Introduction
Low- and middle-income countries (LMICs) bear a disproportionate burden of the world's HIV infections, with over 85% of the world's 35 million HIV cases located in LMICs (UN Joint Programme on HIV/AIDS, 2014). Studies across multiple settings have consistently observed that people living with HIV (PLWH) experience greater psychological distress, such as depression and anxiety, as compared with the general population (Bing et al. Reference Bing, Burnam, Longshore, Fleishman, Sherbourne, London, Turner, Eggan, Beckman, Vitiello, Morton, Orlando, Bozzette, Ortiz-Barron and Shapiro2001; Ciesla & Roberts, Reference Ciesla and Roberts2001). Evidence from LMICs, though limited, has confirmed high rates of mental disorders and psychological distress among PLWH (Breuer et al. Reference Breuer, Myer, Struthers and Joska2011; Chibanda et al. Reference Chibanda, Benjamin, Weiss and Abas2014). Mental disorders in LMICs must be addressed due to their impact on the lives of PLWH, as well as HIV-related outcomes at an individual and population level (Hartzell et al. Reference Hartzell, Janke and Weintrob2008).
Mental disorders and psychological distress not only compromise overall well-being and quality of life among PLWH (Bing et al. Reference Bing, Hays, Jacobson, Chen, Gange, Kass, Chmiel and Zucconi2000), but also impact individuals’ ability to engage effectively with HIV care, including their adherence to antiretroviral therapy (ART) (Collins et al. Reference Collins, Holman, Freeman and Patel2006; Mayston et al. Reference Mayston, Kinyanda, Chishinga, Prince and Patel2012; Uthman et al. Reference Uthman, Magidson, Safren and Nachega2014). The ability to halt disease progression and achieve full viral suppression, which requires proper care engagement, is a primary predictor of HIV infectiousness (Cohen et al. Reference Cohen, Chen, Mccauley, Gamble, Hosseinipour, Kumarasamy, Hakim, Kumwenda, Grinsztejn, Pilotto, Godbole, Mehendale, Chariyalertsak, Santos, Mayer, Hoffman, Eshleman, Piwowar-Manning, Wang, Makhema, Mills, De Bruyn, Sanne, Eron, Gallant, Havlir, Swindells, Ribaudo, Elharrar, Burns, Taha, Nielsen-Saines, Celentano, Essex, Fleming and Team2011). Poor HIV care engagement attributable to unaddressed mental health needs among PLWH may thus hamper proposed efforts to use ‘treatment as prevention’ to curb the spread of the HIV epidemic (Sikkema et al. Reference Sikkema, Watt, Drabkin, Meade, Hansen and Pence2010; Gupta et al. Reference Gupta, Williams and Montaner2014). Additionally, mental disorders and psychological distress may be associated with HIV risk behaviors such as substance abuse, multiple sexual partners and unprotected sexual intercourse (Crepaz & Marks, Reference Crepaz and Marks2001), further contributing to the forward transmission of HIV (Senn et al. Reference Senn, Carey and Vanable2010). Taken together, addressing mental health among PLWH appears to be a critical component of HIV treatment and prevention, and should be considered as part of population-level approaches to prevent HIV transmission, particularly in LMICs where the burden of HIV and its associated morbidities is high.
An emerging body of evidence, mostly from high-income settings, suggests that psychological interventions, primarily focused on treating depression and anxiety, can improve the mental health of PLWH (Crepaz et al. Reference Crepaz, Passin, Herbst, Rama, Malow, Purcell and Wolitski2008; Brown & Vanable, Reference Brown and Vanable2011; Clucas et al. Reference Clucas, Sibley, Harding, Liu, Catalan and Sherr2011; Harding et al. Reference Harding, Liu, Catalan and Sherr2011; Sherr et al. Reference Sherr, Clucas, Harding, Sibley and Catalan2011; Seedat, Reference Seedat2012; Spies et al. Reference Spies, Asmal and Seedat2013; Wu & Li, Reference Wu and Li2013). Among the various treatment modalities, cognitive-behavioral interventions (CBIs) have received the most attention, with skills training and stress management CBIs that include 10 or more sessions demonstrating the greatest improvement in mental health symptoms. These interventions have been found to be equally if not more effective than pharmacological treatments (Clucas et al. Reference Clucas, Sibley, Harding, Liu, Catalan and Sherr2011; Spies et al. Reference Spies, Asmal and Seedat2013), though it has been suggested that pharmacological management can be beneficial as an adjunct treatment or combined with psychological approaches (Sherr et al. Reference Sherr, Clucas, Harding, Sibley and Catalan2011). In addition, CBIs have been found not only to improve mental health symptoms in PLWH, but also to impact HIV-related clinical outcomes, including CD4 counts (Crepaz et al. Reference Crepaz, Passin, Herbst, Rama, Malow, Purcell and Wolitski2008). Furthermore, a limited number of intervention studies have begun to examine the impact of mental health treatment on care engagement and risk behaviors in PLWH. For example, depression treatment has been found to enhance ART adherence (Sin & DiMatteo, Reference Sin and DiMatteo2014), and coping interventions to reduce traumatic stress have been found to decrease substance use (Meade et al. Reference Meade, Drabkin, Hansen, Wilson, Kochman and Sikkema2010) and sexual risk behaviors (Sikkema et al. Reference Sikkema, Wilson, Hansen, Kochman, Neufeld, Ghebremichael and Kershaw2008). There is further evidence that psychological interventions can be delivered in community settings, which has the potential for broader reach (Wu & Li, Reference Wu and Li2013). Intervention studies published subsequent to existing reviews suggest an emerging focus on aging populations (Heckman et al. Reference Heckman, Heckman, Anderson, Lovejoy, Mohr, Sutton, Bianco and Gau2013), increased emphasis on treating traumatic stress and post-traumatic stress disorder (PTSD) (Pacella et al. Reference Pacella, Armelie, Boarts, Wagner, Jones, Feeny and Delahanty2012; Sikkema et al. Reference Sikkema, Ranby, Meade, Hansen, Wilson and Kochman2013), and the use of telephone and web-based modalities (Hersch et al. Reference Hersch, Cook, Billings, Kaplan, Murray, Safren, Goforth and Spencer2013; Himelhoch et al. Reference Himelhoch, Medoff, Maxfield, Dihmes, Dixon, Robinson, Potts and Mohr2013; Drozd et al. Reference Drozd, Skeie, Kraft and Kvale2014), as well as alternative therapeutic approaches that draw on mindfulness (Gayner et al. Reference Gayner, Esplen, Deroche, Wong, Bishop, Kavanagh and Butler2012; Gonzalez-Garcia et al. Reference Gonzalez-Garcia, Ferrer, Borras, Munoz-Moreno, Miranda, Puig, Perez-Alvarez, Soler, Feliu-Soler, Clotet and Fumaz2014) and expressive writing paradigms (Ironson et al. Reference Ironson, O'cleirigh, Leserman, Stuetzle, Fordiani, Fletcher and Schneiderman2013; Carrico et al. Reference Carrico, Nation, Gomez, Sundberg, Dilworth, Johnson, Moskowitz and Rose2015).
