Children’s vegetable intake is persistently low in Australia and globally, which is linked to poor health and increased risk of non-communicable diseases(1,2) . In Australia, despite most children meeting vegetable intake recommendations early in the complementary feeding stage (96 % at 9 months of age)(Reference Spence, Campbell and Lioret3), adherence subsequently reduces substantially, with only 3 % at 1·5 years of age(Reference Spence, Campbell and Lioret3) and 7–13 % at 2–4 years of age meeting recommendations(1,Reference Spence, Campbell and Lioret3) . This is of concern as early childhood is a critical period for the establishment of life-long dietary behaviours, food preferences and habits(Reference Birch4-Reference Drewnowski6), which persist into adolescence and adulthood(Reference Skinner, Carruth and Bounds7,Reference Mikkila, Rasanen and Raitakari8) . Specifically, children’s liking and acceptance of, and stability in intake of, vegetables have been shown to be formed by 3 years of age, tracking into adolescence and beyond(Reference Hodder, O’Brien and Tzelepis9,Reference Taylor, Hays and Emmett10) . It is therefore essential to understand how to improve intake of vegetables early in life.
While taste preferences and liking of vegetables are important determinants of children’s intake(Reference Caton, Blundell and Ahern11), social determinant of health models recognise the impact of social-cultural, economic and physical conditions in determining availability and accessibility of vegetables(12). Young children’s preferences and intake are further influenced by family-related factors such as parental intake, preferences and parenting style(Reference Rasmussen, Krølner and Klepp13). A range of strategies are therefore required to improve children’s vegetable intake early in life. A recent Umbrella review of systematic reviews published from 2015 to 2020(Reference Bell, Gardner and Tian14) demonstrated that liking and acceptance of vegetables in early childhood can be improved by repeated exposure to taste, texture and appearance of a vegetable, and positive experiences with vegetables throughout the first 2000 d (conception to age 5 years(Reference Schwartz, Scholtens and Lalanne15)), with subsequent improvements in children’s intake. Moreover, repeated exposure to a variety of vegetables of various flavours and textures in early childhood is vital for shaping children’s vegetable liking(Reference Bell, Gardner and Tian14), which successively influences food intake patterns throughout life(Reference Scaglioni, De Cosmi and Ciappolino16,Reference Appleton, Hemingway and Rajska17) . Thus, current evidence supports the practical strategies of repeatedly exposing children to a small amount of a variety of vegetables to increase vegetable liking as a key predictor of intake.
National guidelines, resources and other initiatives exist that promote the importance of vegetable intake in early childhood. However, such guidelines commonly address the ‘what’ and the ‘why’, that is, vegetable intake recommendations to support children’s growth, health and development, and not the ‘how to’, that is, evidence-informed practical strategies. Thus, there are uncertainties about the effectiveness and practicality of interventions or strategies to increase vegetable intake in early childhood(Reference Hodder, O’Brien and Tzelepis9). It is therefore important to develop evidence-informed, practical advice messages on how to support the development of children’s liking, and intake, of vegetables throughout the first 2000 d, for dissemination to parents and carers, health professionals, policymakers and food industry(Reference Bell, Gardner and Tian14).
This research is part of a multi-method project designed to identify opportunities to strengthen advice to support children’s liking and intake of vegetables in the early years.
Previous research: framework development, project phases 1 and 2
Theoretical framework
The multi-method project was informed by an a priori sensory and behavioural vegetable liking strategy framework. This framework was adapted from existing complementary feeding (what, when and how of eating)(Reference Schwartz, Scholtens and Lalanne15) and food choice development(Reference Mojet and Cox18) frameworks, with a focus on the sensory and behavioural strategies to improve children’s liking of vegetables. Sensory strategies include flavour–flavour and flavour–nutrient learning, visual and taste exposure, and experiential learning, while examples of behavioural strategies were conditioning, imitation and modelling, and cognitive knowledge transfer. These strategies previously evaluated in the literature for increasing vegetable liking and intake were mapped against the ‘when’ (i.e. timing), ‘what’ (i.e. sensory exposure) and ‘how’ (i.e. parent–child interaction) of feeding. The framework themes focus on modifiable factors (e.g. parenting style and practices) relevant to public health policy and guidelines. Child-centred factors such as child sensory sensitivities and child temperament, which may also influence children’s vegetable liking in some individuals yet require more intensive intervention to modify, were excluded. The framework has been published previously(Reference Bell, Gardner and Tian14).
