Approximately two billion people in the world, mainly women and children, are estimated to have micronutrient deficiencies( Reference Tulchinsky 1 ). Maternal nutritional deficiencies are important contributors to adverse birth outcomes such as low birth weight (LBW), stillbirth, preterm birth and early infant death observed in developing countries( Reference Darnton-Hill and Mkparu 2 – Reference Haider and Bhutta 4 ). Stillbirth and prematurity are important perinatal health problems worldwide, with the highest prevalence in sub-Saharan Africa and South Asia( Reference Lawn, Cousens and Zupan 5 ). A baby born prematurely is at increased risk of both early and late complications, such as cerebral palsy, mental retardation, sensory deficits, respiratory and gastrointestinal problems( Reference Tomashek, Shapiro-Mendoza and Davidoff 6 ). No effective and affordable interventions are known to prevent prematurity in developing countries.
Fe deficiency, a primary cause of anaemia, is common in pregnancy and is associated with adverse pregnancy outcomes( Reference Stevens, Finucane and De-Regil 7 ). Requirements for dietary Fe are increased during pregnancy in order to support the expansion of red cell mass, the placenta and fetal demands( Reference Ladipo 8 ). In order to reduce the magnitude of Fe deficiency in pregnancy, the WHO recommends Fe and folic acid supplementations for pregnant women, especially in developing countries( 9 ). Evidence supports significant beneficial effects of Fe intake in early pregnancy, but this is logistically difficult as women in developing countries often start attending antenatal clinics late in pregnancy( Reference Alwan, Greenwood and Simpson 10 , Reference Papadopoulou, Stratakis and Roumeliotaki 11 ). Dietary approaches to improve Fe status may be an additional effective and sustainable means to prevent and correct Fe deficiency; however, data on the relationships of dietary Fe intake with birth outcomes in developing countries are limited.
Mean risk of dietary Ca deficiency in Africa is 54 %, with the highest odds in pregnant women and children( Reference Joy, Ander and Young 12 ). Ca deficiency in pregnancy is due to physiological changes; increased demand from the growing fetus and maternal urinary excretion of Ca are approximately twice as high during this period( Reference Ritchie, Fung and Halloran 13 ). Some key important benefits of Ca in pregnancy include less gestational hypertension, LBW and preterm birth( Reference Buppasiri, Lumbiganon and Thinkhamrop 14 ). Routine Ca supplementation in pregnancy is recommended by the WHO, but currently few national plans include routine Ca supplementation as standard of care, partly due to cost and logistical issues( 15 ).
The present study examined the relationships of dietary Fe and Ca intakes during pregnancy with LBW, preterm birth, small for gestational age, stillbirth and early child mortality. We utilized data obtained from HIV-negative pregnant women who were enrolled in a multivitamin supplementation study in Tanzania.
Methods
We conducted a prospective cohort study among pregnant women enrolled in a randomized, double-blind, placebo-controlled trial of daily prenatal multivitamin supplements. Pregnant women were recruited from nine public health centres in Dar es Salaam, Tanzania, from August 2001 to July 2004. Eligibility criteria included a negative test for HIV infection, willingness to attend the antenatal clinic monthly in study facilities until delivery and estimated gestational age between 12 and 27 weeks according to the last normal menstrual period. Randomized pregnant women were instructed to take a single daily dose of the supplement or placebo tablets from the time of enrolment in the second trimester until 6 weeks post-delivery. Multivitamin supplements included 20 mg thiamin, 20 mg riboflavin, 25 mg vitamin B6, 100 mg niacin, 50 µg vitamin B12, 500 mg vitamin C, 30 mg vitamin E and 0·8 mg folic acid. All women received daily doses of Fe (60 mg of elemental Fe), folic acid (0·25 mg) and sulfadoxine-pyrimethamine for malaria intermittent preventive treatment as standard of care. Further details about the study have been described elsewhere( Reference Fawzi, Msamanga and Urassa 16 ).
