Introduction
Coronavirus disease 2019 (COVID-19) caused by the SARS-CoV-2 virus has become a global health threat [Reference Guan1–Reference Chen3]. More than half a year after the roll-out of highly effective vaccines against COVID-19, the pandemic remains difficult to control [4].
COVID-19 can be regarded as one of the influenza-like illnesses (ILIs) because it causes upper respiratory symptoms like seasonal influenza and its severity is mild in most cases [Reference Pastor-Barriuso5–Reference Matsunaga7]. However, there are several distinctive characteristics which differentiate COVID-19 from other ILIs.
First, COVID-19 is more likely to result in severe illness and death than other ILIs do. Previous studies suggested that the infection-fatality rate of COVID-19 was about 10 times higher than that of seasonal influenza [Reference Pastor-Barriuso5, Reference van Asten8]. Although patients may recover with only mild symptoms, COVID-19 infection should be another important cause of excess mortality [Reference Vestergaard9].
Second, the transmission dynamics of COVID-19 is quite different from other ILIs, in that pre- and asymptomatic transmission is more common than for other ILIs [Reference Byambasuren10–Reference Ganyani12]. Additionally, both incubation period and infectious period of COVID-19 were regarded as longer than those of other ILIs [Reference Backer, Klinkenberg and Wallinga13, Reference Chun, Baek and Kim14]. These facts suggest that COVID-19 required a longer duration of isolation as a countermeasure in order to slow down its spread.
Presumably, we need to strengthen our isolation policy in order to prevent further spreading of COVID-19 due to the reasons mentioned above. However, at the same time, we have to consider the societal burden of such interventions including productivity loss because its appropriate duration should be determined by a kind of trade-off between disease prevention effect and societal loss.
At the early stage of the pandemic, the Japanese government determined the duration of isolation for COVID-19 patients as two weeks [15], following the recommendation published by World Health Organization (WHO), Centers for Disease Control and Prevention (CDC) and other organisations [16–18]. This recommendation was updated to ‘10 days after symptom onset, plus at least 3 additional days without symptoms’ in June 2020 [15], based on the updated recommendation published by WHO and other organisations [16–18].
However, these recommendations were defined based on clinical insights. It would be relevant to try and define the duration of isolation with clinical, economic and societal aspects taken into consideration because such long duration of isolation may present a substantial burden for the patients.
At present, there is scarce evidence about the socio-economic burden imposed by the isolation of COVID-19 patients. The few previous studies examining the burden caused by isolation focused on narrow psychological impact [Reference Habtamu19–Reference Peçanha21]. The main objective of the present study is to estimate its burden in a way that it might inform health economic evaluation and policy making from a societal perspective.
Methods
Settings
We conducted an online questionnaire survey recruiting people who had been diagnosed with COVID-19 or other ILIs at any time between 1 October 2019 and 28 February 2021 in Japan. Most of the 302 respondents had already recovered but 12 participants had symptoms at the time of the survey. The participants were voluntarily and randomly recruited from registrants of NEO MARKETING INC, a Japanese marketing research company. The participants were asked to provide information on the latest episode of isolation due to having ILIs during the study period and stratified them into (a) COVID-19 group and (b) other ILIs group. We defined ILIs as these diseases diagnosed by physicians: COVID-19, seasonal influenza, adenovirus infection, RSV infection, hand, foot and mouth disease, pertussis and other common colds. We did not use the definition of ILI [22] because asymptomatic infection is common in COVID-19 and other ILIs, in which case not symptoms, but diagnoses provide the rationale for isolation. The respondents had to be at least 20 years old, the legal age for adulthood in Japan at the time of the study. Informed consent was given before the start of the survey.
