CLINICIAN’S CAPSULE
What is known about the topic?
ST-elevation myocardial infarction (STEMI) patients transported by ambulance are at risk for adverse events.
What did this study ask?
What is the impact of transport time on the occurrence of adverse events in the presence of basic life support paramedics?
What did this study find?
Transport time is not associated with a higher risk of adverse events.
Why does this study matter to clinicians?
Largest investigation of adverse events in a Canadian cohort of STEMI patients transported by ambulance.
INTRODUCTION
Approximately 16,000 Canadians die from myocardial infarction every year, and most of these deaths occur outside of the hospital. 1 Primary percutaneous coronary intervention (PCI) has been shown to be superior to fibrinolytic therapy in ST-elevation myocardial infarction (STEMI) patients when performed in a timely manner.Reference de Boer, Barnes and Westerhout 2 The use of prehospital electrocardiograms (ECGs) can reduce treatment delays and improve clinical outcomes,Reference Le May, Dionne and Maloney 3 and are recommended for early STEMI diagnosis.Reference Welsh, Travers and Huynh 4 When a STEMI is diagnosed, the current recommendation is to activate the PCI centre while in transport if the PCI can be performed within 90 minutes from first medical contact (American Heart Association [AHA]/American College of Cardiology [ACC]).Reference Welsh, Travers and Huynh 4 , Reference Armstrong, Bogaty and Buller 5 While it is known that suspected STEMI patients are at risk for clinical adverse events during transport, it is unclear how often these events occur and which complications are most common.Reference Cantor, Hoogeveen and Robert 6 - Reference Ryan, Craig and Turner 9 Neither of these studies distinguished between high risk (i.e., clinically important) and low risk (i.e., clinically minor) adverse events. Furthermore, it is unknown whether longer ambulance transport times (which are often the case in rural areas) are associated with the frequency of clinical adverse events.Reference Bosco and Oandasan 10
In the Chaudière-Appalaches and Québec City regions of Canada, an integrated STEMI program has been used to remotely manage suspected STEMI patients since July 2006Reference Bussieres, Tanguay and Hebert 11 and consistently achieves the recommended 90-minute interval benchmark for PCI.Reference Tanguay, Dallaire and Hebert 12 With implementation of the STEMI program, paramedics are able to wirelessly transmit a prehospital 12-lead ECG to an emergency department (ED) physician at a regional online medical control centre for interpretation. A confirmed STEMI diagnosis results in the regional online medical control contacting an interventional cardiologist at a PCI facility who then decides whether to activate the cardiac catheterization laboratory and receive the patient. Because this system involves bypassing the nearest ED, potentially unstable STEMI patients are transported by basic life support (BLS) paramedics (equivalent to primary care paramedics [PCPs]) for longer periods of time without nursing or physician supervision in person. In Canada, BLS paramedics have a limited scope of practice that includes cardiopulmonary resuscitation, bag-valve-mask ventilation, semi-automatic defibrillation, and esophageal tracheal airway, or Combitube.
The objectives of this study were 1) to establish a clinically relevant classification of complications in STEMI patients based on evidence from the existing literature; 2) to use this classification to determine the frequency of clinical adverse events among suspected STEMI patients in the Chaudière-Appalaches and Québec City regions; and 3) to assess the association between transport time and the development of clinically important and minor adverse events in this population.
METHODS
Study design and setting
We performed a health records review of STEMI patients transported by ambulance to a tertiary cardiology centre. This project was approved by the ethics review board of the Centre intégré de santé et de services sociaux (CISSS) Chaudière-Appalaches and the Québec Heart and Lung Institute–Laval University (IUCPQ-UL), Québec, Canada.
Population studied
All remotely diagnosed STEMI patients transported directly by ambulance to the tertiary cardiology centre for PCI (IUCPQ-UL) between January 2007 and June 2016 were included. Patients with dementia, dialysis, or instability who required immediate medical care were excluded.
