Introduction
The coronavirus disease 2019 (COVID-19) pandemic is ongoing globally (World Health Organization, 2020). Medical health workers, including medical doctors and nurses, are directly in contact with and treat COVID-19 patients (Zhang, Wang, et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng and Wang2020). They are at a high chance of being infected (Chou et al., Reference Chou, Dana, Buckley, Selph, Fu and Totten2020; Givi et al., Reference Givi, Schiff, Chinn, Clayburgh, Iyer, Jalisi and Davies2020), exposed to long and protracting work time (Zhang, Wang, et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng and Wang2020), and have high levels of distress (Zhang, Wang, et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng and Wang2020). Thus, they are at risk of burnout (Aronsson et al., Reference Aronsson, Theorell, Grape, Hammarstrom, Hogstedt, Marteinsdottir and Hall2017; Zhang, Wang, et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng and Wang2020). Identifying a technique that might help them in managing such distress might be helpful to favor their working activity and maintain their mind−body balance. Relaxation techniques, among the others, seem promising (Pospos et al., Reference Pospos, Young, Downs, Iglewicz, Depp, Chen and Zisook2018). Simple, easy, and practical methods are preferable (Zhang, Wang, et al., Reference Zhang, Wang, Yin, Zhao, Xue, Peng and Wang2020), since medical health workers work wearing medical protective equipment which limits their movement, environmental management, space, and body position.
Relaxation is an individual feeling of calm and ease without tension in body and mind, which occurs minimizing neurological arousal (i.e. a feeling of being physically relaxed) and empowering enthusiastic emotions (such as feeling mentally rested, quiet, cheerful, and restored) (Klainin-Yobas, Oo, Suzanne Yew, & Lau, Reference Klainin-Yobas, Oo, Suzanne Yew and Lau2015). Many techniques can produce relaxation. They include abdominal breathing (Chen, Huang, Chien, & Cheng, Reference Chen, Huang, Chien and Cheng2017), yoga (Pascoe, Thompson, & Ski, Reference Pascoe, Thompson and Ski2017), autogenic relaxation (Hashim & Hanafi Ahmad Yusof, Reference Hashim and Hanafi Ahmad Yusof2011), progressive muscle relaxation (Hashim & Hanafi Ahmad Yusof, Reference Hashim and Hanafi Ahmad Yusof2011; Ozgundondu & Gok Metin, Reference Ozgundondu and Gok Metin2019), Kegel exercise (Huang & Chang, Reference Huang and Chang2020), physical exercise (Silva et al., Reference Silva, Tortelli, Motta, Menguer, Mariano, Tasca and Silveira2019; Yang & Chen, Reference Yang and Chen2018), listening to music (Diri, Çetinkaya, & Gül, Reference Diri, Çetinkaya and Gül2019), tai chi (Wang et al., Reference Wang, Lee, Wu, Benson, Fricchione, Wang and Yeung2014), guided imagery (Flynn, Jones, & Ausderau, Reference Flynn, Jones and Ausderau2016), biofeedback (Aritzeta et al., Reference Aritzeta, Soroa, Balluerka, Muela, Gorostiaga and Aliri2017), cognitive behavior therapy (Buhrman et al., Reference Buhrman, Syk, Burvall, Hartig, Gordh and Andersson2015), and mindfulness therapy (Spadaro & Hunker, Reference Spadaro and Hunker2016), etc. Relaxation not only mitigates negative emotions but also enhances physical and mental well-being and relieves the feeling of stress and muscular tension (Hashim & Hanafi Ahmad Yusof, Reference Hashim and Hanafi Ahmad Yusof2011; Klainin-Yobas et al., Reference Klainin-Yobas, Oo, Suzanne Yew and Lau2015; MacSween, Lorrimer, van Schaik, Holmes, & van Wersch, Reference MacSween, Lorrimer, van Schaik, Holmes and van Wersch2018; Ozgundondu & Gok Metin, Reference Ozgundondu and Gok Metin2019).