Statistical analysis
We collected data on sex, age, number of household members, education level, household and individual income per month, duration of symptoms and isolation and health-related quality of life (HRQoL) at the time of questionnaire survey. As for HRQoL, we used the 15-D questionnaire [Reference Sintonen23] to estimate HRQoL value at the time the survey was conducted. The questionnaire assesses the 15 dimensions of HRQoL by each of 15 questions (mobility, vision, hearing, breathing, sleeping, eating, speech, excretion, usual activities, mental function, discomfort and symptoms, depression, distress, vitality and sexual activity). We can obtain HRQoL value between 0 and 1 as the sum of the scores of 15 dimensions. Categorical variables were presented as absolute number and percentage, continuous variables as median and interquartile range (IQR).
We compared the COVID-19 group with the ‘other ILIs’ group by the matched data using one-to-one, nearest neighbour propensity score matching (caliper = 0.2) [Reference Peçanha21]. Age, sex, education level and presence of underlying medical conditions were adjusted. The primary outcome is duration and productivity loss of isolation evaluated as monetary value; the secondary outcome is HRQoL value. We compared the outcomes (not normally distributed) between two groups using Mann–Whitney U test. Monetary value of productivity loss was calculated by multiplication of duration (days) and wage of each participant (per day equivalent). We transformed Japanese Yen (JPY) to USD as 110 JPY = 1 USD, according to the exchange rate in 2021. The HRQoL values were compared after excluding participants who presented any symptoms at the time of the survey.