Phase 1: Desktop review
Phase 1 of the research was a Desktop review of current advice in Australian guideline documents completed in October 2018. Eighteen guideline and position statement documents were sourced from national, state and local stakeholder websites relating to maternal, infant and early years guidance and advice(19–36). Examples include the Australian Dietary Guidelines(27) and Infant Feeding Guidelines (NHMRC)(28), Get Up & Grow Healthy Eating and Physical Activity for Early Childhood (Commonwealth Department of Health)(20) and Caring for Children Birth to 5 years (NSW Ministry of Health)(32). Each document was assessed against the themes of the a priori vegetable liking strategy framework in terms of clarity, ease, detail and practicality of advice using a scoring process adapted from Schwartz and colleagues(Reference Schwartz, Scholtens and Lalanne15) (see online supplementary material, Supplementary File 1). The findings from this review revealed that the majority of advice provided in Australian guidelines was too brief, focused on ‘what’ or ‘when’ to feed rather than ‘how’ to feed, and not specific to vegetables. While some guidelines addressed several vegetable liking themes, it was rarely in the context of vegetables, instead providing general dietary advice. These results highlight opportunities to strengthen existing recommendations by providing more explicit and actionable advice of how vegetable liking can be developed and fostered, to ultimately increase intakes of vegetables in early childhood.
Phase 2: Umbrella review
Phase 2 of the project was an Umbrella review(Reference Bell, Gardner and Tian14), the purpose of which was to synthesise the evidence from published systematic reviews to determine the effectiveness of sensory and behavioural strategies to facilitate liking (primary outcome) of vegetables in children aged 0–5 years, as key predictors of vegetable intake (secondary outcome). An a priori protocol for the review was registered with PROSPERO (CRD42019119556). The evidence from eleven systematic reviews(Reference Appleton, Hemingway and Rajska17,Reference Paroche, Caton and Vereijken37-Reference Nehring, Kostka and von Kries45) , published from 2015 to 2020, containing eighty-five unique primary studies was reviewed and synthesised. Strategy effectiveness was synthesised into three categories based on evidence strength: (1) Promising (large and consistent body of moderate quality evidence; quality assessed using the AMSTAR 2 critical appraisal rating(Reference Shea, Reeves and Wells46)); (2) Emerging (small to moderate body of mixed consistency and quality evidence) and (3) Limited (small body of limited consistency and quality evidence).
The aim of phase 3 of this multi-method research was to build on the outcomes from phases 1 and 2 and help in the translation of best evidence into practical messages which could facilitate adoption and be actioned at a local policy and practice level. In particular, this phase of the research sought to identify opportunities to strengthen vegetable-specific advice for the maternal, infant and early years, to support the development of children’s liking and intake of vegetables throughout the first 2000 d. The objectives were to: (1) garner consensus among key stakeholders and end users and prioritise a set of evidence-informed statements to promote children’s liking and intake of vegetables; (2) translate these statements into advice messages for key stakeholders, specific to the maternal, infant and early years and (3) validate the advice messages with the evidence and advice gaps to develop a series of advice messages for dissemination.
Methods
Project overview
This research presents the third and final phase of a multi-method project designed to identify opportunities to strengthen advice to support children’s liking and intake of vegetables in the early years, including triangulation of findings from all three phases (described below).
Phase 3: Development and consensus on evidence-informed advice statements
Advice statement development
Sensory and behavioural strategies from the Umbrella review relating to the maternal (perinatal and lactation, −4 months pre-birth to 24 months post-birth), infant (complementary feeding, 4–6 to 24 months) and early years (family diet, 24 to 36 months) were extracted and synthesised into evidence-informed statements. This occurred via consensus discussion between experts in nutrition, maternal/family and child health, and infant feeding. Evidence-informed statements were then mapped against the vegetable liking strategy framework developed a priori, to ensure that all strategies were being addressed, resulting in a set of thirty evidence-informed statements (see online supplementary material, Supplementary file 2). For example, for the theme of ‘intake’ during the lactation stage, the statement developed was: ‘Breastfeeding duration (> 3months) for vegetable-consuming mothers supports vegetable intake in children up to 2 years and vegetable acceptance and intake at 3·7 years’.
Phase 3a: Stakeholder prioritisation and consensus process on advice
For the first part of phase 3, which was designed to garner consensus on advice, a group of experts across maternal and child health and development, psychology, sensory science, education and nutrition were consulted and a prioritisation and consensus process applied to the evidence-informed statements developed above. This process consisted of a single nominal group technique (NGT) workshop followed by a Delphi survey to identify and achieve consensus on priority advice to support children’s liking of vegetables in early life. The consensus methodologies were chosen as a systematic process that facilitates both idea generation and consensus development(Reference Cantrill, Sibbald and Buetow47). The study’s original protocol involved a series of NGT workshops only; however, due to coronavirus disease (COVID-19) social distancing measures, subsequent NGT workshops were adapted to the Delphi survey process to progress the study in a timely manner. Fig. 1 outlines the study methodology.