EMS system description
According to the Unité de coordination clinique des services préhospitaliers d’urgence (UCCSPU) protocol, the interval time between a first positive ECG and arrival at the PCI centre should be≤60 minutes, and the mean interval between arrival at the PCI centre and balloon inflation in the cardiac catheterization laboratory is 30 minutes.Reference Tanguay, Dallaire and Hebert 12 A detailed description of the prehospital STEMI remote diagnosis procedure and non-PCI hospital bypass has been published previously.Reference Bussieres, Tanguay and Hebert 11
Automated continuous ECGs were performed every 2 minutes in the Chaudière-Appalaches region using the Ortivus system (Danderyd, Sweden), and BLS paramedics received online medical support allowing for the identification of new STEMI cases during transport and rapid rerouting to PCI centres. In the Québec City area, BLS paramedics had to transmit the ECG to UCCSPU before ambulance departure at the pickup location using the Zoll medical system (Chelmsford, MA) and could not benefit from online medical support. During ambulance transport, paramedics verbally communicated clinical data to the UCCSPU nurse, including age, sex, oxygen saturation, pulse, arterial blood pressure, level of consciousness (LOC) according to the Alert, Voice, Pain, Unresponsive (AVPU) scale, distance to hospital, and any deaths that occurred during prehospital transport. Transport time was defined as the duration between departure from the pickup location and arrival at the hospital. The nurse on duty entered all data in the UCCSPU clinical database after each episode of care. Each nurse received training on data entry. Over the study period, a total of 52 nurses entered clinical data provided by BLS paramedics. Due to missing data in the database, author SB used a data extraction sheet containing the UCCSPU clinical data to validate data or complete the missing information for each patient using information from the ambulance paper reports of patients transported to the PCI centre.
Classification of clinical adverse events
A literature review was performed to classify adverse events in the prehospital setting as either “clinically important” or “clinically minor” (see the strategy in Appendix A). Based on relevant studies identified through this search, emergency physicians (FB, PAL, AT, and RF) and the registered nurse (DH) from the research team used clinical criteria to determine operational definitions of adverse events for systolic blood pressure, heart rate, state of consciousness, and arrhythmias. The experts agreed with these definitions by consensus in a meeting. For every patient who experienced an event, the ECG was reviewed by PAL to determine the specific arrhythmia that occurred. The experts agreed that two or more different clinically minor events should be considered equivalent to one clinically important event.
Comprehensive definitions for prehospital clinical events in STEMI patients were found in one study.Reference Ryan, Craig and Turner 9 Based on this limited literature, operational definitions were determined and classified as either “clinically important” or “clinically minor” events for hypotension, bradycardia, desaturation, ventricular tachycardia with pulse, altered LOC, and pulse for atrial fibrillation (AFib). This classification scheme is shown in Box 1. We considered AFib pulse with a heart rate>120 bpm, atrioventricular (AV) block (Mobitz 2 and high degree AV block), ventricular tachycardia with pulse, pulseless ventricular tachycardia/ventricular fibrillation, and asystole or pulseless electrical activity (PEA) to be clinically important events.
Box 1 Classification and definitions of clinically important events and minor events occurring during prehospital transport of STEMI patients
AFib=Atrial fibrillation; AVPU=Alert, Voice, Pain, Unresponsive; LOC=level of consciousness; PEA=asystole or pulseless electrical activity.
