AIMS AND METHOD
To evaluate the first 2 years of a new adolescent unit.
RESULTS
One-hundred and eighteen cases were admitted, with a broad range of diagnoses. Median length of stay was 33 days and 82% of admissions were urgent, of which 70% were admitted on the day of referral. A later study of 27 consecutive cases showed a mean improvement of 25% in the Children's Global Assessment Scale and 40% in the Child and Adolescent version of the Health of the Nation Outcome Scales scores.
CLINICAL IMPLICATIONS
It is possible to provide an in-patient service for adolescents that includes all-hours emergency access, as well as catering for the full range of severe mental illness and a wide variation in length of stay.
Fourteen years ago the Bridges Over Troubled Waters report (Health Advisory Service, 1986) identified serious weaknesses in in-patient services for adolescents. Since then further reports have repeated the themes of fragmentation and underplanning (Reference Kurtz, Thornes and WolkindKurtz et al, 1994; Health Advisory Service, 1995; House of Commons Health Committee, 1997). Recently there has been a focus on the inadequacy of emergency provision (Audit Commission, 1999; Young Minds, 2000).
In addressing some of the traditional weaknesses in in-patient care we identified the following as key objectives of a new service: accessibility, flexibility and efficiency.
Accessibility
We identified three main barriers to an accessible service.
Overly restrictive admissions criteria
Box 1 lists restriction criteria encountered in clinical practice by the authors. Although some restrictions might be justified as relative contraindications to admission, the overzealous application of such exclusions can readily create an inaccessible service that denies hospital care to those most in need.
Box 1. Some reasons for not admitting a patient to an adolescent unit encountered by the authors in clinical practice
| Already detained under the Mental Health Act |
| Need for medication |
| Diagnosis of psychotic illness |
| No fixed place of residence |
| Learning disability |
| Other disabilities (e.g. profoundly deaf) |
| Young person not willing to engage in therapy |
| Diagnosis of pervasive developmental disorder |
| Drug use |
| History of violence |
| Fire setting |
| Acting out behaviour |
| Previously suspended from the unit |
Over-reliance on reassessment
The insistence on reassessing referred cases before agreeing admission is commonly encountered. The importance of a careful assessment by the admitting unit has been argued (Reference Bruggen, Byng-Hall and PittaikensBruggen et al, 1973; Reference WellsWells, 1989; Reference Steinberg, Rutter, Taylor and HersovSteinberg, 1994), with stress on the need to clarify goals and establish agreement. Such objectives may be laudable, but it remains an untested assumption that they can only be achieved by way of face to face assessment before admission. There is no firm evidence that such reassessments make any difference to outcome and they inevitably create a delay to admission. Furthermore, reassessment risks duplicating work already undertaken by out-patient clinicians. The anomalous situation may arise where a psychiatric trainee is called upon to repeat the assessment of a more experienced out-patient colleague. Such procedures can easily cause frustration for referrers, patients and families.
Lack of emergency admission service
It has been asserted that emergencies requiring immediate admission to a hospital ward are relatively rare (Reference Steinberg, Hsu and HersenSteinberg, 1989). In the experience of the authors such emergencies are not rare. A survey of health service commissioners and out-patient clinicians prior to the opening of Snowsfields identified the lack of emergency beds for adolescents as a frequent complaint, an observation supported by subsequent surveys (Young Minds, 2000; Reference Worrall and O'HERLIHYWorrall & O'Herlihy, 2001). At the time of planning the Snowsfields service, the authors were not aware of any NHS adolescent unit in the country offering a 24-hour, 7 day a week emergency admission service. More recently, the National In-patient Child and Adolescent Psychiatry Study (NICAPS) has indicated that two-thirds of all child and adolescent in-patient units provide no emergency admission service at all (NICAPS Research Team, personal communication, 2001). The definition of an emergency admission used in the survey was admission within 24 hours, so even among the third of units with a service it is unclear how many are able to provide out-of-hours admission. Furthermore, the survey did not ask how many beds were available for emergencies, so it may be that many units offer only a limited service.