Despite promising intervention efforts and related evidence, most of what has been appraised to date has emerged from high-income countries (HICs). Although previous reviews have included a limited number of studies from LMICs (Crepaz et al. Reference Crepaz, Passin, Herbst, Rama, Malow, Purcell and Wolitski2008; Clucas et al. Reference Clucas, Sibley, Harding, Liu, Catalan and Sherr2011; Harding et al. Reference Harding, Liu, Catalan and Sherr2011; Sherr et al. Reference Sherr, Clucas, Harding, Sibley and Catalan2011; Seedat, Reference Seedat2012; Spies et al. Reference Spies, Asmal and Seedat2013), thus far, no reviews have focused on interventions that broadly address mental health for PLWH in these unique settings. Despite the dual burdens of HIV and mental disorders in LMICs, and evidence of their synergistic negative effects, strategies to address the mental health needs of PLWH in LMICs have received only limited attention (Mayston et al. Reference Mayston, Kinyanda, Chishinga, Prince and Patel2012; Chibanda et al. Reference Chibanda, Benjamin, Weiss and Abas2014). Mental disorders in these settings often are untreated due to a lack of behavioral and pharmacological treatment opportunities (Kakuma et al. Reference Kakuma, Minas, Van Ginneken, Dal Poz, Desiraju, Morris, Saxena and Scheffler2011; WHO, 2001). This treatment gap has implications for both the well-being of PLWH as well as the effectiveness of national HIV treatment programs (Mayston et al. Reference Mayston, Kinyanda, Chishinga, Prince and Patel2012).
There is a need to take stock of existing efforts to respond to mental health distress challenges among PLWH in LMICs, so as to inform the development and scale up of appropriate mental health services in these countries. The goal of this review paper is to synthesize findings from mental health intervention trials for PLWH in LMICs. This information will extend our knowledge of mental health interventions for PLWH beyond those that have been developed and tested in HICs, and will illuminate avenues for future intervention development, testing, and delivery in LMIC settings where there is greatest need.
Methods
Inclusion criteria
Studies were included in this review if they met the following criteria:
-
(1) Described a trial evaluating a mental health intervention (e.g. CBT, coping, cognitive functioning, and pharmacological) among PLWH,
-
(2) Intervention was implemented in either a LMIC, as defined by the World Bank (The World Bank Group, 2015), or one of the emerging-economy Brazil, Russia, India, China, and South Africa (BRICS) countries (),
-
(3) Trial assessed at least one negative psychological state or disorder (e.g. depression and anxiety), and
-
(4) Outcomes were assessed pre- and post-intervention.
Exclusion criteria
Studies with a heterogeneous (HIV-positive and HIV-negative) sample were excluded if mental health outcomes were not presented separately for the HIV-positive population. Trials with only substance use outcomes were not included in this review. Systematic and non-systematic review articles, as well as studies unavailable in English, qualitative exploratory studies, and studies not published in a peer-reviewed journal were also excluded from this review.
Search strategy
PubMed, EMBASE, and PsychInfo were searched between 9 and 11 November 2014. Limits to time period were not applied to the search. Standardized search terms and key words related to the constructs of (a) HIV or AIDS, (b) mental health, (c) intervention, and (d) LMIC/BRICS were used in all databases. For example, within PubMed, terms used to capture the construct of mental health included the following: mental health, mental*, depress*, anxi*, trauma*, PTSD, psycholog*, coping, stress, and psychiat*. Search terms for LMIC/BRICS were derived from the World Bank's classification of low-income, lower-middle income, and upper-middle income economies (The World Bank Group, 2015). Conducting the search was a multi-step process. First, separate searches were conducted using HIV/AIDS, mental health, intervention, and LMIC/BRICs search terms, respectively. In the final step, results from these four separate searches were combined using ‘AND’ terms to capture manuscripts that possibly met study inclusion criteria. Where possible, studies with ‘orphan’ in the title were eliminated from the search using the term ‘HIV or AIDS not Orphan’ so as to more efficiently exclude studies focusing on HIV-impacted orphans who were not necessarily HIV-infected. Filters for the above constructs were applied within each database to restrict the search in the following ways:
-
(1) HIV or AIDS terms were restricted to title only,
-
(2) Mental health terms were restricted to title or abstract,
-
(3) Intervention terms were restricted to title only, and
-
(4) LMIC/BRICS terms were restricted to title, abstract or topic.
