Published online by Cambridge University Press: 04 November 2024
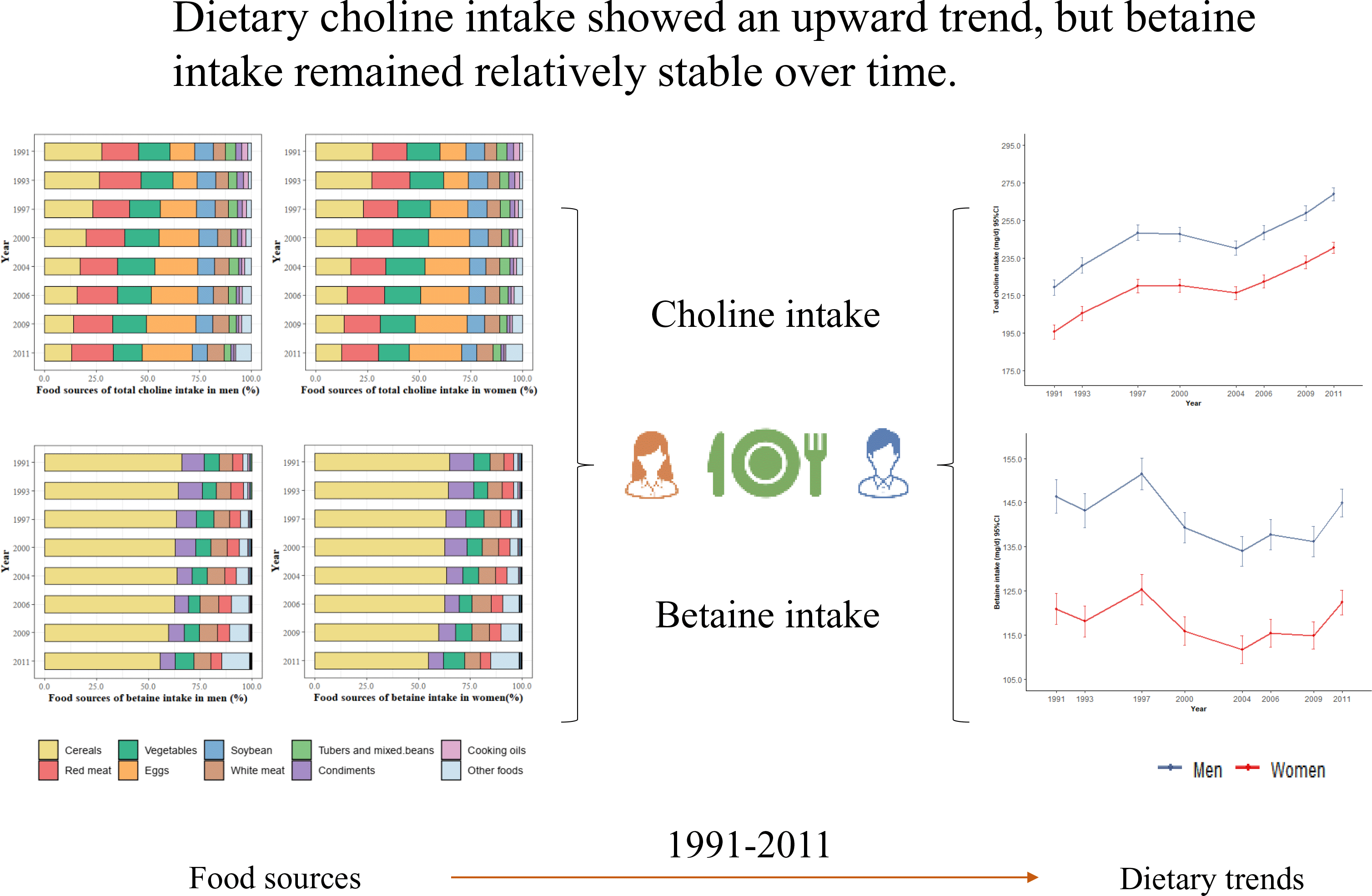
Choline and betaine are important in the body, from cell membrane components to methyl donors. We aimed to investigate trends in dietary intake and food sources of total choline, individual choline forms and betaine in Chinese adults using data from the China Health and Nutrition Survey (CHNS) 1991–2011, a prospective cohort with a multistage, random cluster design. Dietary intake was estimated using three consecutive 24-h dietary recalls in combination with a household food inventory. Linear mixed-effect models were constructed using R software. A total of 11 188 men and 12 279 women aged 18 years or older were included. Between 1991 and 2011, total choline intake increased from 219·3 (95 % CI 215·1, 223·4) mg/d to 269·0 (95 % CI 265·6, 272·5) mg/d in men and from 195·6 (95 % CI 191·8, 199·4) mg/d to 240·4 (95 % CI 237·4, 243·5) mg/d in women (both P-trends < 0·001). Phosphatidylcholine was the major form of dietary choline, and its contribution to total choline increased from 46·9 % in 1991 to 58·8 % in 2011. Cereals were the primary food source of total choline before 2000, while eggs had ranked at the top since 2004. Dietary betaine intake was relatively steady over time with a range of 134·0–151·5 mg/d in men (P-trend < 0·001) and 111·7–125·3 mg/d in women (P-trend > 0·05). Chinese adults experienced a significant increase in dietary intake of choline, particularly phosphatidylcholine during 1991–2011 and animal-derived foods have replaced plant-based foods as the main food sources of choline. Betaine intake remained relatively stable over time. Future efforts should address the health effects of these changes.
These authors contribute equally to this work and are the co-first authors for this paper.
These authors are co-senior authors.
To send this article to your Kindle, first ensure no-reply@cambridge.org is added to your Approved Personal Document E-mail List under your Personal Document Settings on the Manage Your Content and Devices page of your Amazon account. Then enter the ‘name’ part of your Kindle email address below. Find out more about sending to your Kindle. Find out more about saving to your Kindle.
Note you can select to save to either the @free.kindle.com or @kindle.com variations. ‘@free.kindle.com’ emails are free but can only be saved to your device when it is connected to wi-fi. ‘@kindle.com’ emails can be delivered even when you are not connected to wi-fi, but note that service fees apply.
Find out more about the Kindle Personal Document Service.
To save this article to your Dropbox account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Dropbox account. Find out more about saving content to Dropbox.
To save this article to your Google Drive account, please select one or more formats and confirm that you agree to abide by our usage policies. If this is the first time you used this feature, you will be asked to authorise Cambridge Core to connect with your Google Drive account. Find out more about saving content to Google Drive.