Flexibility
Lack of flexibility was identified as a key problem in Bridges Over Troubled Waters (Health Advisory Service, 1986). An example of inflexible practice might include an over reliance on a narrow therapeutic ideology, with all patients being expected to take part in very similar treatment packages. Such an approach can easily feed into a restrictive admissions policy. Other forms of inflexible practice include the use of fixed time frames for assessment or treatment. This type of thinking often occurs in debates regarding the merits of long-stay v. short-stay units, missing the point that adolescents with severe mental health problems do not conveniently aggregate into groups requiring brief or long admissions. Our plan was to allow for flexible treatment planning around individual need.
Efficiency
Length of stay
Length of stay was frequently raised as an area of concern by health service commissioners when consulted about the new service. In addressing the problem we identified the following as likely contributing factors: bureaucratic inefficiencies, therapeutic perfectionism and the lack of adequate support and placement opportunities post-discharge. Bureaucratic inefficiencies include problems such as an overly long decision-making cycle. If the main clinical review for a patient occurs as infrequently as once a month then there is a tendency for all admissions to last for many months, irrespective of need. Therapeutic perfectionism applies when a unit aims to resolve all of the presenting problems before deciding that a young person is ready for discharge. This may be unrealistic, as in many cases of emotional/behavioural disturbance, where an emphasis on short-term crisis management and a planned return to local services with ‘managed risk’ is more realistic than a long-term attempt at personality modification.
The lack of adequate support and placement opportunities post-discharge is a frequent complaint of in-patient providers and undoubtedly contributes to unnecessarily prolonged in-patient stays. Our intention was to design a service that could anticipate such problems at an early stage and work flexibly with outside agencies to try to minimise the impact of these difficulties.
Bed occupancy
A key objective of the new service was to maintain bed occupancy at an efficient level, while preserving some unused capacity for urgent admissions.
Brief description of the service
Snowsfields is located within Guy's Hospital, London. Staffing levels are indicated in Box 2. Ten in-patient beds and four day patient places are provided. Nine of the beds are contracted to commissioning health authorities in the central London area, with one further bed contracted to a health authority just outside of London. The total population covered is approximately 2 million. The contracts are for fixed numbers of beds, in other words the purchasers pay for the availability of the bed, regardless of occupancy.
Box 2. Staffing levels, expressed as whole time equivalents
| 1 consultant adolescent psychiatrist |
| 1 clinical nurse manager |
| Nursing cover of four staff per early shift, four per late shift and three per night shift |
| 1 specialist registrar |
| 1 senior house officer |
| 1 psychologist |
| 1 occupational therapist |
| 1 social worker |
| 2 teachers |
Patients can be admitted after their 12th birthday, up until their 18th birthday. The key inclusion criterion is the presence of a severe mental health problem requiring hospital admission. The only absolute exclusion is for patients with a level of dangerousness requiring security beyond that which can be provided on the unit (i.e. at the level of an adult intensive care unit). Young people with learning disabilities, drug problems or pervasive developmental disorders and those who are homeless or who require detention under the Mental Health Act are not excluded from the service.
A 24-hour, 7 day a week emergency admission service is offered. It is a requirement that all referrals must be channelled through an out-patient psychiatric team. Referrals from adult mental health teams are welcomed.
A management round and a multi-disciplinary wardround are held weekly. All patients on the unit are discussed at each meeting.
A broad range of treatments are provided, including medication, cognitive—behavioural therapy, group work, psychoeducational family work, systemic family work and art psychotherapy. Treatments are flexibly delivered according to the individual needs of the patient. It is unit policy to attempt to hold Care Programme Approach meetings for all patients. The young person and family are routinely invited to these meetings, as well as all outside professionals with an involvement in the case. These meetings are an important forum for planning discharge and after-care with referrers.
Results
During the first 2 years of operation (April 1998 to April 2000) 118 cases were admitted as in-patients (a mean of 1.1 per week). Fifty-eight per cent of admissions were female and the mean age was 15.9 years. Thirty-five per cent of admissions were detained under the Mental Health Act at some point during their stay. Mean bed occupancy was 88%. Mean length of stay was 51 days. However, owing to the very skewed distribution (Fig. 1) a better indication of central tendency is provided by the median of 33 days. At the extremes, 23 cases stayed on the unit for less than 10 days and two cases remained on the unit for nearly a year.