Study selection and data abstraction
A list of all titles and abstracts were considered independently by two researchers, eliminating those studies that did not appear to meet study inclusion criteria; the full study team then reached consensus on articles to be assessed for eligibility. The full text of all relevant articles were then independently reviewed by two researchers to determine inclusion, with >85% agreement between researchers. Discrepancies about the remaining studies were reconciled through discussion with the full study team. Data display matrices were used to extract data from included studies. Data extracted from studies were as follows: author, year, title, date of study, city/country, sample characteristics (age, sex, HIV-status, sample size of intervention and control conditions, mental health inclusion criteria), intervention characteristics (name, level, components, duration, deliverer), study design, evaluation design (control or comparison condition, follow-up, retention), outcome measures, and relevant findings.
Results
Search results
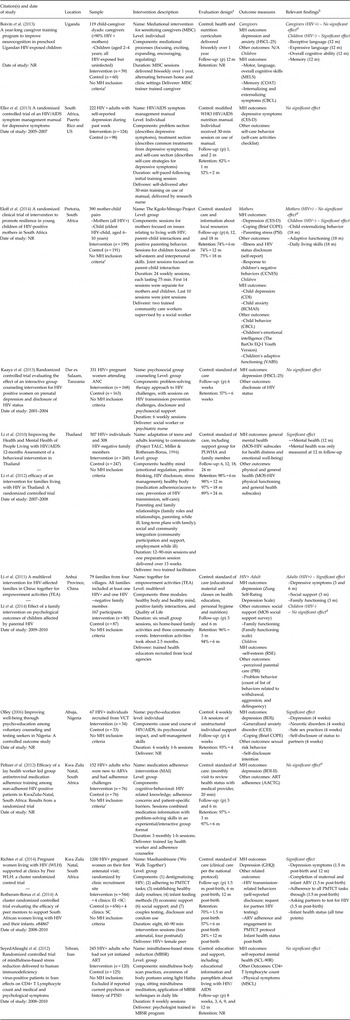
Initial database searches yielded 454 records, and 369 unique records remained after elimination of duplicates across databases. Screening of titles and abstracts resulted in 44 articles. The full text of these 44 articles was reviewed, which yielded 25 articles (describing 21 unique studies) that met the inclusion criteria for this review (see Fig. 1). One additional article was identified through examination of the reference lists of relevant systematic and non-systematic reviews (Field & Kruger, Reference Field and Kruger2008), for a total of 22 unique intervention studies included in this review. All included studies were published in peer-reviewed journals between 2000 and 2014. The summaries of the 10 randomized control trials (Table 1) and the 12 pilot or feasibility trials (Table 2) are presented separately.

Fig. 1. Study selection process.
Table 1. Randomized controlled trials
a Number of months (m) since baseline; (p) = immediate post assessment.
b No significant effect’ or ‘significant effect’ refer to between-condition effects.
c Indicates that mental health was a secondary outcome.
d No significant difference between conditions; both conditions improved.
NR, not reported; AACTG, Adult AIDS Clinical Trials Group adherence measure; BDI , Beck Depression Inventory; BDI-II, Beck Depression Inventory II; CBCL, Achenbach Child Behavior Checklist; CCBL, Child Behavior Checklist; CCEI, The Crown Crisp Experimental Index; CCNES, Coping with Children's Negative Emotions Scale; CDI, Child Depression Index; CES-D, Center for Epidemiologic Studies-Depression Scale; COAT, Color-Object Association Test; GHQ, General Health Questionnaire; HSCL-25, Hopkins Symptom Checklist; MELS, Mullen Early Learning Scales; MOS-HIV Medical Outcomes Study HIV Health Survey Instrument; MSCL, Medical Symptom Checklist; PBI, Parental Bonding Instrument; RCMAS, Revised Child Manifest Anxiety Scale; RSE, Rosenberg Self-Esteem Scale; SCL-90R, Symptom Checklist-90-Revised; VABS, Vineland Adaptive Behavior Scales.
Table 2. Pilot and feasibility studies
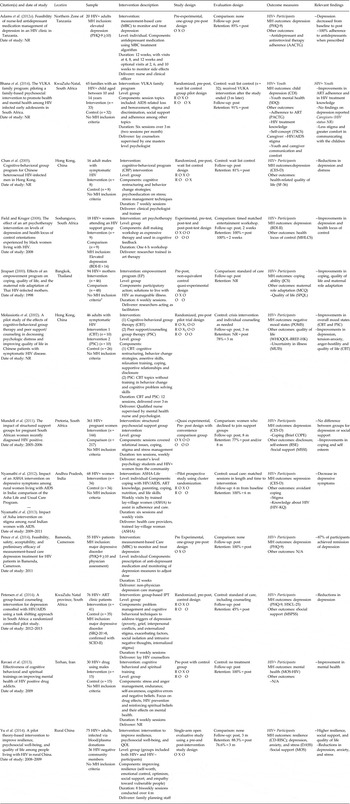
a Indicates that mental health was a secondary outcome.