Two-sided P values of <0.05 were considered to show statistical significance. All analyses were conducted in the R environment, version 4.0.5 [24].
Ethics approval
This study was approved by the Ethics Committee of the National Center for Global Health and Medicine (NCGM-G-004001-01). Written informed consent was obtained from each participant before starting the survey through an electronic form and the ethical review board approved this form of consent.
Results
Table 1 shows the demographic characteristics of participants. Of the 302 respondents, 138 were classified into COVID-19 group and 164 were other ILIs group. The basic characteristics of two groups were similar (Table 1). The median duration of symptoms (from the onset to the end of symptom presentation) and isolation (from the onset until the end of the isolation period) for the other ILIs group were 7 days each, while those for the COVID-19 group were 15.5 and 17.0 days.
Table 1. Demographic characteristics of the participants
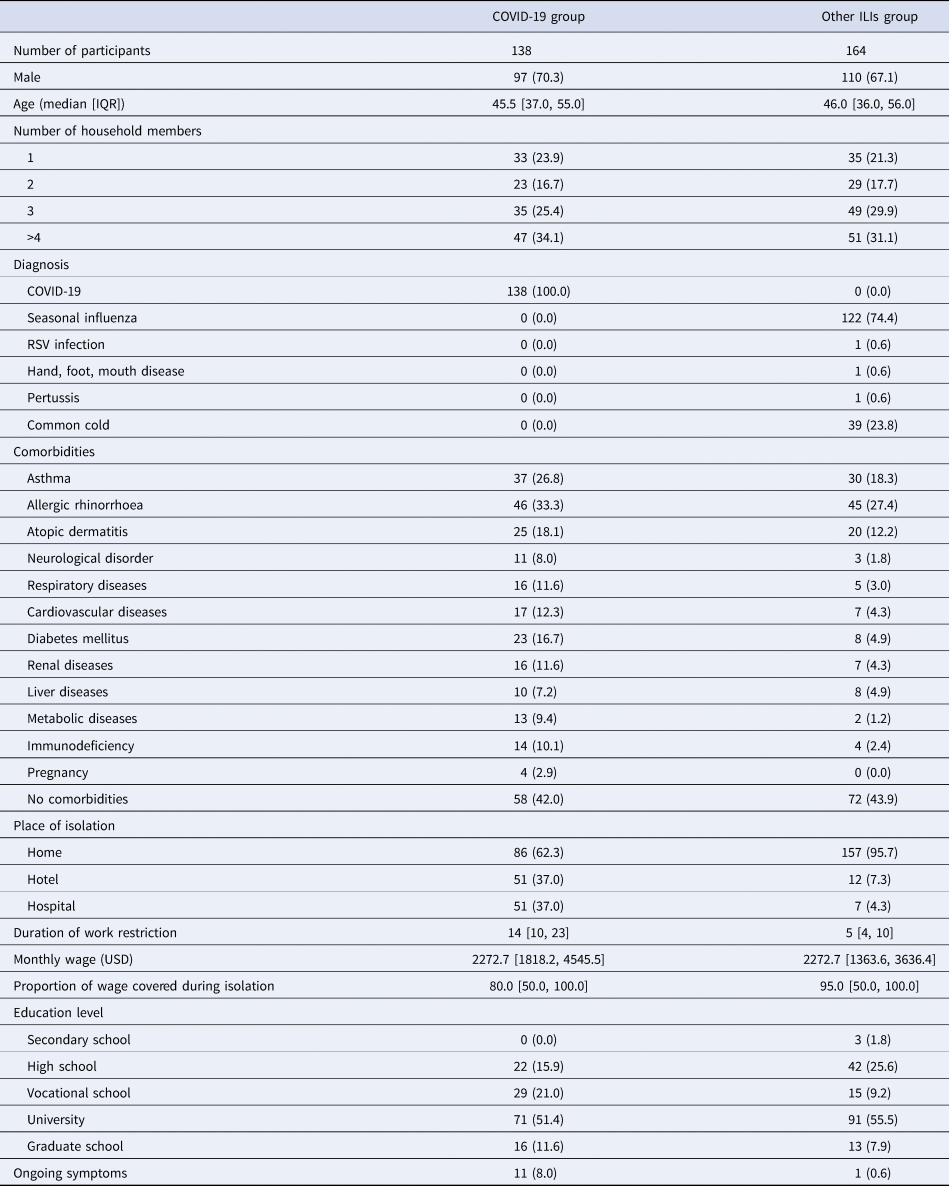
ILI, influenza-like illness; RSV, respiratory syncytial virus; USD, United States Dollar (110 Japanese Yen = 1 USD).
Numbers with brackets represent absolute number and percentage.
Numbers with square brackets represent median value and interquartile range.
Table 2 describes the details of data after propensity score matching. Standardised mean difference larger than 0.1 was regarded as significant imbalance.