As of today, many papers have focused on the emergence of psychological distress and/or mental health in medical health workers during the pandemic (Bao, Sun, Meng, Shi, & Lu, Reference Bao, Sun, Meng, Shi and Lu2020; D'Agostino, Demartini, Cavallotti, & Gambini, Reference D'Agostino, Demartini, Cavallotti and Gambini2020; Kang et al., Reference Kang, Li, Hu, Chen, Yang, Yang and Liu2020; Liu et al., Reference Liu, Yang, Zhang, Xiang, Liu, Hu and Zhang2020; Walton, Murray, & Christian, Reference Walton, Murray and Christian2020; Zhang, Yang, et al., Reference Zhang, Yang, Liu, Ma, Wang, Cai and Zhang2020), but no studies reported on how to relieve such distress via a simple, easy, and practical relaxation technique to be used while wearing medical protective equipment (which cannot be removed during work time). This was the aim of this study. Medical staff who supported hospitals in Wuhan among the pandemic was tested to reach the goal.
Methods
Design, participants, and procedure
A two-step study was conducted (Fig. 1). All participants were 18−60 years and agreed with enrollment in the study. At step 1, a qualitative interview and a quantitative questionnaire survey on common possible relaxation techniques used by medical health workers were proposed to 17 experts (i.e. five nurses and doctors as first-line medical health workers who had severe acute respiratory syndrome − SARS experience in 2003, five psychiatrists, three psychologists, and four neuropsychiatrists who have expertise in relaxation techniques in their clinical settings). Six relaxation techniques were selected: autogenic relaxation (i.e. imagining previous peaceful places followed by developing an awareness of physical sensations) (Hashim & Hanafi Ahmad Yusof, Reference Hashim and Hanafi Ahmad Yusof2011), Kegel exercise (i.e. pelvic-floor exercise which involves repeatedly contracting and relaxing the muscles that form part of the pelvic floor) (Huang & Chang, Reference Huang and Chang2020), progressive muscle relaxation (i.e. tensing and relaxing the muscle groups, typically accompanied by deep breathing) (Hashim & Hanafi Ahmad Yusof, Reference Hashim and Hanafi Ahmad Yusof2011; Ozgundondu & Gok Metin, Reference Ozgundondu and Gok Metin2019), guided imagery (i.e. controlling breathing and visualizing a soothing image) (Flynn et al., Reference Flynn, Jones and Ausderau2016), listening to music (Diri et al., Reference Diri, Çetinkaya and Gül2019), and aerobic exercises (i.e. repetitive movement, such as walking, running, dancing, etc.) (Yang & Chen, Reference Yang and Chen2018). Because COVID-19 is a disease dominantly transmitted through the respiratory system (Zhang, Li, Zhang, Wang, & Molina, Reference Zhang, Li, Zhang, Wang and Molina2020), abdominal breathing was not listed as one of the recommended techniques by our experts. Then, 