MH, Mental Health; NR = not reported; AACTG, Adult AIDS Clinical Trial Groups Adherence Measure; BDI-II, Beck Depression Inventory; Brief COPE, abbreviated version of the COPE inventory; CBP, Cognitive Behavioral Program; CBT, Cognitive Behavioral Therapy; CES-D, Center for Epidemiologic Studies Depression Scale; CDI, Child Depression Inventory; CD-RISC, Connor-Davidson Resilience Scale; DASS, Depression, Anxiety, and Stress Scale; HIV-KQ, HIV Knowledge Questionnaire; HSCL-25, Hopkins Symptom Checklist; JCS, Jalowiec Coping Scale; MBC, Measurement Based Care; MCQ, Maternal Caregiving Questionnaire; MHLCS, Multidimensional Health Locus of Control Scale; MOS, Medical Outcomes Study; MOS-HIV, Medical Outcomes Study HIV Health Survey Instrument; MSSI, Multidimensional Social Support Inventory; MSPSS, Multidimensional Scale of Perceived Social Support; MUIS, Mishel Uncertainity in Illness Scale; PACTG, Pediatric AIDS Clinical Trial Groups Adherence Measure; PHQ-9, Patient Health Questionnaire-9; POMS, Profile of Mood States; PSC, Peer support/counseling group therapy; QOL, Quality of Life; RSE, Rosenberg Self-Esteem Scale; SCID-II, Structured Clinical Interview for DSM Disorders; SDQ, Strengths and Difficulties Questionnaire; SF-36, Medical Outcomes Study Short-Form 36; SPQL, Perceived Life Quality Index; SRQ-20, Self-Reporting Questionnaire; TSCS, Tennessee Self-Concept Scale; WHOQOL-BREF-HK, World Health Organization Quality of Life scale.
Randomized controlled trials (RCTs)
Study location
RCTs were conducted in Uganda (Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013), South Africa (Peltzer et al. Reference Peltzer, Ramlagan, Jones, Weiss, Fomundam and Chanetsa2012; Eller et al. Reference Eller, Kirksey, Nicholas, Corless, Holzemer, Wantland, Willard, Robinson, Hamilton, Sefcik, Moezzi, Mendez, Rosa and Human2013; Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014), Tanzania (Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013), Nigeria (Olley Reference Olley2006), China (Li et al. Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Ji, Wu and Xiao2014), Thailand (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012), and Iran (Seyed Alinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012).
Participants
A total of 2893 participants were reported across all trials, of which 1664 individuals participated in the experimental intervention condition. A median sample size of 233.5 at baseline (range 67–1200) was reported across all trials. All studies included HIV-positive participants, yet study samples were diverse. Four RCTs were designed for implementation within families (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Reference Li, Liang, Ji, Wu and Xiao2014; Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013; Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014); no studies included only child or adolescent participants. Of the six remaining RCTs, four were designed for implementation with HIV-positive men and women (Olley, Reference Olley2006; Peltzer et al. Reference Peltzer, Ramlagan, Jones, Weiss, Fomundam and Chanetsa2012; SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012; Eller et al. Reference Eller, Kirksey, Nicholas, Corless, Holzemer, Wantland, Willard, Robinson, Hamilton, Sefcik, Moezzi, Mendez, Rosa and Human2013), and two were for women only (Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014). Only one study had a specified mental health inclusion criterion, depressive symptoms (Eller et al. Reference Eller, Kirksey, Nicholas, Corless, Holzemer, Wantland, Willard, Robinson, Hamilton, Sefcik, Moezzi, Mendez, Rosa and Human2013). None of the RCTs utilized a mental disorder as inclusion criteria.
Study design
One RCT (Li et al. Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Ji, Wu and Xiao2014) randomized by cluster; all other RCTs randomized individual participants to the intervention or control condition. In all studies, outcomes were assessed post-intervention (median retention rate reported of 87.5%, range 57–98%), with most trials also reporting longer-term follow-up assessments between 2 and 18 months (median retention rate reported final follow-up of 82%, range 24–97%). (Note: outcomes in Tables 1 and 2 correspond to post-intervention measurements, unless otherwise noted).
Intervention content and delivery method
The interventions reported in these studies had diverse characteristics. Most interventions were designed to be implemented with groups (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Peltzer et al. Reference Peltzer, Ramlagan, Jones, Weiss, Fomundam and Chanetsa2012; SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012; Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013; Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014), and one group-based intervention was multilevel, including family and community components (Li et al. Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Ji, Wu and Xiao2014). Individual-based interventions (1–26 sessions) sought to address neurocognitive (Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013), psychological (Eller et al. Reference Eller, Kirksey, Nicholas, Corless, Holzemer, Wantland, Willard, Robinson, Hamilton, Sefcik, Moezzi, Mendez, Rosa and Human2013), and behavioral (Olley, Reference Olley2006) outcomes through approaches utilizing psycho-education (Olley, Reference Olley2006; Eller et al. Reference Eller, Kirksey, Nicholas, Corless, Holzemer, Wantland, Willard, Robinson, Hamilton, Sefcik, Moezzi, Mendez, Rosa and Human2013) or focusing on meditational processes for cognitive outcomes (Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013). Group interventions (3–24 sessions) primarily addressed psychological (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Reference Li, Liang, Ji, Wu and Xiao2014), behavioral (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Peltzer et al. Reference Peltzer, Ramlagan, Jones, Weiss, Fomundam and Chanetsa2012; Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013; Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014), and biological (SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012) outcomes through approaches utilizing mindfulness meditation (SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012), skills training, problem solving, or cognitive behavioral approaches (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Reference Li, Liang, Ji, Wu and Xiao2014; Peltzer et al. Reference Peltzer, Ramlagan, Jones, Weiss, Fomundam and Chanetsa2012; Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013; Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014). Interventions were delivered by a wide range of professionals and non-specialists. Only one study (Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013) noted the cultural appropriateness of the tested intervention.
Control/comparison groups
For most studies, control participants received the standard of care (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Reference Li, Liang, Ji, Wu and Xiao2014; Peltzer et al. Reference Peltzer, Ramlagan, Jones, Weiss, Fomundam and Chanetsa2012; SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012; Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013; Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014); three studies (Olley, Reference Olley2006; Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013; Eller et al. Reference Eller, Kirksey, Nicholas, Corless, Holzemer, Wantland, Willard, Robinson, Hamilton, Sefcik, Moezzi, Mendez, Rosa and Human2013) utilized an attention-matched control intervention.