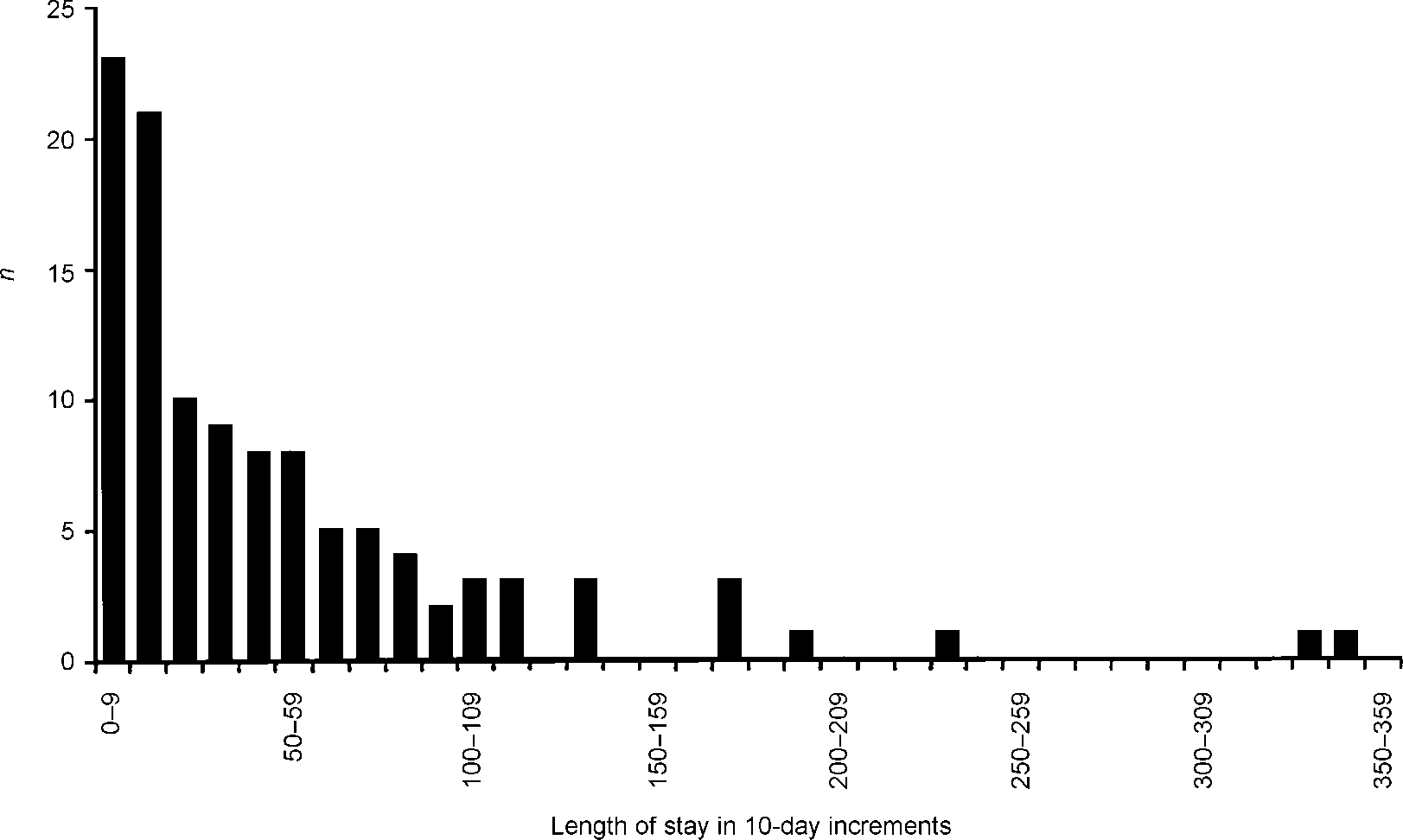
Fig. 1 Length of stay for adolescent in-patient admissions (n=118)
There were 29 episodes of day patient care during the audit period, with a mean length of stay of 28 days. Most of these episodes were former in-patients who were offered day patient attendance as a step towards reintegration into the community. However, for four cases it was possible to avoid admission altogether.