Table 2. Demographic characteristics of data after propensity score matching
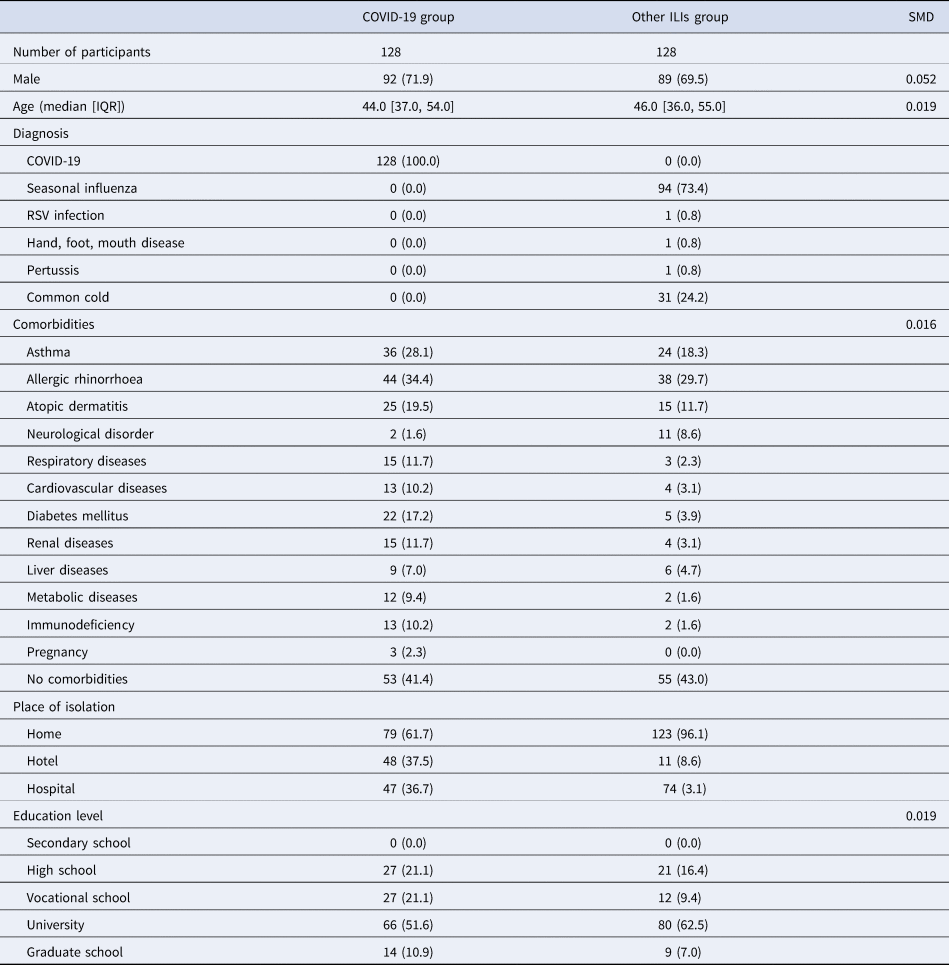
ILI, influenza-like illness; SMD, standardised mean difference; RSV, respiratory syncytial virus; USD, United States Dollar (110 Japanese Yen = 1 USD).
Numbers with brackets represent absolute number and percentage.
Numbers with square brackets represent median value and interquartile range.
Table 3 shows the outcome comparison between the COVID-19 group and the ‘other ILIs’ group. The COVID-19 group showed longer median duration of symptoms (18 vs. 7 days) and isolation (16 vs. 7 days). Productivity loss of isolation due to COVID-19 was greater than that due to other ILIs (1424.3 USD vs. 606.1 USD). The HRQoL value of the COVID-19 group was lower than that of the other ILIs group (0.89 vs. 0.96).
Table 3. Comparison of outcomes between two groups
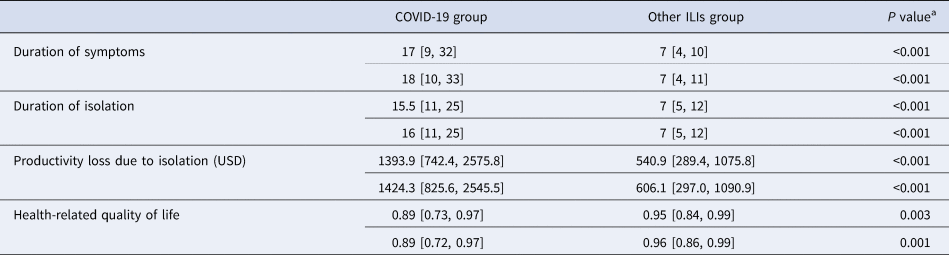
ILI, influenza-like illness; USD, United States Dollar.
Numbers with square brackets represent median value and interquartile range.
Numbers in upper rows represent the results before matching.
Numbers in lower rows represent the results after matching.
a Results of Mann–Whitney U test.
Table 4 shows the difference in each dimension of HRQoL in 15-D questionnaire. While most of 15 dimensions were lower in the COVID-19 group, vision, depression, distress and vitality were not substantially different.
Table 4. Difference in each dimension of health-related quality of life between two groups by matched data
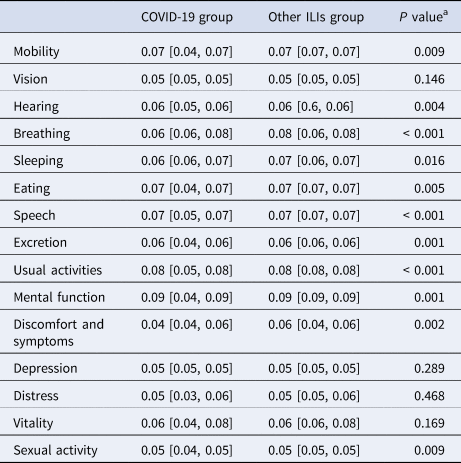
a Results of Mann–Whitney U test.