Outcome measures
Mental health outcomes were reported in all studies (Table 1); all primary mental health outcomes were measured using standardized psychological symptom scales. None of the studies reported including a diagnosis of mental disorder. Outcomes related to depression were reported in all but two studies (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012). In the latter, composite mental health outcome measures were utilized. See Table 1 for mental health and related psychological assessments utilized across studies. Six studies (Olley, Reference Olley2006; Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012; SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012; Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013; Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013; Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014) noted attention to cultural adaptation of measures or validation of measures in the country in which the study took place.
Intervention effects
Four of the 10 studies reported a significant between-condition intervention effect for PLWH (Olley, Reference Olley2006; Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Reference Li, Liang, Ji, Wu and Xiao2014; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014). Further, Boivin et al. (Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013) and Eloff et al. (Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014), both family studies with HIV-infected caregivers and HIV-uninfected children, found significant effects in the child sample but non-significant effects in the HIV-infected adult caregivers; notably, these studies were designed to improve neurocognitive (Boivin et al. Reference Boivin, Bangirana, Nakasujja, Page, Shohet, Givon, Bass, Opoka and Klein2013) and resiliency (Eloff et al. Reference Eloff, Finestone, Makin, Boeving-Allen, Visser, Ebersohn, Ferreira, Sikkema, Briggs-Gowan and Forsyth2014) outcomes in children. Four studies (Peltzer et al. Reference Peltzer, Ramlagan, Jones, Weiss, Fomundam and Chanetsa2012; SeyedAlinaghi et al. Reference Seyedalinaghi, Jam, Foroughi, Imani, Mohraz, David and Black2012; Eller et al. Reference Eller, Kirksey, Nicholas, Corless, Holzemer, Wantland, Willard, Robinson, Hamilton, Sefcik, Moezzi, Mendez, Rosa and Human2013; Kaaya et al. Reference Kaaya, Blander, Antelman, Cyprian, Emmons, Matsumoto, Chopyak, Levine and Smith Fawzi2013) resulted in positive but non-significant intervention effects on mental health outcomes.
Pilot, feasibility, and quasi-experimental studies
In addition to the 10 RCT studies described in detail above, 12 additional preliminary studies were identified that provide future directions for mental health intervention with PLWH in LMIC settings. These studies, details shown in Table 2, were either described by the authors as pilot trials (many with RCT methods) or were not conducted using an RCT design.
Study location
Pilot, feasibility, and quasi-experimental studies were conducted in, Tanzania (Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ), South Africa (Field & Kruger, Reference Field and Kruger2008; Mundell et al. Reference Mundell, Visser, Makin, Kershaw, Forsyth, Jeffer and Sikkema2011; Bhana et al. Reference Bhana, Mellins, Petersen, Alicea, Myeza, Holst, Abrams, John, Chhagan, Nestadt, Leu and Mckay2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014), Cameroon (Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014), China (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005; Yu et al. Reference Yu, Lau, Mak, Cheng, Lv and Zhang2014), Thailand (Jirapaet, Reference Jirapaet2000), India (Nyamathi et al. Reference Nyamathi, Salem, Meyer, Ganguly, Sinha and Ramakrishnan2012, Reference Nyamathi, Ekstrand, Salem, Sinha, Ganguly and Leake2013), and Iran (Ravaei et al. Reference Ravaei, Hosseinian and Tabatabaei2013).
Participants
A total of 924 HIV-infected individuals participated across all studies. A median baseline sample size of 60 (range 16–361) was reported across all trials. The median retention rate reported post-intervention was 88.3% (range 45–100%). Study samples were diverse, and included drug-addicted males (Ravaei et al. Reference Ravaei, Hosseinian and Tabatabaei2013), women only (Nyamathi et al. Reference Nyamathi, Salem, Meyer, Ganguly, Sinha and Ramakrishnan2012, Reference Nyamathi, Ekstrand, Salem, Sinha, Ganguly and Leake2013), pregnant women or mothers (Jirapaet, Reference Jirapaet2000; Mundell et al. Reference Mundell, Visser, Makin, Kershaw, Forsyth, Jeffer and Sikkema2011), children (Bhana et al. Reference Bhana, Mellins, Petersen, Alicea, Myeza, Holst, Abrams, John, Chhagan, Nestadt, Leu and Mckay2014), patients screened for depression (Field & Kruger, Reference Field and Kruger2008; Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014), individuals in a symptomatic stage of infection (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005), and a general population of HIV-infected men and women (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014; Yu et al. Reference Yu, Lau, Mak, Cheng, Lv and Zhang2014). Four of the studies reported inclusion criteria based on depressive symptoms or disorder (Field & Kruger, Reference Field and Kruger2008; Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014).
Study design
Five of the pilot studies randomized individual participants (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005; Bhana et al. Reference Bhana, Mellins, Petersen, Alicea, Myeza, Holst, Abrams, John, Chhagan, Nestadt, Leu and Mckay2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014) and one study randomized clusters (Nyamathi et al. Reference Nyamathi, Salem, Meyer, Ganguly, Sinha and Ramakrishnan2012) to the intervention or control condition. Three studies were quasi-experimental, and did not randomize participants to condition (Jirapaet, Reference Jirapaet2000; Field & Kruger, Reference Field and Kruger2008; Mundell et al. Reference Mundell, Visser, Makin, Kershaw, Forsyth, Jeffer and Sikkema2011). Three studies were pre-experimental with a one-group, pre-posttest design (Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a , Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014; Yu et al. Reference Yu, Lau, Mak, Cheng, Lv and Zhang2014). Most of the studies (8 of 12) measured effects at posttest only and utilized sample sizes appropriate for pilot studies.