Statistical analysis
Patient demographic and clinical characteristics were reported using descriptive statistics. The association between transport time, age, and sex with the occurrence of clinically important events was assessed with a multivariate ordinal logistic regression model. The dependent variable was stratified into three levels according to clinical events defined in Box 1: no event, 1 clinically minor event, or ≥1 clinically important event. Patients who experienced two or more different clinically minor events were placed in the clinically important events group. Clinically minor events occurring to the patients suffering from clinically important events were not reported. Transport time (independent variable) was classified into three levels (0-14 minutes, 15-29 minutes, ≥30 minutes), representing the length of short, medium, and long transport runs (respectively) in the Chaudière-Appalaches and Québec City regions. Age was classified according to the interquartile ranges. Unadjusted and adjusted odds ratios (OR) were reported for all independent variables. All statistical analyses were conducted using SAS University Edition. 13
RESULTS
Patient characteristics
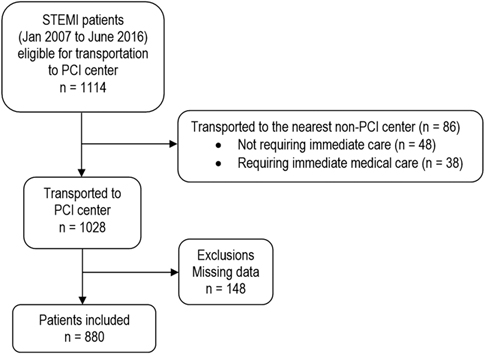
A total of 1,114 STEMI patients were eligible for transportation to PCI centre between 2007 and 2016 (Figure 1). Eighty-six patients were not included in our cohort because 48 of them were transported to the nearest non-PCI centre for non-medical reasons, and 38 required immediate medical care. The non-medical reasons were a borderline STEMI diagnosis (20 patients), unjustified BLS paramedic decision (9), dementia (5), very old age (4), decision made by the emergency physician (4), late ECG transmission (2), trauma (1), blocked road (2), and palliative care (1). For the remaining 38 patients who experienced a total of 40 clinically important events, the nurse suggested to the BLS paramedic to transport the patient to the nearest non-PCI centre for instability reasons: severe hypotension (systolic blood pressure<80 mm Hg; 14), Mobitz 2 and high degree AV block (12), ventricular fibrillation without spontaneous return to alert (8), altered LOC at P or U (3), pulmonary embolism (2), and AFib>120 (1). Two of these patients suffered from two and three different clinically minor events. As a result, 880 STEMI patients were transported by ambulance to the IUCPQ.
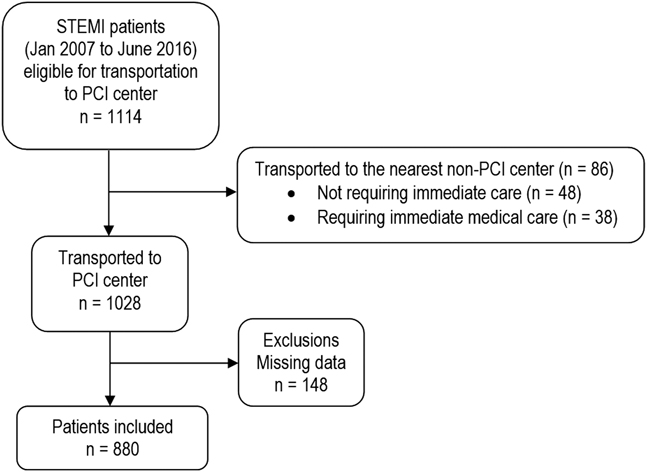
Figure 1 Flow diagram of included patients.
Characteristics of the study population are described in Table 1. STEMI patients were predominantly male (73.9%) with a mean age of 65±13 years. Most patients were from the rural Chaudière-Appalaches, Portneuf, and Baie-Saint-Paul regions (80%). Among these patients, 230 (21.1%) were routed directly to the IUCPQ, whereas 650 patients (73.9%) were diverted to the IUCPQ after remote interpretation of the prehospital ECG by an ED physician at the regional online medical control centre. Overall, the first positive ECG to balloon inflation was performed within 90 minutes from their initial positive ECG for 816 patients (97%), considering that the transportation time was available for 841 patients.
Table 1 Population characteristics
Note: Transportation time was available for 841 patients only.
IQR=interquartile range; SD=standard deviation.
Clinical adverse events
Of the 880 STEMI patients transported by BLS paramedics, 18.5% (163/880) experienced 197 clinically important events, and 12.2% (107/880) experienced 115 clinically minor events during transport (Table 2). Overall, 30.7% (270/880) of patients suffered a clinical adverse event. The most common clinically important events were severe hypotension (systolic blood pressure<80 mm Hg; 5.8%), ventricular tachycardia/ventricular fibrillation (5.1%), altered LOC (P or U) (3.3%), ventricular tachycardia with a pulse (2.4%), and AV block (2.6%). The clinically minor events observed most frequently were mild bradycardia (heart rate of 40-49 bpm; 5.3%), mild hypotension (systolic blood pressure: 80-89 mm Hg; 4.8%), and mild desaturation (80%-89%; 0.8%). All patients suffering from ventricular tachycardia/ventricular fibrillation were successfully resuscitated with semi-automated defibrillation. There were no deaths recorded during prehospital transport. Overall, 40 (4.5%) patients suffered greater or equal to two clinically important events, 32 (3.6%) patients experienced two clinically important events, and 7 (0.8%) and 1 (0.1%) suffered from three and four events, respectively.