Fig. 1 Flow chart of study processes, study participants and advice adoption priorities generated
Nominal Group Technique (NGT) workshop
Participants
While there are no set sample size requirements for NGT, optimal group size for NGT in terms of productivity and participant satisfaction is reported at no >10(Reference Burton, Pathak and Zigli48). The sample size for the NGT workshop was informed by a desire to maintain the group dynamic of the technique in addition to including representation from a range of experts. Participants were purposefully sampled to capture perspectives from nutrition, sensory science, psychology, maternal, child and family health, and infant/child feeding, in addition to covering the study’s key feeding transition stages (perinatal and lactation, complementary feeding and family diet). Experts were identified through a range of strategies, including use of existing contact lists and collegial contacts (attained through snowballing) with direct invitations issued to eleven potential participants.
Procedure
To develop priorities to strengthen advice across the maternal, infant and early years, this study utilised four key stages common in NGT methodology during a 6-h in-person workshop moderated by an experienced facilitator (S.K.): (1) silent idea generation, (2) round robin, (3) group discussion (clarification) and (4) voting(Reference Wilfley, Staiano and Altman49) (Fig. 1). Prior to the NGT workshop, participants were provided with the thirty evidence-informed statements (see online supplementary material, Supplementary File 2) (an output of the Umbrella review process) and the outcomes of the review of policy and guideline advice (i.e. the Desktop review) for review and familiarisation.
Stage 1: Silent idea generation
Participants silently reflected and recorded their top six individual ideas for advice priorities in response to the following questions: (1) What are the key priority areas for each feeding transition stage? (2) Which evidence-informed statements need to be reviewed (and why)? (3) Where are the research gaps? (4) What is the priority for addressing/strengthening current advice (i.e. immediate or longer-term)? What is pertinent given our goal of supporting vegetable liking development in the first 2000 d? and (5) Why is it immediate OR longer-term (justification)? Participants were asked to consider the following: importance for practice (i.e. need and impact), limitations/gaps, concerns around evidence quality or scope and generalisability, missing data, red flags, likely support from key stakeholders (e.g. government and health professionals/professional associations) and end users (e.g. families and carers, and food industry), and feasibility of adoption. Facilitators maintained silence during this phase except for clarifying the purpose of the activity.
Stage 2: Round Robin
Each participant presented their ideas to the group in a round robin format. Notes were taken during the process and displayed for transparency. Participants were discouraged from evaluating others’ contributions during this stage.
Stage 3: Group discussion (clarification)
Participants engaged in discussion around the development and refinement of ideas to clarify meaning and exclude, include or alter ideas previously raised.
Stage 4: Ranking
Participants independently ranked their top three preferences for the evidence-informed statements for each feeding transition stage from the generated ideas (Stages 1–3) using the voting criteria outlined in Table 1, allocating a score of three for their top-ranked priority, two for second highest and one for third highest. Facilitators summed the scores for each idea and presented the prioritised list of evidence-informed statements to all participants prior to concluding the workshop.
Table 1 Importance and achievability criteria for prioritising the evidence-informed statements and translated advice messages

Delphi survey
Participants
There is limited guidance on appropriate sample sizes for Delphi surveys(Reference Hsu and Sandford50). The Delphi methodology relies more on the process for reaching consensus in a group of experts than on statistical power, with the scope of the issue and available resources typically determining participant numbers(Reference Hasson, Keeney and McKenna51,Reference Powell52) . Given the specific interest of this study and the resources available, a sample size of 20–25 was sought, consistent with sample sizes reported in other Delphi surveys(Reference Veziari, Kumar and Leach53). A purposeful sample of stakeholders considered to have high interest and influence in this area(54), from academia, government, policymaking, professional organisations, health services and non-government organisations, was identified by collegial contacts and web-based searches. A minimum of one representative from each stakeholder category was invited via direct email to participate. In total, eighty-three invitations were sent out to stakeholders from thirty-eight organisations.
Procedure
A Delphi survey comprising two rounds was undertaken. The Delphi methodology is a structured, rigorous and established process which is commonly used to garner consensus among a group of experts in a particular field(Reference Sinha, Smyth and Williamson55). The approach enables anonymous exploration on a complex topic by a group of experts in an iterative series of rounds until consensus is reached(Reference Slade, Dionne and Underwood56). Data from each round are analysed and collated, and the results are presented back to participants for reviewing and providing further comments in the subsequent rounds(Reference Veziari, Kumar and Leach53,Reference Dars, Uden and Kumar57) . Delphi surveys do not have a set limit on the number of rounds required; instead, repeat rounds are continued until consensus is reached, with three rounds being common(Reference Veziari, Kumar and Leach58). As there is no set agreement on consensus, as has been widely used in other health research, an a priori decision was made that once agreement (≥70 % of participants) was reached the Delphi survey concluded(Reference Veziari, Kumar and Leach59-Reference Hicks62).