Intervention content and delivery method
The interventions tested in these studies were diverse. Most interventions were designed for delivery within groups (Jirapaet, Reference Jirapaet2000; Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005; Field & Kruger, Reference Field and Kruger2008; Mundell et al. Reference Mundell, Visser, Makin, Kershaw, Forsyth, Jeffer and Sikkema2011; Ravaei et al. Reference Ravaei, Hosseinian and Tabatabaei2013; Bhana et al. Reference Bhana, Mellins, Petersen, Alicea, Myeza, Holst, Abrams, John, Chhagan, Nestadt, Leu and Mckay2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014; Yu et al. Reference Yu, Lau, Mak, Cheng, Lv and Zhang2014), one was designed for delivery with individuals (Nyamathi et al. Reference Nyamathi, Salem, Meyer, Ganguly, Sinha and Ramakrishnan2012, Reference Nyamathi, Ekstrand, Salem, Sinha, Ganguly and Leake2013), and two were pharmacological studies that utilized a clinic-based model for task-shifting antidepressant management (Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014). The individual-level intervention (six sessions) addressed behavioral outcomes using psychoeducation, coping, and skills training (Nyamathi et al. Reference Nyamathi, Salem, Meyer, Ganguly, Sinha and Ramakrishnan2012, Reference Nyamathi, Ekstrand, Salem, Sinha, Ganguly and Leake2013). Group interventions (1–12 sessions) targeted behavioral (Jirapaet, Reference Jirapaet2000; Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Bhana et al. Reference Bhana, Mellins, Petersen, Alicea, Myeza, Holst, Abrams, John, Chhagan, Nestadt, Leu and Mckay2014) and psychological (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005; Field & Kruger, Reference Field and Kruger2008; Mundell et al. Reference Mundell, Visser, Makin, Kershaw, Forsyth, Jeffer and Sikkema2011; Ravaei et al. Reference Ravaei, Hosseinian and Tabatabaei2013; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014; Yu et al. Reference Yu, Lau, Mak, Cheng, Lv and Zhang2014) outcomes through utilization of art therapy (Field & Kruger, Reference Field and Kruger2008), cognitive behavioral therapy (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005), peer support counseling/group therapy, coping and stress management (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Mundell et al. Reference Mundell, Visser, Makin, Kershaw, Forsyth, Jeffer and Sikkema2011; Yu et al. Reference Yu, Lau, Mak, Cheng, Lv and Zhang2014), skills building (Jirapaet, Reference Jirapaet2000), and interpersonal therapy (Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014). Both of the pharmacological interventions aimed to reduce depression symptoms over a period of 12 weeks through a task-shifting model (Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014). A wide range of professionals and non-specialists delivered the interventions.
Control/comparison condition
Most studies (eight) used a comparison or control condition, with six of the 12 studies randomizing participants to condition (Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005; Nyamathi et al. Reference Nyamathi, Salem, Meyer, Ganguly, Sinha and Ramakrishnan2012, Reference Nyamathi, Ekstrand, Salem, Sinha, Ganguly and Leake2013; Ravaei et al. Reference Ravaei, Hosseinian and Tabatabaei2013; Bhana et al. Reference Bhana, Mellins, Petersen, Alicea, Myeza, Holst, Abrams, John, Chhagan, Nestadt, Leu and Mckay2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014). As shown in Table 2, these included, for example, standard of care, wait list control, and counseling as needed.
Outcome measures
All studies assessed mental health outcomes using various standardized psychological scales (Table 2). Depressive symptomatology was the most commonly assessed mental health outcome; one study (Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014) used major depressive disorder based on a symptom scale and physician assessment.
Preliminary intervention effects
Eleven of the 12 pilot, feasibility, or quasi-experimental studies demonstrated promising effects related to improvements in mental health (Jirapaet, Reference Jirapaet2000; Molassiotis et al. Reference Molassiotis, Callaghan, Twinn, Lam, Chung and Li2002; Chan et al. Reference Chan, Kong, Leung, Au, Li, Chung, Po and Yu2005; Field & Kruger, Reference Field and Kruger2008; Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ; Nyamathi et al. Reference Nyamathi, Salem, Meyer, Ganguly, Sinha and Ramakrishnan2012, Reference Nyamathi, Ekstrand, Salem, Sinha, Ganguly and Leake2013; Ravaei et al. Reference Ravaei, Hosseinian and Tabatabaei2013; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014; Petersen et al. Reference Petersen, Hanass Hancock, Bhana and Govender2014; Yu et al. Reference Yu, Lau, Mak, Cheng, Lv and Zhang2014), or behavioral (Adams et al. Reference Adams, Almond, Ringo, Shangali and Sikkema2012a ; Bhana et al. Reference Bhana, Mellins, Petersen, Alicea, Myeza, Holst, Abrams, John, Chhagan, Nestadt, Leu and Mckay2014) outcomes. One study (Mundell et al. Reference Mundell, Visser, Makin, Kershaw, Forsyth, Jeffer and Sikkema2011) demonstrated mixed effects, with improvements in active coping and self-esteem in the intervention group, but not in depression or social support.
Discussion
There is an urgent need to address mental health in the context of HIV/AIDS in LMICs, which bear the brunt of global HIV infections. Although previous reviews (Crepaz et al. Reference Crepaz, Passin, Herbst, Rama, Malow, Purcell and Wolitski2008; Brown & Vanable, Reference Brown and Vanable2011; Clucas et al. Reference Clucas, Sibley, Harding, Liu, Catalan and Sherr2011; Harding et al. Reference Harding, Liu, Catalan and Sherr2011; Sherr et al. Reference Sherr, Clucas, Harding, Sibley and Catalan2011; Seedat, Reference Seedat2012; Spies et al. Reference Spies, Asmal and Seedat2013; Wu & Li, Reference Wu and Li2013) have identified a large number of RCTs to improve mental health in high-income settings, they have only included a small number of intervention trials conducted in LMICs. The purpose of this review was to systematically identify intervention trials that have addressed mental health among PLWH in LMIC settings, and to synthesize the lessons learned from those studies. Our review identified 22 unique intervention studies, 10 of which were evaluated using rigorous RCT methodology. Although this systematic search included a range of terms for mental health, only intervention trials with depression, anxiety or overall psychiatric distress outcomes were identified. Despite the fact that only a small number of full scale trials provided evidence for improvements in mental health, the findings of the review point to opportunities for further research on interventions to address the mental health needs of PLWH in LMIC settings.