Table 2 Frequency of clinically important and minor events
Note: Some patients experienced more than one clinical event.
AFib=atrial fibrillation; LOC=level of consciousness; AVPU=Alert, Voice, Pain, Unresponsive; PCI=percutaneous coronary intervention; STEMI=ST-elevation myocardial infarction.
To assess the impact of transportation time, age, and sex on the incidence of clinically important and minor events, a multiple ordinal logistic regression was performed (Table 3). The model initially included a comorbidity variable, which took into account patients suffering from greater or equal to two clinically important events. However, because the number of patients (40) who suffered from two or more clinically important events was too small and resulted in an unstable OR, the variable for comorbidity was removed from the model. Transport time was not associated with clinical events (global p-value=0.19). Ages 74-97 were found to be statistically significant at the 0.05 level when controlling for transportation time and sex (p=0.03).
Table 3 Ordinal logistic regression of clinically important and minor events
CI=confidence interval; OR=odds ratio.
DISCUSSION
In this study, we classified clinical adverse events in STEMI patients as either “important” or “minor,” based on expert opinion and the published literature. The occurrence of these adverse events was common in our study population with 30.7% of STEMI patients experiencing at least one event during transport, with more than half of the events being classified as clinically important. Furthermore, we observed that STEMI patients with longer transport times to the PCI centre did not experience more clinical events compared to patients with shorter transport times. However, clinical events were more frequent in the older age group (74-97), which could mean that these patients are more at risk from clinical events, regardless of the transportation time. Our findings demonstrate that rural STEMI patients can be safely transported by BLS paramedics over long ambulance runs (≥30 minutes).
A prehospital diagnosis of STEMI and direct transport to a PCI centre while bypassing non-PCI hospitals is a well-established strategy for reducing patient contact-to-balloon times.Reference Camp-Rogers, Dante and Kontos 14 - Reference Fosbol, Granger and Jollis 16 Although most studies have focused on the accuracy of prehospital diagnosis and the duration of transport to PCI, the safety of prolonged transport of rural STEMI patients by BLS paramedics has not been adequately evaluated. To our knowledge, four Canadian studies performed in Ontario have described adverse events occurring during prehospital transport of STEMI patients in urban and suburban settings. A pilot study conducted by Cantor et al. in Ontario concluded that suspected STEMI patients could be safely and effectively transported directly to primary PCI by paramedics without advanced care training.Reference Cantor, Hoogeveen and Robert 6 In that study, 1 of 134 patients developed a rapid atrial flutter during transport that required Advanced Care Paramedic (ACP) skills, 1 patient had ventricular fibrillation, and 5 patients had transient hypotension, for a total of 7 (5%) clinical adverse events.Reference Cantor, Hoogeveen and Robert 6 In the second study, which was conducted by Ryan et al., 487 STEMI patients were transported by ACPs to a PCI centre or to a non-PCI ED with an interfacility transfer to a PCI laboratory.Reference Ryan, Craig and Turner 9 The authors reported an overall clinical event rate of 27%, which is higher than the clinically important events rate that we reported (18.5%). In the third study, STEMI patients were transported by PCPs to either the closest non-PCI centre or to a PCI centre, with an optional ACP rendezvous. Three patients (3%) experienced a clinically important event (ventricular fibrillation) in the prehospital setting.Reference Ross, Alsayed and Turner 8 In the fourth study, 361 STEMI patients were transported by PCPs to a PCI centre.Reference Kwong, Ross and Turner 7 In a STEMI bypass guideline that was implemented, PCPs have to request an en route ACP-rendezvous to be authorized to transport unstable patients (heart rate<50 or ≥120, systolic blood pressure<80 mm Hg, or ventilation required). In addition to the 119 unstable patients, 8 stable patients experienced a cardiac arrest under the care of the paramedics, which represented an overall clinical event rate of 35%.
