilian food culture context and included ultra-processed foods metric in its components to evaluate diet quality among the participants of the ELSA-Brasil study. In addition, the follow-up period can be considered a strength since the ELSA-Brasil is one the largest cohort studies in Brazil.
However, some limitations may be pointed out as well. Food consumption was assessed using an FFQ, an instrument that, despite being one of the most commonly used methods in nutritional epidemiological studies, still features some limitations, such as the finitude of its food list and dietary misreporting bias. Although the ELSA-Brasil is a multicentre cohort study, it is not representative of the entire Brazilian population. However, the ELSA-Brasil sample and design allowed the inclusion of an ethnic and social diversity that is observed in populations who live in Brazilian large cities. Thus, our results can be extended to urban centres with similar characteristics.
Conclusion
In conclusion, this study conducted in a large Brazilian cohort of middle-aged individuals, free of apparent CVD, underscores the correlation between diet quality – assessed throughout the CHDI score – and a prospective decrease in the rate of increase in cIMT values. Notably, consumption of whole grains and nuts emerged as influential factors in reducing cIMT, while the adoption of dietary patterns characterised by higher intakes of processed meat, SSB and ultra-processed foods contributed to a favourable increase in cIMT over time. Nonetheless, no discernible link was seen between the diet quality and the incidence of CAC after a 4-year follow-up period. More prospective studies with large period designs are needed to explore the nuanced interactions between diet quality and markers of subclinical atherosclerosis.
Supplementary material
For supplementary material/s referred to in this article, please visit https://doi.org/10.1017/S0007114524002836.
Acknowledgements
The ELSA-Brasil baseline study was supported by the Brazilian Ministry of Health (Science and Technology Department) and the Brazilian Ministry of Science and Technology and National Research Council (grants 01 06 0010.00 RS, 01 06 0212.00 BA, 01 06 0300.00 ES, 01 06 0278.00 MG, 01 06 0115.00 SP and 01 06 0071.00 RJ). The research centre of São Paulo was also supported by São Paulo Research Foundation (FAPESP) (grant no. 2011/12256–4). LTC received a doctoral scholarship from the FAPESP (grant no. 2019/13424–0). No funding agencies had a role in the study design, data collection, analysis, decision to publish or preparation of the article.
L. T. C. conducted the conceptualisation, data curation, formal analysis and interpretation of the data and produced the first draft of this manuscript. M. A. A. contributed to the formal analysis. I. S. S., G. G., M. S. B., P. A. L. and I. M. B. revised the manuscript due to the intellectual content. D. M. M. contributed to conceptualisation and supervised L. T. C. All authors critically revised and approved the final version to be published.
The authors declare no conflict of interest.