The four RCT intervention trials in our review that demonstrated an impact on mental health primarily utilized a multi-component approach. Interestingly, the most robust outcomes, including over longer term follow up assessments, were found in community based trials (Li et al. Reference Li, Lee, Jiraphongsa, Khumtong, Thammawijaya and Rotheram-Borus2010, Reference Li, Ji, Liang, Ding, Tian and Xiao2011, Reference Li, Liang, Lee, Iamsirithaworn, Wan and Rotheram-Borus2012, Reference Li, Liang, Ji, Wu and Xiao2014; Richter et al. Reference Richter, Rotheram-Borus, van Heerden, Stein, Tomlinson, Harwood, Rochat, van Rooyen, Comulada and Tang2014; Rotheram-Borus et al. Reference Rotheram-Borus, Richter, van Heerden, van Rooyen, Tomlinson, Harwood, Comulada and Stein2014) that contextualized HIV/AIDS and mental health within family interactions or through peer support that addressed issues related to pregnancy and child outcomes. The inclusion of pilot studies and quasi-experimental trials in our review provided a framework for mental health interventions that are in the development phase and potentially proceeding to full scale trials. Although the study methods were acknowledged as less rigorous, many used RCT methodology albeit among small sample sizes, and all reported encouraging results using several innovative intervention approaches.
A number of studies, both RCTs and preliminary studies, were group-based interventions, utilizing a cognitive behavioral approach (including stress management and coping interventions), and often delivered in a task-shifting or task-sharing model with lay counselors or community health workers. Future directions explored in pilot trials included a measurement based care (MBC) stepped approach to antidepressant medication management (Trivedi et al. Reference Trivedi, Rush, Gaynes, Stewart, Wisniewski, Warden, Ritz, Luther, Stegman, Deveaugh-Geiss and Howland2007; Adams et al. Reference Adams, Gaynes, McGuinness, Modi, Willig and Pence2012b ) that employed non-specialists to screen and monitor depressive symptoms, thereby supporting intervention at the clinic system level. These trials, as well as two others that evaluated psychotherapeutic approaches, were the only studies that used an inclusion criterion for mental disorder or depressive symptoms. Several of these pilot trials included an intervention focus or secondary outcome measure of adherence to ART. These study methods and intervention approaches point the way forward for mental health intervention trials with PLWH in LMICs, including integration with HIV care and treatment.
The studies we identified had methodological limitations similar to those documented in prior reviews of trials conducted primarily in HICs (Crepaz et al. Reference Crepaz, Passin, Herbst, Rama, Malow, Purcell and Wolitski2008; Clucas et al. Reference Clucas, Sibley, Harding, Liu, Catalan and Sherr2011; Sherr et al. Reference Sherr, Clucas, Harding, Sibley and Catalan2011; Seedat, Reference Seedat2012; Spies et al. Reference Spies, Asmal and Seedat2013). Of key importance only a few studies used mental disorder or above threshold symptom levels as an inclusion criterion for trial selection. This suggests that either the interventions may not have targeted PLWH experiencing significant psychological distress or that symptom levels were sub-threshold, making it difficult to demonstrate an intervention effect. In addition, a limited number of studies provided information on the cultural appropriateness of the intervention or the adaptation and validation of the mental health measures utilized (Bass et al. Reference Bass, Bolton and Murray2007). Several other secondary limitations of the methodologies used in our included studies should be noted. Even among the RCTs, the majority of the intervention trials assessed either immediate post- or short-term intervention effects, with longer term follow up assessments needed to determine sustainability of intervention effects. Most studies provided a general description of the intervention approach, but a detailed description of intervention components and fidelity to them in delivery would enhance the understanding of intervention outcome findings. Finally, intervention trials using non-specialists to deliver mental health interventions (i.e. a task-sharing model) did not provide adequate information on the training and supervision of the providers (Patel et al. Reference Patel, Araya, Chatterjee, Chisholm, Cohen, De Silva, Hosman, Mcguire, Rojas and Van Ommeren2007).
Despite the methodological limitations of the studies included in this review, it is encouraging to see an increasing number of mental health intervention trials for PLWH conducted in LMICs, which span a wide range of populations, countries, and intervention approaches. Additional lessons can be drawn from efficacious interventions for depression treatment in LMICs, (Bolton et al. Reference Bolton, Bass, Neugebauer, Verdeli, Clougherty, Wickramaratne, Speelman and Weissman2003; Patel et al. Reference Patel, Araya, Chatterjee, Chisholm, Cohen, De Silva, Hosman, Mcguire, Rojas and Van Ommeren2007, Reference Patel, Simon, Chowdhary, Kaaya and Araya2009; Rahman et al. Reference Rahman, Malik, Sikander, Roberts and Creed2008), even if not specific to PLWH. Such interventions have been integrated into routine health care, adapted to local cultural context, and implemented by non-specialists. The intervention approaches for treating depression varied, but reflect approaches identified in this review for PLWH, including a collaborative stepped care approach (Patel et al. Reference Patel, Araya, Chatterjee, Chisholm, Cohen, De Silva, Hosman, Mcguire, Rojas and Van Ommeren2007, Reference Patel, Simon, Chowdhary, Kaaya and Araya2009), home-based individual CBT (Rahman et al. Reference Rahman, Malik, Sikander, Roberts and Creed2008), and interpersonal group therapy (Bolton et al. Reference Bolton, Bass, Neugebauer, Verdeli, Clougherty, Wickramaratne, Speelman and Weissman2003). Although mental disorders in HIV care settings in LMICs often go undiagnosed due to lack of screening protocols (Breuer et al. Reference Breuer, Stoloff, Myer, Seedat, Stein and Joska2014; Tsai, Reference Tsai2014), these studies suggest that integration of mental health screening and intervention into health care settings would be an effective approach for improving mental health among PLWH. Two of the preliminary studies we identified support the feasibility of a MBC approach for antidepressant medication in the HIV care setting (Adams et al. Reference Adams, Gaynes, McGuinness, Modi, Willig and Pence2012b ; Pence et al. Reference Pence, Gaynes, Atashili, O'donnell, Kats, Whetten, Njamnshi, Mbu, Kefie, Asanji and Ndumbe2014), similar to the stepped approach in the MANashanti Sudhar Shodh (MANAS) trial (Patel et al. Reference Patel, Araya, Chatterjee, Chisholm, Cohen, De Silva, Hosman, Mcguire, Rojas and Van Ommeren2007, Reference Patel, Simon, Chowdhary, Kaaya and Araya2009), yet more medication-based or combined medication and therapy based trials are needed.