Table 1 shows the breakdown of all 122 cases (in-patients and day patients) by ICD-10 diagnosis (World Health Organization, 1992). In addition to the main diagnosis, 16 cases (13.1%) had a moderate learning disability (one case borderline severe learning disability). It is likely that an even greater number of cases would fall into the category of mild learning disability, but confirmatory evidence was often lacking for those in whom such an impairment might be suspected clinically.
Table 1. ICD-10 (World Health Organization, 1992) psychiatric diagnoses
| ICD—10 code | Frequency | Per cent | |
|---|---|---|---|
| Drug-induced disorders | F1x | 1 | 0.8 |
| Schizophrenia-like | F12.50 | 1 | 0.8 |
| psychotic disorder owing to use of cannabinoids | |||
| Schizophrenic disorders | F2x | 40 | 32.8 |
| Schizophrenia | F20.x | 31 | 25.4 |
| Schizotypal disorder | F21 | 1 | 0.8 |
| Delusional disorder | F22.x | 1 | 0.8 |
| Acute schizophrenia-like | F23.x | 6 | 4.9 |
| Schizoaffective disorder | F25.x | 1 | 0.8 |
| Mood disorders | F3x | 27 | 22.1 |
| Manic disorder | F30.x | 6 | 4.9 |
| Bipolar disorder | F31.x | 10 | 8.2 |
| Depressive disorder | F32.x | 11 | 9.0 |
| Neurotic disorders | F4x | 21 | 17.2 |
| Agoraphobia | F40.x | 1 | 0.8 |
| Panic disorder | F41.x | 1 | 0.8 |
| Obsessive—compulsive disorder | F42.x | 2 | 1.6 |
| Stress reactions | F43.x | 15 | 12.3 |
| Somatisation disorder | F45.x | 2 | 1.6 |
| Eating disorders | F5x | 2 | 1.6 |
| Atypical anorexia nervosa | F50.1 | 2 | 1.6 |
| Personality disorders | F6x | 2 | 1.6 |
| Emotionally unstable personality disorder, borderline type | F60.31 | 2 | 1.6 |
| Pervasive developmental disorders | F8x | 2 | 1.6 |
| Childhood autism | F84.0 | 1 | 0.8 |
| Asperger's syndrome | F84.5 | 1 | 0.8 |
| Disorders in childhood | F9x | 7 | 5.7 |
| Hyperkinetic disorder | F90.x | 1 | 0.8 |
| Conduct disorder | F91.x | 1 | 0.8 |
| Mixed disorder of conduct and emotions | F92.x | 5 | 4.1 |
| No psychiatric diagnosis | 20 | 16.4 |
Of all referrals resulting in admission to the unit just over 82% were urgent, of which 70% were admitted on the same day as referral (i.e. no overnight wait and these were usually admitted within a few hours of the referral). Of those urgent admissions that were delayed the large majority (82%) were for reasons beyond the control of the unit. Reasons for delay included delay in arranging detention under the Mental Health Act in the community, cases not judged as medically fit for transfer and reluctance of family members to agree to admission. Where admission was delayed owing to lack of beds, patients were either admitted to another ward or held in the community (with the agreement of the referrer) and transferred as soon as a bed became available.
The vast majority of cases were discharged home to carers (97). Small numbers went on to alternative placements, which included other adolescent units (five), adult psychiatric wards (four), foster care (three), residential care (two) and independent living (five). Of the five cases going on to other adolescent units, one went to a private sector unit because of lack of beds in the trust. Two went on to therapeutic community style adolescent units and two went to a private sector adolescent rehabilitation unit.
Outcomes were rated by the authors on a consensus basis, using a simple clinical scale based on a scale used in the Core Data Set of the Association of Child Psychology and Psychiatry (Reference Berger, Hill and SeinBerger et al, 1993). No cases were rated as having become clinically worse, 11.5% were rated as ‘no change’, 16.8% ‘some improvement’, 46.9% ‘considerable improvement’ and 24.8% were rated as ‘problems resolved’. In addition, a more detailed study of outcome was undertaken after the main audit period, using data from 27 consecutive cases. For this study the Children's Global Assessment Scale (C-GAS; Reference Shaffer, Gould and BrasicShaffer et al, 1983) and the Child and Adolescent version of the Health of the Nation Outcome Scales (HoNOSCA; Reference Gowers, Harrington and WhittonGowers et al, 1999) were added. Both scales were consensus rated by the junior doctor and consultant. These results are shown in Table 2. A mean improvement of 24.5% was achieved for C-GAS and 39.5% for HoNOSCA.