The Delphi survey was administered online using Qualtrics®. The participant information sheet and consent letter formed the first part of the survey, and upon providing consent, participants were able to progress. Initial demographic questions were asked prior to commencing the main survey, including gender, State or Territory of residence, sector(s) of work, area(s) of work and experience in the relevant feeding transition stages. Round 1 was open in May–June 2020, and round 2 in July 2020. Participants who completed the previous round were invited to participate in subsequent rounds. Participants were invited by email with up to two reminders sent each round. See online supplementary material, Supplementary File 3 for examples of the Delphi survey questions.
Round 1: Ranking of the importance and achievability of the evidence-informed statements and phrasing and translating the evidence-informed statements into advice messages
In round 1, participants were asked to prioritise the evidence-informed statements generated by the expert panel (NGT workshop) by ranking them using the same importance and achievability criteria (Table 1), except for the strength of evidence criteria. A point-grading system was used to calculate the overall ranking of statements, whereby participants allocated a score of three for their top-ranked (first) priority, two for second highest and one for third highest. Statements were considered to have achieved consensus within round 1 when 70 % or more of participants (≥16 of 23 participants) allocated the same ranking to a statement. For instance, if more than sixteen participants voted a statement as their first priority in that feeding transition stage, consensus for the ranking of that specific statement was achieved. Statements that participants (approximately one-third) questioned regarding suitability and consistency with other statements were removed. Following this, participants were asked to provide recommendations for rephrasing and translating the evidence-informed statements into advice messages for uptake in relevant sectors. Open-ended responses to the translated advice messages were themed and analysed for consensus by two authors (H.W. and C.G.). Key words or phrases were extracted from the range of responses and common words or phrases used to formulate advice messages from the translated evidence-informed statements. Recommendations were sought from two additional authors (S.K. and R.G.) where there was ambiguity or disagreement arose.
Round 2: Determining consensus on the translated advice messages
Round 2 was based on advice messages and ranking outcomes from round 1. Participants were presented with the translated advice messages in order of priority and asked to indicate their level of agreement, using a five-point Likert scale ‘strongly agree’ to ‘strongly disagree’ with both the ranking and phrasing of the translated advice message. Consensus was considered achieved if 70 % or more of participants indicated they agreed or strongly agreed with the message and ranking. As consensus was achieved for nearly all statements, further actions of participants in a third round, as planned, were not required. However, the fourteen translated advice messages in order of priority were presented back to the sixteen participants with no further changes required.
Phase 3b: triangulation analysis
For the second part of phase 3, advice messages identified through the stakeholder prioritisation consensus process (NGT workshop and Delphi survey) were mapped against the vegetable liking strategy framework developed a priori and validated against the strength of evidence (Umbrella review) and gaps in guideline advice (Desktop review). The triangulation process led to a final list of advice messages for adoption by key stakeholders (Table 5). These were categorised into three areas for dissemination: (1) Policy and practice; (2) Food industry and (3) Research.
Results
Participant characteristics
The characteristics of participants of the NGT workshop and Delphi survey are summarised in Table 2. All NGT workshop participants (n 8) were from academia as content experts were specifically targeted, while Delphi survey participants (n 23) were from a range of sectors including academia (n 8), non-government/not-for-profit (n 8), government (n 6), health services (n 5) and education (n 1). Representation from a range of discipline areas including nutrition, maternal/family and child health, and infant/child feeding, and experience in the feeding transition stages of interest was achieved for both activities.
Table 2 Characteristics of consensus process participants from the nominal group technique (NGT) workshop (n 8) and Delphi survey (n 23)

* Multiple responses allowed.
Consensus process
Nominal group technique workshop
Nine of the eleven invited stakeholders agreed to participate in the NGT workshop, one of whom was unable to attend the workshop. Prioritisation via silent idea generation (stage 1) resulted in the reduction of thirty statements (n 4 perinatal and lactation stage, n 10 complementary feeding stage, n 16 family diet stage; see online supplementary material, Supplementary File 2) down to sixteen (n 3 perinatal and lactation stage, n 6 complementary feeding stage, n 7 family diet stage; Table 3). The prioritised list of evidence-informed statements per feeding transition stage, at the end of stage 4 of the NGT, is shown in Table 3. The top priority per feeding transition stage was: (1) Perinatal and lactation stage: ‘A vegetable rich diet during pregnancy has health benefits for both mother and baby’ (n 24 votes), (2) Complementary feeding stage: ‘Repeated exposure (up to 10 times or more) of target vegetables increases acceptance (liking) and intake in children aged up to 24 months’ (n 19 votes) and (3) Family diet stage: ‘Increased availability (serving order, portion size, variety, choice, visual presentation) supports vegetable intake in children aged 2–5 years’ (n 20 votes).