CBIs, including problem solving, skills training, and stress management, commonly used in both HIC and LMIC, support the use of cognitive-behavioral treatments as a key mental health intervention approach. However, there is a need for cultural adaptation and tailoring mental health idioms to the local context, which may preclude the ready transplant of existing CBIs for PLWH. Research trials are still needed to test factors such as required intervention length for feasibility, effectiveness and maintenance of effect, and delivery by non-specialists. There is a need for task-sharing and interventions that can be delivered by non-specialists that are brief and scalable, while providing supervision and fidelity monitoring.
While mental health interventions for PLWH should draw upon the broader evidence of efficacious mental health interventions, they must also remain attuned to issues that are unique for a population living with HIV. These include potential barriers related to HIV-related stigma (Skinner & Mfecane, Reference Skinner and Mfecane2004), substance abuse co-morbidities (Gonzalez et al. Reference Gonzalez, Barinas and O'Cleirigh2011; Kader et al. Reference Kader, Seedat, Koch and Parry2012), and other disorders prevalent among PLWH such as PTSD (Machtinger et al. Reference Machtinger, Wilson, Haberer and Weiss2012). Multilevel system-strengthening approaches that integrate mental health care into HIV care and prevention within health care and community based organizations has been recommended (Joska & Sorsdahl, Reference Joska and Sorsdahl2012; Lund et al. Reference Lund, Joska, Stein and Grant2014). Areas for future research in LMICs include the integration of mental health treatment with adherence, HIV care engagement, and HIV prevention (Sikkema et al. Reference Sikkema, Watt, Drabkin, Meade, Hansen and Pence2010; Chibanda et al. Reference Chibanda, Benjamin, Weiss and Abas2014). Thus, one priority for future research is to conduct RCTs of mental health interventions that improve mental health and enhance HIV treatment and prevention.
The findings from this review of interventions to improve mental health among PLWH in LMICs also provide lessons learned and potential future directions to improve related efforts in HICs. Effective interventions in LMICs utilized family or multilevel interventions and were integrated within community based health care – approaches that contextualize mental health and provide an opportunity to address comorbidities. These approaches, in combination with addressing structural barriers to care such as poverty, health care access, and mental health care policies, are also relevant in HICs, especially in settings where health disparities clearly exist. Given the limited mental health resources in LMICs, including the absence of specialists trained in mental health treatment, the LMIC interventions incorporated approaches delivered by non-specialists. This task-sharing approach is also relevant and should be evaluated in HIC settings, particularly in communities and settings where access to mental health care is limited. Research methodologies related to monitoring intervention fidelity and supervision of non-specialists could enhance our understanding of key elements of effective interventions in both settings. Lastly, this review of interventions in LMIC settings offers lessons for the adaptation of available evidence-based interventions with attention to language, culture, and literacy, as well as feasibility of intervention length. These factors may also impact the effectiveness of mental health intervention for PLWH in HICs, and if better addressed, could improve the outcomes in higher income settings where disparities and cultural differences exist.
Our search strategy, while systematized, cannot guarantee the identification of all interventions to improve mental health among PLWH in LMICs, and omission of related intervention research is possible and may have influenced our conclusions. Unlike prior reviews (Clucas et al. Reference Clucas, Sibley, Harding, Liu, Catalan and Sherr2011; Seedat, Reference Seedat2012; Spies et al. Reference Spies, Asmal and Seedat2013), we intentionally cast a wide net that resulted in the inclusion of studies ranging from multilevel family and community based approaches to a group adherence intervention that also assessed the impact on depression. In addition, we included trials that reported mental health as secondary outcomes (4 of 22 studies). Although this approach broadly defined mental health and supports the importance of addressing mental health in context, a limited number of RCTs were identified, and only a portion of these trials provided evidence for the efficacy of the mental health intervention, even when looking for post-only mental health outcomes. Despite these potential shortcomings, this review provides an overview of the body of evidence available on mental health treatment of PLWH on LMICs, and offers suggestions for the path forward for understanding and addressing these needs.
Conclusion
There is a paucity of empirical data investigating the effectiveness of interventions for mental disorders and psychological distress among PLWH in LMICs. The available data are restricted to several RCTs with widely varied approaches and methodology; and to several smaller pilot, and innovative studies. It is not possible therefore to describe from such a review, the nature, content, and delivery of an ideal intervention. Key issues such as adapting the intervention to suit local culture, language, and resource-limitations are typically not addressed. We are some way from being able to define an ideal intervention, and so a framework for building interventions of this kind is a desirable next step.
Acknowlegements
This manuscript was supported by the Duke Center for AIDS Research (P30 AI064518) and a grant from NIMH (R34 MH102001).
Conflict of Interest
None.