Figure 1 shows the probability density curve of duration of symptoms and isolation, productivity loss and quality of life at the day of questionnaire survey.
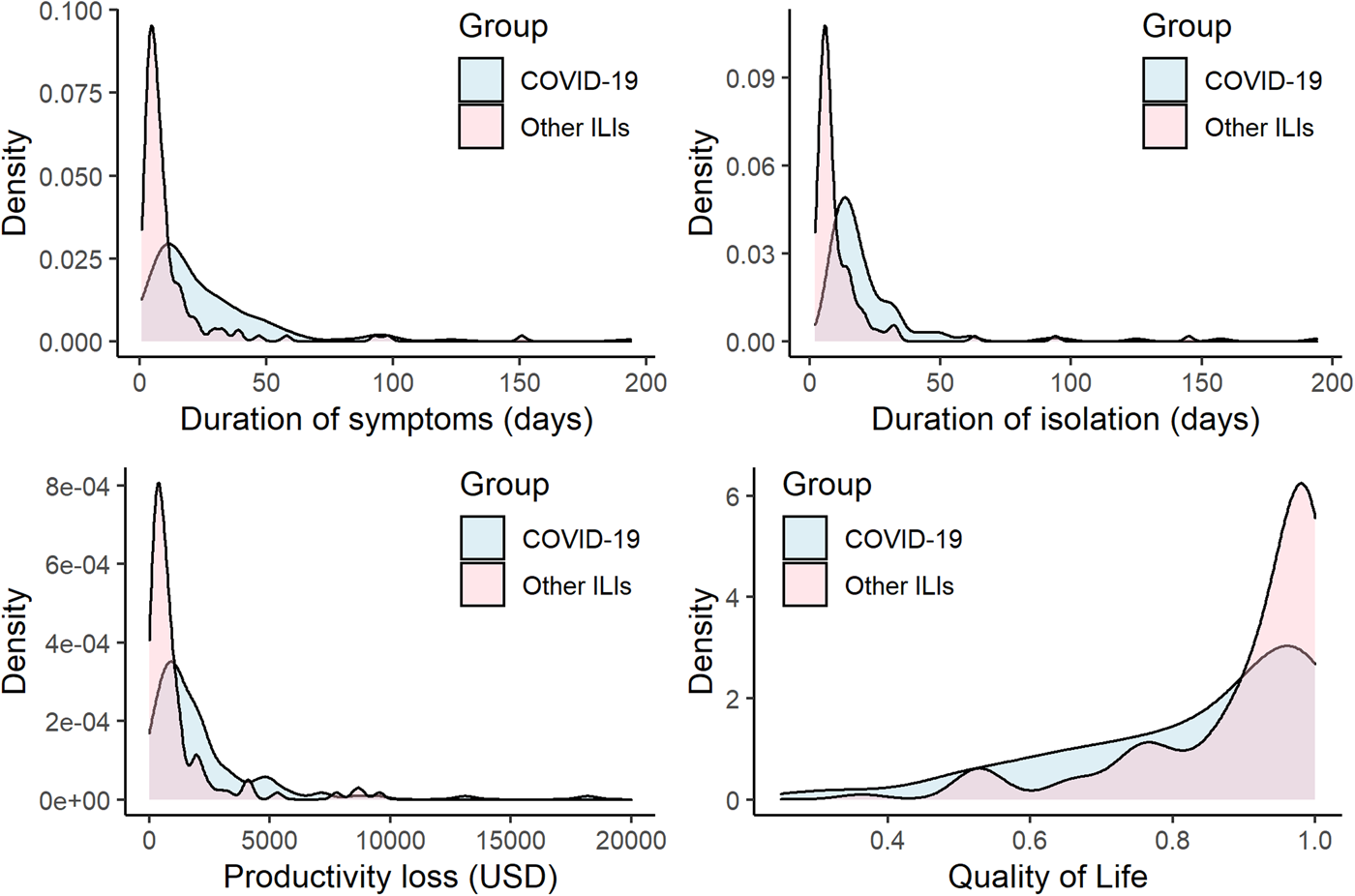
Fig. 1. Probability density curve of duration of symptoms and isolation, productivity loss and quality of life. Top left panel shows duration of symptoms. Top right panel shows duration of isolation. Bottom left panel shows productivity loss. Bottom right panel shows health-related quality of life. ILI, influenza-like illness; HRQoL, health-related quality of life. Blue area represents COVID-19 group and Red area represents other ILIs group.