Table 3 Rankings and top three priority outcomes from the nominal group technique (NGT) workshop, according to feeding transition stage

* Bold text indicates the top three priority outcomes, per feeding transition stage.
Delphi survey
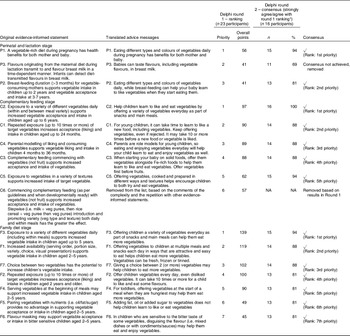
Of the eighty-three invitations sent, twenty-three participants (28 % response rate) completed the round 1 Delphi Survey. Seven participants did not complete round 2, resulting in a total of sixteen participants in round 2. Table 4 outlines the rankings of the evidence-informed statements and the consensus agreement of the ranking and phrasing of the translated advice messages in the Delphi survey.
Table 4 Delphi rankings of the original evidence-informed statements (round 1) and consensus agreement (round 2), according to feeding transition stage, including the translated advice messages

PL, perinatal and lactation; C, complementary feeding; F, family diet.
* ≥70 % agreement = consensus.
In round 1, the most highly ranked priority for the perinatal and lactation stage (n 56 points) was ‘A vegetable rich diet during pregnancy has health benefits for both mother and baby’. For the complementary feeding stage, the most highly ranked priority (n 97 points) was ‘Exposure to a variety of different vegetables daily (within and between meal variety) supports increased vegetable acceptance and intake in children aged up to 6 years’. For the family diet stage, the most highly ranked priority (n 139 points) was ‘Exposure to a variety of different vegetables daily (including within meals) supports increased vegetable intake in children aged up to 5 years’. Attempts of rephrasing and translating each statement were received from all twenty-three participants. Responses were screened, with those such as ‘no comment’ and ‘agree with the original statement’ excluded. The original evidence-informed statements and the translated advice messages for each feeding transition stage are outlined in Table 4.
In round 2, almost all statements (n 14 of 15) received 70 % or more agreement with the ranking and phrasing of translated advice messages (Table 4). Only one translated advice message from the perinatal and lactation stage – ‘Babies can taste flavours, including vegetable flavours, in breast-milk’ – did not reach consensus (11/16, 69 %). Based on this and the comments received, this statement was removed from the final list as it was positioned as a rationale statement rather than an action-orientated message that could be adopted in advice.
Triangulation analysis
Three key areas for dissemination were identified as part of the analysis process including (1) Policy and practice, (2) Food industry and (3) Research. These groups were selected as key influencers of which foods are encouraged or promoted, available to purchase and offered to children to consume. Research was also identified as playing an important role in strengthening the research base where evidence was deemed emerging but not strong enough to recommend for policy and practice adoption.
Policy and practice
Two strategies, ‘repeated exposure’ and ‘vegetable variety’, for both the complementary feeding and family diet stages, and their associated messages, were prioritised in the triangulation analysis for policy and practice. Both strategies were identified as having a strong evidence base (promising evidence identified in the Umbrella review), being of high priority according to key stakeholders (consensus process) and with gaps in current advice (Desktop review) (Table 5). This highlights that these areas could be strengthened to provide more explicit advice in policy and guideline documents regarding repeatedly exposing children to a variety of vegetables.
Table 5 Triangulation analysis outcomes

BF, breast-feeding; DR, Desktop review; UR, Umbrella review.
* Original evidence-informed statements, i.e., were not identified in NGT workshop as a priority therefore were not presented in Delphi for translation to user-friendly messages by stakeholder.
Food industry
Four strategies (Table 5), and their associated advice messages, were identified as being relevant for potential adoption by food industry. These included ‘vegetables as first foods’ (complementary feeding stage), ‘variety’ (complementary feeding to toddlerhood stage), ‘vegetable presentation’ (toddlerhood stage) and ‘pairing’ (adding fat or oil to vegetables) (toddlerhood stage). These were chosen as an opportunity to provide insights to food industry on consistency between current product availability, marketing and promotion activities and the scientific evidence base.
Research
Twelve strategies, and their associated advice messages (Table 5), were identified as opportunities to further build the evidence base, due to having either limited or emerging evidence as identified in the Umbrella review, and thus categorised as advice messages suitable for a research audience. Stakeholder priorities for these strategies ranged from low to high, with some medium to highly ranked priorities having limited evidence to support their dissemination to policy and practice audiences. For example, offering children up to 5 years a ‘choice between vegetables’ and ‘serving vegetables at the beginning of a meal’ were rated as limited evidence, yet medium priority by stakeholders. On the other hand, ‘non-food rewards’ and ‘vegetable-based picture books’ were rated as emerging evidence yet ranked as low priorities by stakeholders.