A baseline questionnaire that included sociodemographic characteristics, medical and obstetrics history was completed. Dietary intake was assessed by 24 h recalls during monthly antenatal clinic visits from enrolment until 36 weeks of gestational age. Interviews were conducted by research nurses trained on foods and nutrition assessment. The multiple-pass recall approach was used; pregnant women were asked to remember and report freely all foods and beverages consumed in the preceding day. The latter was followed by guiding the respondents to recall eating occasions and times for each specific food consumed. This was accompanied by probing and detailed questions to determine the portion size of food intake, aided by a locally adopted food atlas. The Tanzania Food Composition Tables ( Reference Lukmanji, Hertzmark and Mlingi 17 ) were used to determine nutrient content and quantity.
Women were always encouraged to come to Muhimbili National Hospital for delivery, where they were attended by research midwives. Newborns were weighed immediately after birth.
The study protocol was approved by independent institutional review boards at Muhimbili University of Health and Allied Sciences and the National Institute for Medical Research in Tanzania and the Harvard School of Public Health in the USA.
Study end points
The study’s end points included neonatal death (death within the first 28 d of life) and stillbirth (fetal death after 28 completed weeks of pregnancy). Other end points assessed were LBW (<2500 g), preterm delivery (birth before 37 weeks of gestational age), extremely preterm delivery (birth before 34 weeks of gestational age) and small for gestational age (birth weight below the 10th percentile for gestational age, according to INTERGROWTH)( Reference Villar, Cheikh Ismail and Victora 18 ).
Statistical analysis
Data from the participants with at least one 24 h diet recall were included in the analysis. A mean prenatal dietary intake was estimated as the average of multiple 24 h dietary recalls. Fe sources from meat, fish and poultry were categorized under one group of dietary animal Fe. The mean total dietary Fe, animal Fe and Ca intakes were predictors of the study. The predictors were categorized into four groups based on quartiles: <25th percentile, 25·0–49·9th percentile, 50·0–74·9th percentile and ≥75th percentile.
Missing data of study variables were retained in the analysis using the missing-indicator method( Reference Miettinen 19 ). Log-binomial regression models were used to estimate the relative risk (RR) of each outcome for the higher levels of intake, compared with the lowest level of intake. Relationships between each potential confounder and end points were assessed by bivariate analysis. Predictors with a P value <0·2 in bivariate analysis were included in the multivariate analysis.
In subgroup analyses we tested for interactions between dietary intakes and multivitamin regimen on the outcomes of interest using the Mantel–Haenszel test. There were no statistical interactions between multivitamin regimen and dietary intakes on study outcomes; therefore we present the findings of the associations between dietary intakes and outcomes across both intervention arms. We evaluated the associations across quartiles of nutrient (total Fe, animal Fe and Ca) intakes with adverse birth outcomes and neonatal mortality using the non-parametric test for trend across order groups (nptrend).
All covariates were considered in the analysis. Continuous variables are presented as mean and standard deviation, and as median and interquartile range for skewed distribution. Categorical variables are summarized as percentages. Two-sided Wald test P values are presented. A Filmer–Pritchett wealth index based on family possessions was constructed( Reference Filmer and Pritchett 20 ). The statistical software package Stata® 12.0 was used for data analysis.
Results
Of the 8468 pregnant women enrolled in the study, 7634 (90·1 %) women had known birth outcome and 24 h diet recall information, and hence were included in the current prospective cohort analysis. The median (interquartile range) number of times women were interviewed for 24 h recall was 3 (2–3). Within-subject CV for dietary Fe and Ca intake was 0·45 (95 % CI 0·45, 0·46) and 1·30 (95 % CI 1·27, 1·33), respectively. The median (interquartile range) daily intake of total dietary Fe, Fe from animal sources and Ca was 11·9 (9·3–14·7), 0·5 (0–1·1) and 383·9 (187·4–741·2) mg, respectively. Ninety-nine per cent (n 7602) of women had total daily dietary Fe intake below the RDA of 27 mg and 90·1 % (n 6880) of women had daily dietary Ca intake below 1200 mg. The mean (sd; range) gestational age at enrolment in the study was 21·2 (3·5; 8·4–27·0) weeks and for maternal age was 25·2 (5·1; 13·5–45·5) years. Baseline and demographic characteristics are presented in Table 1.