Discussion
We showed the difference between COVID-19 and other ILIs in relation to the individual HRQoL, economic impact and duration of isolation. As expected, COVID-19 imposes a heavier burden on society than other ILIs do in various aspects. To our knowledge, there are no previous studies which compare the economic impact and duration of isolation between persons infected by SARS-CoV-2 and by other ILIs.
First, the longer duration of isolation comes with greater absenteeism from work. It is noteworthy that the median duration of isolation (16 days by the data after propensity score matching) was longer than 14 days. As described above, its duration in Japan was initially determined as 14 days at the early stage of the pandemic and reduced to 10 days later by the Ministry of Health, Labour and Welfare (MHLW) [15]. The Japanese government also adopted the additional isolation time defined by WHO [16], i.e. ‘plus at least 3 additional days without symptoms (including without fever and without respiratory symptoms)’. This means that longer duration of symptoms will consequently result in longer duration of isolation.
In the ‘other ILIs’ group (excluding COVID-19), the most frequent diagnosis was seasonal influenza (74.4%). The large proportion of seasonal influenza in this group was probably due to the isolation policy specific to Japan [Reference Tsuzuki and Yoshihara25]. The responsibility for defining the duration of isolation for school children infected with seasonal influenza lies with the Ministry of Education, Culture, Sport, Science and Technology, and not the MHLW. This is based on the School Health and Safety Act [26]. This law defines a 5-day isolation period for seasonal influenza with the day of symptom onset as day 0. It is the main cause of the comparatively long isolation period for seasonal influenza in Japan [Reference Tsuzuki and Yoshihara25]. Therefore, the burden caused by isolation due to seasonal influenza in Japan seems heavier than that in other countries, nevertheless, that caused by COVID-19 imposes a heavier burden than other ILIs.
As a result of this longer duration of isolation, the productivity losses should become larger in the COVID-19 group than in the other ILIs group. In addition, our results showed the economic loss from the patients' perspective and as such it represents an underestimate of the societal economic burden. From the societal perspective, productivity losses, arising to employers and other third parties may exceed the sum of individual employee losses, if many employees are simultaneously isolated. Furthermore, in contrast to other ILIs, COVID-19 patients were often isolated in a designated hotel and not at home, especially when the patients have no risk factors of severe diseases and their cohabitants also have no apparent risk factors [15]. Their accommodation fee and professional healthcare personnel costs are covered by the government and these costs should be included in the total costs from a societal perspective. Such cost data were not available and therefore not included here. Additionally, an infection in any household, even if it is a single member of the household, often consigned the whole household to isolation especially if they could not provide additional accommodation to isolate the infected person. Therefore, the number of jointly isolated household members is another important factor to consider when estimating costs.
In short, our results suggest that the longer duration of the isolation period associated with COVID-19 imposed a greater burden than that associated with other ILIs, and it might be even underestimated. The optimal duration of the isolation period for epidemic control should ideally be considered jointly with the socioeconomic consequences of isolation.
Also, after adjusting for the participants' background, there were significant differences in HRQoL value at the day of the survey between the COVID-19 group and the ‘other ILIs’ group (0.89 and 0.96, respectively). This result might suggest that, even if patients were not aware of it, COVID-19 had long-term effect on their psychosocial health status. Although most of the COVID-19 group feel that they have already recovered and have no symptoms, actually they showed lower value of HRQoL on most dimensions of the 15-D questionnaire (Table 4). For instance, these results suggest that some participants of the COVID-19 group had more difficulty with breathing and mental functioning.