Discussion
This project used a multi-method stakeholder engagement process to develop a set of evidence-informed maternal, infant and early years advice messages to support the development of children’s liking and intake of vegetables throughout the first 2000 d and to translate these messages for dissemination to relevant audiences. Based on stakeholder priority (high), strength of the evidence (promising) and gaps in advice, two strategies, ‘repeated exposure’ and ‘vegetable variety’, and their associated messages, were identified for dissemination to policy and practice audiences. Four strategies, ‘vegetables as first foods’ (emerging evidence, low stakeholder priority), ‘vegetable presentation’ (emerging evidence, high priority), ‘pairing vegetables with nutrients’ (emerging evidence, low priority) and ‘vegetable variety’ (promising evidence, high priority), and their associated messages, were identified for food industry application. Twelve strategies, where stronger evidence is needed (limited or emerging evidence), were identified as recommendations for future research. These included, for example, the strategies of ‘in-utero’ and ‘lactation flavour exposure’, ‘presentation (appearance)’, ‘vegetable picture books’ and ‘choice’ between vegetables. Collectively, these advice messages can support stronger and more practical advice to promote the development of vegetable liking, and subsequent intake, throughout the first 2000 d.
Policy and practice
Government and health practitioners play a critical role in disseminating practical feeding advice that encourages liking and increased intake of vegetables in the first years of a child’s life. However, gaps in current advice documents limit their effectiveness. Thus, an opportunity exists to strengthen vegetable advice through incorporating the advice messages, associated with the strategies of ‘repeated exposure’ and ‘vegetable variety’, developed in this multi-method, stakeholder engagement research process. These strategies were identified as ‘promising’ evidence in the scientific literature(Reference Bell, Gardner and Tian14) and of high stakeholder importance. Their associated advice messages provide simple, useful and practical advice of how to support liking of vegetables in the early years, characteristics essential for adoption(Reference Netting, Campbell and Koplin63). Such advice messages could be incorporated into national, state and organisational dietary and infant feeding guidelines and related resources, for example, the Australian Infant Feeding Guidelines(28) and related educator guides(64). When supported by such government policy and guidelines, this advice can then be readily communicated by health practitioners, such as Maternal, Child and Family Health Nurses, to families and carers to encourage liking, and increased intake of vegetables in early childhood. It is essential that advice messages are clear and consistent across consumer materials and policy documents, including at both the national and state levels, to ensure they are easily interpreted and adopted by all health professionals, parents and carers(Reference Netting, Campbell and Koplin63). Further advice, underpinned by strong evidence, may be required by parents and caregivers on how to repeatedly expose children to a variety of vegetables, particularly in the context of food-related challenges, such as fussy eating(Reference Taylor, Wernimont and Northstone65,Reference Byrne, Jansen and Daniels66) or access to vegetables(Reference Krolner, Rasmussen and Brug67,Reference Rasmussen, Krolner and Klepp68) . Future research could test the advice messages with consumers, such as parents and carers, to determine their usefulness and acceptability.
Food industry
To support Government and health practitioners, there is scope for food industry to play an increasing role in encouraging children’s vegetable liking and intake. For example, the formulation of single vegetable-only weaning foods would support the strategies and their associated messages, of ‘vegetables as first foods’ (a strategy consistent with a recent narrative review(Reference Chambers69) and consensus reached between infant feeding experts(Reference Chambers, Hetherington and Cooke70)) and exposing children to a ‘variety’ of vegetables (flavours and textures), individually, within- and between-meals and snacks’. In Australia, the range of commercial infant and toddler food products is limited to mixed-vegetable and/or fruit products. That is, of 414 commercial infant and toddler foods available in Australia in 2019, 80 % of fruit and vegetables first foods were fruit-based, with <10 % vegetable-based (two or more vegetables mixed together and typically of the sweet varieties such as carrot or sweet potato) and no single vegetable-only products(Reference Moumin, Green and Golley71). It is therefore evident that reformulation of products and/or product development is warranted to expand the range of single vegetable-only commercial infant and toddler food products available to consumers in Australia, to enable young children to experience a range of vegetable flavours, particularly those that do not appeal to their innate likes (i.e. non-sweet vegetables such as spinach, green beans and broccoli), and those not paired with another flavour (e.g. sweet vegetables or fruits).