Table 1 Basic characteristics of the study participants: HIV-negative pregnant women recruited from nine public health centres in Dar es Salaam, Tanzania, from August 2001 to July 2004

The mean (sd) birth weight among the cohort was 3143·5 (493·9) g, with 441 (6·2 %) of births being LBW (<2500 g). The mean (sd) gestational age was 39·6 (2·9) weeks with 1100 (14·9 %) preterm births (<37 weeks) and 298 (4 %) extreme preterm births (<34 weeks). There were 241 (3·1 %) stillbirths and 175 (2·4 %) neonatal deaths.
The relationships between total Fe intake and adverse birth outcomes and neonatal mortality are presented in Table 2. Total dietary Fe intake was not associated with prematurity or severe prematurity. Dietary Fe intake was associated with reduced risk of stillbirth in all upper quartiles (test for trend over quartiles, P=0·010). There was no significant association between total dietary Fe intake and the risk of LBW, small for gestational age or neonatal mortality.
Table 2 Total dietary iron intake in relation to adverse birth outcomes and neonatal mortality in HIV-negative pregnant women recruited from nine public health centres in Dar es Salaam, Tanzania, from August 2001 to July 2004

RR, relative risk; ref., reference quartile.
* Adjusted for maternal education level, maternal age, BMI, parity, wealth, energy intake, baseline Hb level and treatment regimen.
Dietary animal Fe intake from meat, fish and poultry sources was assessed. The upper quartile means the one with highest intake (i.e. quartile 4) and the comparison or reference group is the lowest quartile. Dietary animal Fe intake was significantly associated with reduced risk of preterm birth: compared with the lowest quartile, women in the upper quartile were 0·75 times as likely to have preterm birth (95 % CI 0·65, 0·86; test for trend over quartiles, P<0·001). Similarly, comparing women in the highest and the lowest quartile of dietary animal Fe intake, the RR (95 % CI) of extreme preterm birth was 0·67 (0·51, 0·90; test for trend over quartiles, P=0·004). Intake of dietary animal Fe was inversely related to the risk of neonatal mortality; the adjusted RR (95 % CI) of neonatal mortality in the upper two quartiles was 0·62 (0·42, 0·91) and 0·51 (0·33, 0·77), respectively, while in the second lowest quartile it was 0·69 (0·46, 1·03). Dietary animal Fe intake was not significantly associated with reduced risk of LBW, small for gestational age or stillbirth (Table 3).
Table 3 Dietary animal iron intake in relation to adverse birth outcomes and neonatal mortality in HIV-negative pregnant women recruited from nine public health centres in Dar es Salaam, Tanzania, from August 2001 to July 2004
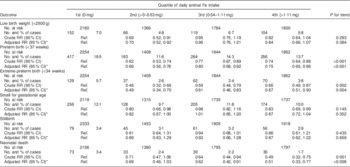
RR, relative risk; ref., reference quartile.
* Adjusted for maternal education level, maternal age, BMI, parity, wealth, energy intake, baseline Hb level and treatment regimen.
The median (interquartile range) daily dietary Ca intake in the first, second, third and fourth quartile was 101·4 (67·0–144·30), 277·9 (230·7–329·0), 529·8 (4491·1–624·4) and 1078·3 (879·1–1426·8) mg, respectively. Dietary Ca intake was significantly associated with reduced risk of preterm birth in all upper quartiles (test for trend over quartiles, P<0·001). It was also significantly associated with reduced risk of extreme preterm birth by an average of 37–41 % (test for trend over quartiles, P=0·002). Dietary Ca intake was also significantly associated with reduced adjusted RR of LBW in the second and third quartiles. Intake of dietary Ca in the upper quartile was significantly associated with reduced risk of neonatal mortality (RR=0·59; 95 % CI 0·37, 0·92) compared with the lowest quartile. There was no significant association between dietary Ca intake and the risk of small for gestational age or stillbirth (Table 4).
Table 4 Dietary calcium intake in relation to adverse birth outcomes and neonatal mortality in HIV-negative pregnant women recruited from nine public health centres in Dar es Salaam, Tanzania, from August 2001 to July 2004

RR, relative risk; ref., reference quartile.
* Adjusted for maternal education level, maternal age, BMI, parity, wealth, energy intake, baseline Hb level and treatment regimen.
Discussion
Higher daily dietary intakes of Fe and Ca among Tanzanian women were significantly associated with reduced risks of preterm birth, extreme preterm birth and neonatal mortality. Dietary Fe intake also reduced the risk of stillbirth. These two micronutrients did not significantly reduce the risk of being small for gestational age.