15 medical health workers who had never experienced psychotherapy training and supporting Wuhan of Hubei Province from Inner Mongolia, Beijing, and Shanxi were recruited from January 21 to 25, 2020, and trained to use these six relaxation techniques. Thereafter, participants were qualitatively interviewed via telephone interviews, and data were quantitatively collected via a survey created ad hoc assessing several dimensions of relaxation technique to identify the most feasible one. As a result, autogenic relaxation and Kegel exercise were recommended by the 15 first-line medical health workers for their working hours.
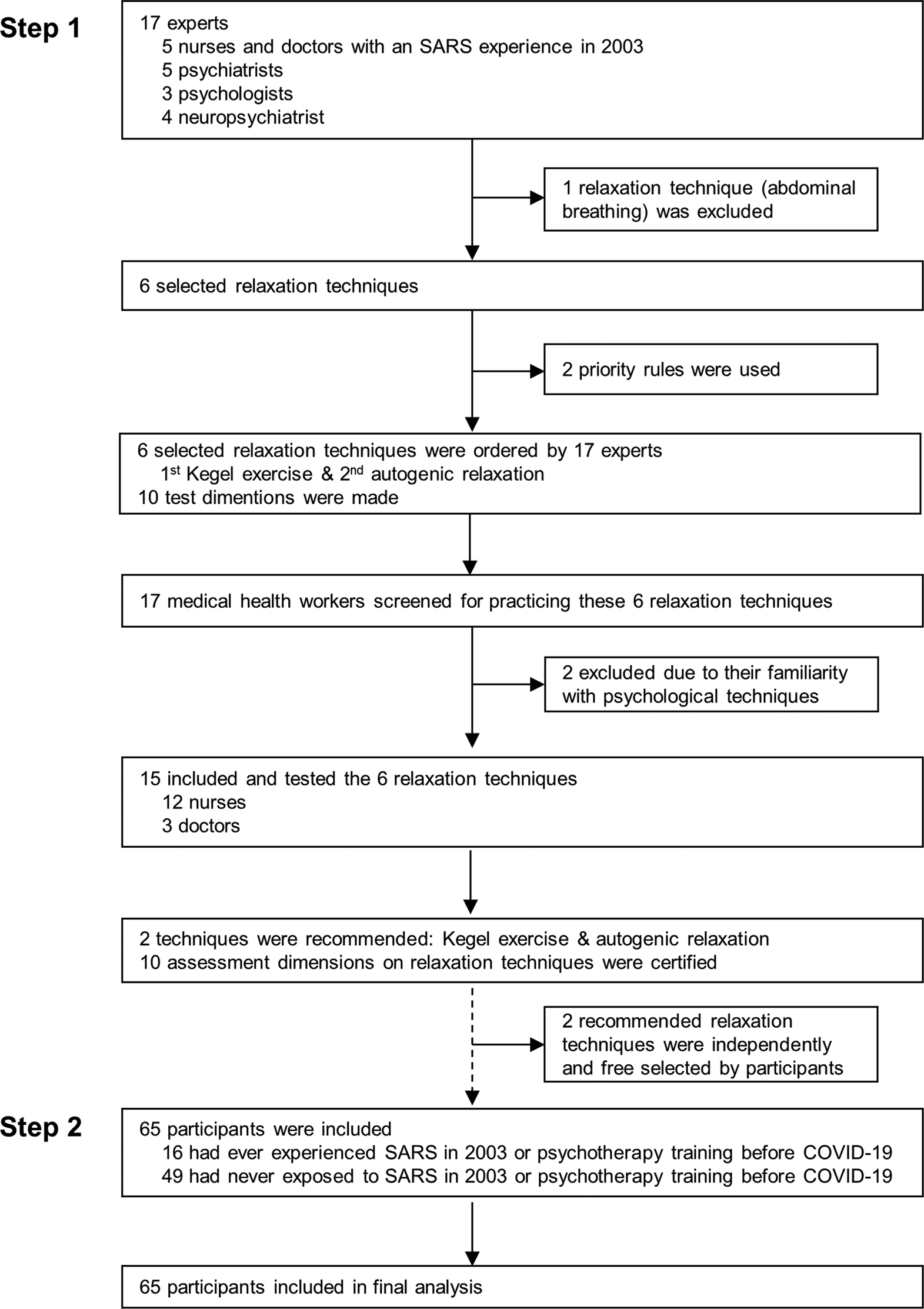
Fig. 1. Study profile.
At step 2, 65 participants (39 of Shanxi, 10 in Beijing, 17 of Inner Mongolia), who were at work from April 10 to May 10, 2020, volunteered to practice autogenic relaxation and Kegel exercise. The instructions for these relaxation techniques were published online at the official WeChat public account of Department of Neurology of Xuanwu Hospital, Capital Medical University, and thus made available for all first-line medical staff. In addition, the online link was also directly sent via WeChat to the 65 volunteers to ensure that they received it and read this material before arriving at Hubei.
Two days after having received the material and being asked to practice autogenic relaxation and/or Kegel exercise for the following 70 days at work, the 65 participants were invited to fill in the online survey created ad hoc evaluating the proposed dimensions of relaxation technique in step 1, aiming to identify the most feasible one. Data were collected anonymously via the Wenjuanxing platform (https://www.wjx.cn/m/73948651.aspx).
Instruments
The online survey was used at step 1 and at step 2 allowed to collect sex, age, marital status, education, psychotherapy before the pandemic COVID-19, participation in the campaign against SARS in 2003. In addition, 10 dimensions, including efficacy, no space, no time, no body position, no environment limitation; easiness to learn, simplicity, convenience, practicality, and acceptance were assessed referring to autogenic relaxation or Kegel exercise. Each dimension was rated on an analogue scale ranging from 0 (not at all) to 10 (maximum). Each subject could use both or one single relaxation technique, according to his/her preference, and was asked to rate each technique that they had used.
In addition, in order to verify which relaxation method was best suited for medical staffs while wearing medical protective equipment or in leisure time in Wuhan of China, the following questions were formulated: ‘which relaxation technique did you prefer while wearing medical protective equipment?’ and ‘which relaxation technique did you prefer during your leisure time among these six relaxation techniques?’.