Although so-called ‘long COVID syndrome’ or ‘post COVID syndrome’ is not conclusively defined in previous studies [27, Reference Ayoubkhani28], it covers important clinical manifestations that are specific to COVID-19, as compared with other ILIs. Therefore, it increases the additional burden on society. In our survey, more than a half of participants who had COVID-19 infection indicated that their symptom(s) lasts more than 4 weeks. Conversely, only 7.9% in the other ILIs group reported a duration of symptoms longer than 4 weeks. The proportion of patients who reported ‘long COVID syndrome’ in previous studies varies, including between another study in Japan [Reference Miyazato29] and a review of previous studies in other countries [Reference Nalbandian30]. Although our study was not designed to study long-COVID specifically, our estimate is not substantially different from these previous findings [Reference Miyazato29–Reference Roessler31]. Considering this, even after its acute phase, COVID-19 may continue to have a negative impact on HRQoL and productivity, more frequently and longer than other ILIs.
Our study includes several limitations. First, our data were based on an online survey, and therefore requires participants to have basic Internet literacy. That is, participants of our survey might have more interest in their health status and better basic computational skills than the general Japanese population. However, this form of survey was preferred because in the case of COVID-19, minimising contact between the interviewers and the patients is important to contribute to breaking transmission chains.
Second, as already discussed in this section, productivity loss was evaluated only from the participants' viewpoint, and insufficient data are available to inform the broader societal perspective (accommodation fee, healthcare professional personnel, etc.). Third, HRQoL was assessed at the day of the survey and not assessed at different time points over the periods of symptomatic disease and isolation. Note that the 15-D questionnaire does not include a recall period. More elaborate quantitative evaluation of productivity losses and HRQoL remains a subject for future research.
In conclusion, our results showed that COVID-19 imposes a heavier burden in Japan than other ILIs do, not only due to its symptoms but also due to the productivity losses during the longer period of isolation. These findings are preliminary, but could be useful to inform future research and healthcare policy makers to determine the optimal duration of isolation. The health and economic impact of epidemic mitigation through isolation could then be estimated, considering not only the benefits in terms of mitigating the epidemic spread, but also the costs of lost productivity. The challenge will be to identify the economic optimum for society, where the marginal benefits equal the marginal costs of isolating an average infected person for an extra day.
Acknowledgement
We thank all the people who participated in our survey.
Author contributions
Shinya Tsuzuki: conceptualisation, funding acquisition, data curation, formal analysis, methodology, visualisation, project administration, original draft preparation. Norio Ohmagari: funding acquisition, project administration, supervision, review and editing. Philippe Beutels: conceptualisation, methodology, supervision, project administration, review and editing.
Financial support
This research was funded by JSPS KAKENHI (grant number 18K17369), a grant for the National Center for Global Health and Medicine (20A05), Development of a standardized protocol for a UK-Japan cohort study of long COVID, the 2021 Tohoku University-University College London Matching Fund, and the Health and Labor Sciences Research Grant, Research on Emerging and Re-emerging Infectious Diseases and Immunization. PB acknowledges support from the Epipose project from the European Union's SC1-PHE-CORONAVIRUS-2020 programme, project number 101003688, during the conduct of the study.
Conflict of interest
PB reports previous unrelated grants from Pfizer, GSK and the European Commission IMI. The other authors declare no conflicts.
Ethical standards
This study was reviewed and approved by the Ethics Committee of the Center Hospital of the NCGM (NCGM-G-004001-01).
Patient consent
Written informed consent was obtained from each participant before starting the survey through an electronic form.
Permission to reproduce material from other sources
Not applicable.
Data availability statement
The data that support the findings of this study are available upon request to the corresponding author. The data are not publicly available due to privacy or ethical restrictions.