Working with food industry would need to ensure that the message regarding the importance of Fe-containing first foods is maintained(Reference Finn, Callen and Bhatia72), particularly given that most commercial infant and toddler products available in Australia are poor sources of Fe(Reference Moumin, Green and Golley71). For example, Fe-containing commercial vegetable products may include spinach or broccoli pouches, as well as Fe-fortified single vegetable products. Product development could also address the strategy of ‘presentation (appearance)’ for 2- to 5-year-olds through the development of vegetable-only snacks or side dishes presented in ways that are attractive and easy to eat, for example, ready-to-eat fresh vegetable rainbow sticks. Care in this area needs to consider choking risk(73). Further, as ‘pairing vegetables with nutrients’ such as fat, oil or sugar does not help children learn to like or eat vegetables and does not have benefits over repeated exposure, this strategy could be communicated to industry to encourage them to instead focus on the simpler strategies of repeated exposure to a variety of vegetables through production and marketing of single vegetable-only products.
Food industry can also play a role through the promotion and marketing of evidence-informed advice messages, relating to the strategies of ‘vegetable variety’, ‘vegetables as a first food’ and vegetable ‘presentation’, and ‘pairing vegetables with nutrients’. For example, messages on food product labels may include ‘iron-rich vegetable first food’, ‘, and ‘eat a rainbow veggie stick’. Marketing could focus on newly developed single vegetable-only commercial infant and toddler food products, as well as on existing vegetable-only products, for example, frozen, tinned and canned vegetables, that may not generally be marketed towards young children, yet are suitable. Thus, through both product reformulation and/or development, and the promotion and marketing of evidence-informed strategies, food industry are vital in increasing children’s vegetable liking and intake, as without the appropriate food supply, the role of Government and health practitioners in advising families and carers on these strategies is limited.
Research recommendations
Increased quantity and quality of research regarding strategies to increase vegetable intake in early childhood would enable determination of whether other strategies are also suitable for dissemination to policy and practice and food industry audiences. Several strategies, where stronger evidence is needed (i.e. identified as either limited or emerging evidence in the scientific literature(Reference Bell, Gardner and Tian14)), were identified as important for future research. Specifically, greater evidence on the strategies of ‘in-utero flavour exposure’ and ‘lactation flavour exposure’, considered high priority by stakeholders yet without sufficient evidence to be disseminated to policy and practice audiences, is required. The current evidence base (two reviews per strategy, rated critically low – moderate, mix of intervention and observational studies) is limited to predominately carrot, garlic or vegetable juices from which the evidence may not be generalisable to other flavours(Reference Bell, Gardner and Tian14). Additional evidence regarding these strategies could support advice on the health benefits of eating vegetables in line with dietary guidelines when pregnant and breast-feeding (which are not currently achieved(74)), beyond those to the mother(27,Reference Ortega75) to benefits to their child. Care needs to be taken in this area to consider additional perspectives, such as ‘do no harm’ (i.e. consideration of the risk of listeriosis from cold vegetable preparations during pregnancy(Reference Verbeke and De Bourdeaudhuij76)) and concerns by breast-feeding women that certain vegetables (e.g. cruciferous vegetables such as broccoli and cabbage) may cause infant colic(Reference Kidd, Hnatiuk and Barber77).
Greater evidence on the strategy of ‘presentation (appearance)’ of vegetables, also considered high priority by stakeholders yet without sufficient evidence for policy and practice uptake, could support the idea that presenting vegetables in appealing (e.g. bright colours, various shapes) and interesting ways (e.g. characters/faces made with vegetables) that are easy and/or fun to eat (e.g. bite-sized) increases children’s vegetable liking and intake. For those statements ranked low by stakeholders, yet with ‘emerging evidence’, an opportunity exists to update stakeholders’ knowledge on the evidence base regarding potentially effective strategies to support children’s vegetable liking. Examples of these strategies include: ‘vegetable picture books’ and ‘vegetables as first foods’. Likewise, for those statements ranked medium by stakeholders, yet with ‘limited evidence’, for example, offering children a ‘choice between vegetables’ and ‘serving vegetables at the beginning of a meal’, an opportunity exists to advise stakeholders on the current lack of evidence underpinning these strategies. Overall, further research could help to identify the most, and least, effective of these strategies to enable prioritisation for incorporation into policy and guideline documents and resources as advice for parents and carers, and into recommendations for food industry.