Nearly all women included in the study had low daily dietary Fe intake, with a median of less than half the recommended amount in pregnancy (12 mg v. 27 mg). This is alarming considering that study participants resided in areas with high prevalence of malaria and helminthic infections, important causes of Fe deficiency in sub-Saharan African populations. Median daily dietary Ca intake was one-third when compared with the WHO recommended daily intake in pregnancy (384 mg v. 1200 mg)( 15 , 21 ). Despite the vast known advantages of Ca intake in pregnancy, it is not provided as a routine supplement in the prenatal health programme as recommended by the WHO( 15 ). The observed low intakes of Fe and Ca in the study may suggest the possibility of low intakes of other micronutrients that we did not assess. Similar reports of suboptimal intakes of most micronutrients in pregnancy have been presented in other studies( Reference Blumfield, Hure and Macdonald-Wicks 22 , Reference Kamau-Mbuthia and Elmadfa 23 ). Emphasis on interventions that promote intake of a diet rich in nutrients may have a significant impact on maternal nutrition because such a dietary approach is more sustainable and may benefit a woman even before conception. It is therefore not effective enough to underpin supplements uptake and ignore the promotion of a nutrient-rich diet considering that in many developing countries supplements are often provided in advanced pregnancy stages due to late booking at the antenatal clinic.
Mothers with higher dietary Fe intake from animal sources, as opposed to total dietary Fe intake, appeared to carry a significant risk reduction of preterm birth and extreme preterm birth. The direct link between maternal Fe intake and fetal maturity may be due to improved Hb level as a result of adequate Fe intake, which automatically improves fetal growth( Reference Jwa, Fujiwara and Yamanobe 24 ). Recent studies support an association between maternal Fe supplementation and increased birth weight; improved birth weight is more of a linear dose response( Reference Haider, Olofin and Wang 25 , Reference Mwangi, Roth and Smit 26 ). There are limited studies on the association between prenatal dietary Fe and birth outcomes. However, a study in Australia supports the association of a preconception diet rich in nutrients including Fe and reduced risk of preterm birth( Reference Grieger, Grzeskowiak and Clifton 3 ).
Our study showed that higher total dietary Fe intake was protective against stillbirth. This may be due to the association between anaemia and low Fe intake, considering that anaemia in pregnancy has been reported to be a risk factor for stillbirth in a systematic review by Haider et al.( Reference Haider, Olofin and Wang 25 ). To date, there are no effective interventions in place to prevent either stillbirth or preterm birth. Thus, it is vital to evaluate further the specific roles of Fe and other micronutrients in preventing stillbirth and preterm birth.
Fe intake in pregnancy has been associated with reduced risk of LBW( Reference Haider, Olofin and Wang 25 , Reference Abdullahi, Gasim and Saeed 27 ). A study in India showed that daily intake of Fe–folic acid supplements during pregnancy increases birth weight by 6·5 g per month( Reference Malhotra, Upadhyay and Bhilwar 28 ). Our study found no relationship between dietary Fe intake in pregnancy and reduced risk of LBW. This may be due to the fact that all women had been provided Fe supplements as per standard of care in Tanzania. Additionally we had very low median and limited variability of daily dietary Fe intake among study participants. The findings in our study are also supported by a study in the UK that showed no association between dietary Fe and birth weight( Reference Alwan, Greenwood and Simpson 10 ). Such inconsistency to support the role of Fe on birth weight may also be due to limitations of 24 h dietary recall assessments, in which failure to recall diet accurately and the chance of consuming a non-typical diet during the day prior to the interview are common.