Table 2. Outcome measures for 27 consecutive cases
| Outcome measure | C-GAS | HoNOSCA |
|---|---|---|
| Mean admission score | 49.0 | 12.9 |
| Mean discharge score | 61.0 | 7.8 |
| Percentage improvement | 24.5 | 39.5 |
Discussion
The opening of a new service has allowed many of the conventional assumptions regarding the provision of inpatient psychiatric care for adolescents to be reconsidered. The results from the first 2 years of the operation of Snowsfields Adolescent Unit indicate that this new model, providing accessible flexible and efficient care for young people, can be successful.
In our experience contracts with local health authorities with specified bed numbers is a helpful way of providing an adolescent in-patient service. This arrangement encourages a sense of responsibility to a defined population, fosters a comprehensive approach to provision and provides a welcome transparency for referrers. The alternative system of taking cases on an ad hoc basis, by way of out-of-area transfers, may tend to reinforce a selective approach to admissions and distances the unit from the community it should be serving. Contracting also assists in matching provision to real need, as the size and origin of excess demand is easily identified. Furthermore, it assists the providing unit in developing a genuinely collaborative relationship with commissioners and referrers over time.
Our attempt to avoid the over-restrictive admissions policies commonly encountered in adolescent in-patient provision has been successful. It has proved possible to cater for a broad range of mental disorder in one general purpose unit. The one area that the service has been unable to cater for is that of dangerous patients requiring a secure environment. Nonetheless, the service has been able to cope with significant levels of challenging behaviour (including some cases of violent behaviour, fire setting and drug use) and has coped with a high level of patients detained under the Mental Health Act. Cases exceeding the threshold for safe management have been those that could not be prevented from absconding by the use of a single locked door or those requiring greater than one-to-one nursing for extended periods. Such cases have been managed either by soliciting the assistance of local adult intensive care facilities or by seeking referral to secure adolescent provision. Secure provision for adolescents is noticeably deficient and should be a priority for future commissioning.
Of particular note is the provision of an all-hours emergency admission service. This has proved to be a perfectly viable model for delivering care, helping to address a badly unmet need for the adolescent population. Dispensing with the mandatory reassessment of referred cases, a corollary of any workable emergency admission service, has not proved to be problematic and has been popular with referrers.
The relatively high proportion of cases with moderate learning difficulties underlines the viability of a service aimed at inclusion rather than exclusion. Young people with learning disabilities are an important and potentially vulnerable group — there is no justification for excluding them from age appropriate in-patient services.
The bed occupancy achieved allowed for efficient use of the beds while yielding enough spare capacity to sustain an emergency admission service. The Snowsfields experience of providing for local populations in central London indicates that two beds are probably sufficient to meet the in-patient needs of one inner-London borough (population approximately 250 000), assuming a median length of stay of just over 1 month. However, our experience indicates that need can vary considerably, even within the inner-London area. In our view bed norms are not meaningful for adolescent units unless explicit reference is made to the expected length of stay.
The mean length of stay on Snowsfields is roughly half that derived from a survey of general child and adolescent psychiatric units in England and Wales (NICAPS research team, personal communication, 2001). However, we do not argue that brief admission should be regarded as an end in itself. As we have shown, it is perfectly viable to cater for a wide variation in length of stay within the same unit. It is an error to confuse emergency access with length of stay. Developing short-stay services alongside existing units will only serve to increase fragmentation and inefficiency. Emphasis should be placed on reforming existing provision to encourage greater flexibility and inclusiveness.
Declaration of interest
R.C. has admitting rights at the Nightingale Young Person's Unit, a private unit offering in-patient care for young people with mental illness.








eLetters
No eLetters have been published for this article.