Strengths and limitations
The primary limitation of this study is that a change in methodology was required to determine stakeholder consensus, from a series of NGT workshops to an online Delphi survey due to social distancing measures related to the COVID-19 global pandemic. This limited the rich depth of participant discussion that is a key advantage of the NGT process(Reference McMillan, King and Tully78). Nonetheless, the Delphi survey method implemented is a commonly used and well-recognised methodology(Reference Hasson, Keeney and McKenna51,Reference Powell52,Reference Sinha, Smyth and Williamson55) which allowed for prioritisation and consensus to be achieved. It further helped to overcome access barriers for potential participants associated with the face-to-face NGT process (e.g. travel time) due to the geographically diverse nature of Australia, thus facilitating participation in the Delphi Survey. Privacy and confidentiality were well considered due to the nature of anonymity in this survey; however, it may have also led to a lack of accountability and loss of respondents in subsequent rounds. That is, while the desired sample size (n 20–25) for the Delphi survey was achieved for round 1, which is consistent with sample sizes reported in other Delphi studies(Reference Veziari, Kumar and Leach58), the sample size declined in round 2 (n 16), which is a common feature of subsequent Delphi rounds. Finally, the prioritised advice messages lack consultation with food industry experts to ensure they are practical for this audience. Food industry was not consulted as they were considered out of scope due to requiring targeted consultation and to minimise potential conflicts of interest and biases with stakeholders who have commercial interests(Reference Mozaffarian, Angell and Lang79). Further conversations with the food industry are warranted to ensure they are a facilitator for children’s vegetable liking and consumption. Parent testing of the advice message wording was also out of scope of the current project; however, this is an important next step for the project to ensure relevance and traction with parents as well as adoption of advice messages to different audiences.
This study is strengthened by the integration of the scientific evidence (Umbrella review), with current advice gaps (Desktop review), expert consensus and stakeholder prioritisation, through a triangulation analysis. Incorporating these key sources of information ensured that the resulting advice messages are not only informed by the best available scientific evidence but are also practical for Australian policy and practice, research and food industry audiences. In addition, the use of consensus methods (NGT and Delphi) and stakeholder engagement process of the study with experts (NGT) in the field as well as end users (Delphi) are strengths of this research. Further, eight participants for the NGT fits within the optimal group size for NGT in terms of productivity and participant satisfaction of no >10(Reference Burton, Pathak and Zigli48). Last, the advice messages were informed by an a priori developed theoretical framework, ensuring advice aligned with suitable theory to promote vegetable liking and intake.
Conclusion
Using a multi-method stakeholder engagement process, informed by a theoretical framework, the scientific evidence and gaps in advice, a set of expertly designed and prioritised evidence-informed maternal, infant and early years advice messages were developed to help address the issue of low vegetable intake in young Australian children. These advice messages can support Government, health practitioners and food industry to encourage the development of children’s vegetable liking, and intake, throughout the first 2000 d. Evidence-informed advice messages regarding ‘repeated exposure’ and ‘variety’ of vegetables are recommended to be incorporated into national, state and organisational dietary and infant feeding guidelines, and related resources. Supported by such documents, these messages can be readily communicated to carers by healthcare practitioners to equip them with useful and practical strategies regarding ‘how to’ help children learn to enjoy and eat vegetables. Food industry also provides a vehicle for marketing and promotion activities regarding ‘vegetable variety’, ‘vegetables as a first food’ and vegetable ‘presentation’. For strategies identified as having ‘limited’ or ‘emerging’ supporting evidence in the scientific literature, further research is required to determine their potential at fostering a love of vegetables in early childhood. Together, Government and health practitioners, food industry and researchers have the potential to significantly improve vegetable liking and acceptance in early childhood, setting children up on the path of life-long vegetable intake habits.
Acknowledgements
Acknowledgements: The authors wish to thank the participants of the Nominal Group Technique workshop and Delphi survey for their time and expert contribution to refining and prioritising the evidence-informed statements and advice messages. Financial support: This project has been funded by Hort Innovation, using the vegetable research and development levy and contributions from the Australian Government. Hort Innovation had no input into the study design, the interpretation of the results or the preparation of this manuscript. Hort Innovation has approved the manuscript for publication. Conflict of Interest: R.B. receives funding for research unrelated to this project from the Children’s Hospital Foundation, under the auspices of the Woolworth’s Centre for Childhood Nutrition Research. Authorship: R.G., S.K., D.C., A.P. and C.G. designed the study; C.G., H.W., B.J., R.G. and S.K. conducted the research (NGT workshop, Delphi Survey, Triangulation analysis); L.B., R.B., K.C., E.D.Q., G.L., M.N. and G.R. were key NGT workshop stakeholders who contributed to garnering consensus and prioritisation of the evidence-informed statements; C.G. and R.G. led the interpretation of the results, with contributions from L.K.B., H.W. and B.J.; L.K.B. wrote the first draft of the manuscript, with contributions from C.G., H.W., B.J. and R.G.; All authors provided critical review of subsequent iterations of the manuscript; All authors read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving research participants were approved by the Flinders University Social and Behavioural Research Ethics Committee (SBREC, #8476). Written informed consent was obtained from all subjects.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980021001907