Increased risk of neonatal mortality was directly associated with decreased intake of dietary animal Fe. It is not clear why the association was observed to be significant for Fe intake from animal sources alone and not also for total dietary Fe. The reason may be due to haem Fe, for which meat, poultry and fish are major sources, being more bioavailable as compared with non-haem Fe( Reference Lopez and Martos 29 ). Such observation should open a way forward to explore the importance of Fe from animal sources and hence to encourage its intake among pregnant women in developing countries. To the best of our knowledge, the present study is the first to assess dietary Fe and the risk of early child survival. However, a study in Indonesia reported that Fe–folic acid supplementation in pregnancy reduces the risk of early neonatal deaths( Reference Titaley, Dibley and Roberts 30 ). The biological relationship on this may be linked with the beneficial effects of Fe and folic acid use in pregnancy on risk reduction of preterm birth and LBW( Reference Zeng, Dibley and Cheng 31 ). Preterm birth and LBW are reported to be important causes of neonatal death in developing countries( Reference Ngoc, Merialdi and Abdel-Aleem 32 , Reference Yasmin, Osrin and Paul 33 ). Typically study participants are provided with Fe supplements in the antenatal clinic, although compliance with the supplements is variable given gastrointestinal adverse effects( Reference Hyder, Persson and Chowdhury 34 ). The specific benefits of higher dietary Fe intake were noted in spite of women receiving prenatal supplements at the initiation of antenatal clinic visits. Therefore, the beneficial role of dietary Fe intake on pregnancy outcome should not be underestimated.
Ca is known as one of the vital micronutrients for the pregnant woman and her growing fetus. Yet, the role of Ca intake in pregnancy in relation to birth outcomes is not clear, with conflicting results on its advantages and risk reduction of LBW and preterm birth( Reference Buppasiri, Lumbiganon and Thinkhamrop 14 ). Our present study showed dietary Ca intake was significantly associated with reduced risk of both preterm birth and extreme preterm birth. This is also supported by Ramakrishnan et al. in their meta-analysis review of Ca supplementation( Reference Ramakrishnan, Imhoff-Kunsch and Martorell 35 ). The role of prenatal Ca intake in relation to reduced risk of preterm birth may be associated with its function in supporting fetal growth and maturity. This may also explain the significant association observed in our study between higher dietary Ca intake and reduced risk of neonatal mortality.
Despite low median daily dietary Ca intake among study participants, dietary Ca intake was borderline significantly associated with reduced risk of LBW. This may agree with a study in Iran that showed the association between maternal Ca intake and increased birth weight( Reference Khoushabi and Saraswathi 36 ). The association is particularly clear when Ca intake reaches dietary recommendation levels( Reference Sabour, Hossein-Nezhad and Maghbooli 37 ), but the latter was not the case in our study. The advantage of Ca intake to the human body also depends on optimal levels of vitamin D. Our study’s ability to determine multiple interaction effects among different micronutrients and vitamins in relation to birth outcomes and early child survival was limited. Since the mean amounts of daily dietary Fe and Ca intakes were very low in our study, their role in reducing risks of LBW, preterm birth, small for gestational and neonatal mortality may have been significantly higher than what we observed if it was in a population with adequate intake of these micronutrients. Furthermore, limitations of dietary intake studies, particularly imprecise estimates of nutrient intakes and fewer numbers of times to interview women for 24 h recall, should not be ignored when evaluating nutritional net benefits. However, these limitations contribute to random misclassification of dietary nutrient intakes, which tends to bias results towards the null rather than present associations that are not real.
Conclusion
Daily dietary Fe and Ca intakes among Tanzanian pregnant women in Dar es Salaam were very low compared with the WHO recommended levels. We determined that dietary Fe and Ca were associated with reduced risk of low preterm birth, stillbirth and neonatal mortality. Dietary micronutrients in pregnancy may be vital, particularly in developing countries where indicators of maternal and child health are worse. Improvement of women’s diet quality during gestation is likely to improve the risks of adverse birth outcomes. Further research on dietary intervention is needed to assess the effects of individual micronutrients, preconception and during gestation, in relation to pregnancy and early child outcomes.
Acknowledgements
Acknowledgements: The authors sincerely thank the women who participated in the study and the project coordinator, physicians and research assistants. Financial support: This work was supported by the National Institute of Child Health and Human Development (NICHD; grant number R01 37701) and the National Institutes of Health (NIH) Fogarty International Center programme. Conflict of interest: None. Authorship: D.M. and W.F. conceived the idea and wrote the first draft of the manuscript. E.L. and E.H. were responsible for data management and assisted in data analysis. All authors participated in data interpretation, review and approved the final manuscript. Ethics of human subject participation: Independent institutional review boards at Muhimbili University of Health and Allied Sciences and the National Institute for Medical Research (Tanzania) and the Harvard School of Public Health (USA) approved the study protocol.