In our cohort, the most common clinically important events were severe hypotension (5.8%) and ventricular tachycardia/ventricular fibrillation (5.1%). All patients were successfully resuscitated prior to their arrival at the PCI centre, suggesting that extended transport of mainly rural STEMI patients can be managed by BLS paramedics. It is unlikely that most of the clinical events we observed in our study would have been managed differently by ACPs, with the possible exception of advanced interventions such as external pacemakers for patients with Mobitz 2 and complete AV block or high degree AV block (n=23), intravenous fluids for patients with severe hypotension (n=51), or manual cardioversion for patients with ventricular tachycardia with a pulse (n=21). However, it is unknown whether the benefits of these advanced interventions would offset the potential harm that may occur with delayed transport to the PCI centre. Thus, we believe that STEMI patients benefit more from timely PCI access rather than from a broader range of prehospital interventions.
In Canada, access to primary PCI within recommended time frames is variable; approximately 64% of patients ages 40 and older are ambulance transported to a PCI facility within 60 minutes.Reference Patel, Tu and Waters 17 When a STEMI is diagnosed in the prehospital setting, a bypass of the nearest ED requires potentially unstable STEMI patients to be transported by BLS paramedics for longer periods of time without nursing or physician supervision in person. The results from our study demonstrate that longer transport times for rural patients do not increase the risk of clinical adverse events. Therefore, our study reports that prehospital STEMI triage for primary PCI should be extended to regions that have few or no paramedics with advanced care training, a conclusion that was also drawn by Cantor et al.Reference Cantor, Hoogeveen and Robert 6
There is considerable variability in EMS systems across Canada with respect to training, scope of practice, management, private versus public financing, air medevac capacity, and other factors related to prehospital care. STEMI patients are usually transported to the nearest hospital by paramedics who may not have access to ECG interpretation services in the ambulance. In the province of Québec, the transfer of STEMI patients to a PCI hospital requires an in-hospital acute care nurse or physician. 18 For rural hospitals with limited resources, this may significantly limit the ability of health care providers at the facility to respond to other medical conditions requiring emergency care.Reference Welsh, Travers and Huynh 4 However, this population is more likely to have a longer ischemic time, may be more unstable, and need different interventions. As a consequence, a study should be performed to determine the safety of interfacility transports by PCPs with this subset of patients.
Strengths and limitations
This study is subject to the known limitations of health records review, which is subject to non-differential information bias. A major limitation was the inability to link to hospital records and patient outcomes. We were unable to evaluate adverse events that may have occurred shortly after hospital arrival. For 38 patients (4.3%) who experienced a total of 40 clinically important events, the nurse had suggested that BLS paramedics transport the patient to the nearest non-PCI centre for instability reasons, which may have introduced a selection bias. Although the treatments administered by BLS paramedics were captured in the ambulance reports, we were unable to use these data in the analysis due to a large amount of missing values. In addition, continuous monitoring of patient vital signs and ECGs was not available for those patients transported in the Québec City region. There was the potential for misclassification of arrhythmia types due to only one observer reviewing the ECGs. Despite these limitations, this study also has a number of strengths. The clinical data extracted from a medico-administrative database were validated with ambulance reports to improve data validity. Additionally, this study represents the largest investigation of clinical adverse events in a Canadian cohort of STEMI patients transported by ambulance.
CONCLUSIONS
Our study demonstrates that transport time is not associated with clinical adverse events in rural STEMI patients who are transported by BLS paramedics. Advanced age was associated with adverse events. Although clinical events were common, there were no deaths recorded during prehospital transport. Further research is needed to determine long-term outcomes in patients who experience clinically important events during ambulance transport. Nevertheless, the results from our study indicate that a prehospital STEMI diagnosis by BLS paramedics followed by triage for primary PCI is safe.
Acknowledgements: We thank Stéphane Turcotte for his assistance with statistical analysis for this study.
Competing interests: None declared.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/cem.2018.383