Statistical analysis
Frequencies were calculated for each dimension for each relaxation technique. Median, interquartile range (IQR), mean, and standard deviation (s.d.) were used to further describe each dimension. The percentage of the preferred relaxation method during leisure time was also determined.
The previous experience on SARS or psychotherapy training before COVID-19 pandemic may affect participants’ choices on the two recommended relaxation techniques, so Chi-square tests were used to compare those who were previously exposed to SARS or psychotherapy and those who had never experienced SARS or psychotherapy concerning the 10 dimensions assessed for autogenic relaxation and Kegel exercise.
Results
Results of step 1
Based on the qualitative interviews, the 17 experts agreed that ‘easily learning by their reading directions on relaxation techniques’ was of the most priority. Based on this, six relaxation techniques were identified: Kegel exercise (17/17), autogenic relaxation (17/17), progressive muscle relaxation (14/17), guided imagery (11/17), aerobic exercise (3/17), listening to music (1/17). Secondly, all experts agreed that ‘no need to pour more energy and attention’ was another priority. Based on this, Kegel exercise (17/17), autogenic relaxation (16/17), progressive muscle relaxation (11/15), guided imagery (10/17), listening to music (2/17), aerobic exercise (1/17), were selected.
The six relaxation techniques were tested among 15 of 17 participants while supporting medical services and wearing medical protective equipment; the two subjects who had experienced psychotherapy were excluded, due to their familiarity with specific psychological techniques. According to the choice of the 15 subjects, Kegel exercise (15/15), autogenic relaxation (15/15), guided imagery (10/15), progressive muscle relaxation (8/15), aerobic exercise (3/15), listening to music (0/15) were selected. In working condition, aerobic exercise was not preferred as 15 participants worried that aerobic exercise might have a risk of breaking medical protective equipment; likewise, listening to music needed specific tools and was not preferable. However, they thought that these two relaxation methods might be good in their leisure time. All recruited participants considered that Kegel exercise and autogenic relaxation were feasible relaxation techniques while wearing medical protective equipment, and 10 dimensions of the assessment of the relaxation techniques were proposed (Fig. 1). The steps on Kegel exercises applied in our study were: 1. To find your pelvic muscles. Assume you are trying to prevent traveling gas. If you've recognized the correct muscles, you'll notice the tightening more in the back of the pelvic region than the front. 2. To flex pelvic floor muscles for 3 to 5 s. 3. To relax pelvic floor muscles for 3 to 5 s. 4. To replicate the contraction−relaxation pattern 8–10 times. After you have grasped the steps, you can practice freely anytime and anywhere without the restriction of position for experiencing self-relaxation. However, it should be noted that, do not habituate Kegel exercises to begin and discontinue your urine flow; do not contract the muscles of your abdomen, thighs, or buttocks; and keep freely breathing among the contraction−relaxation exercises.
Results of step 2
Data from 65 subjects (41 female, 24 male) with a mean age of 38.0 ± 4.1 years (minimum: 32; maximum: 55 years) were collected. They confirmed that they freely and independently tried to select and apply these relaxation techniques to relax when they were not in the handling of the patient's affairs in their medical protective equipment, and admitted that these relaxation techniques to some extent benefited their reducing stress. All participants anonymously completed the online survey. Of them, six were single, 59 married; 19 were doctors and 46 nurses; all had more than 14-year educational level; three had SARS experience in 2003, and 12 were on psychotherapy before the pandemic. Their working experience was of 15.7 ± 3.9 years (from 7 to 30 years).
During working time and while wearing medical protective equipment, more participants considered Kegel exercise better than autogenic relaxation on the 10 dimensions (efficacy: 24 v. 15, no space limitation: 30 v. 4, no time limitation: 31 v. 4, no body position requirement: 26 v. 4, no environment limitation to be done: 30 v. 11, easiness to learn: 28 v. 5, simplicity: 29 v. 7, convenience: 29 v. 4, practicality: 30 v. 14, acceptance: 32 v. 6, Fig. 2), and the scores on the 10 dimensions of Kegel exercise was higher than that of autogenic relaxation (Fig. 3a and 3b). On the contrary, during leisure time, the preferred relaxation technique was autogenic relaxation (46.2%), followed by listening to music (35.2%), and physical exercise (16.9%).
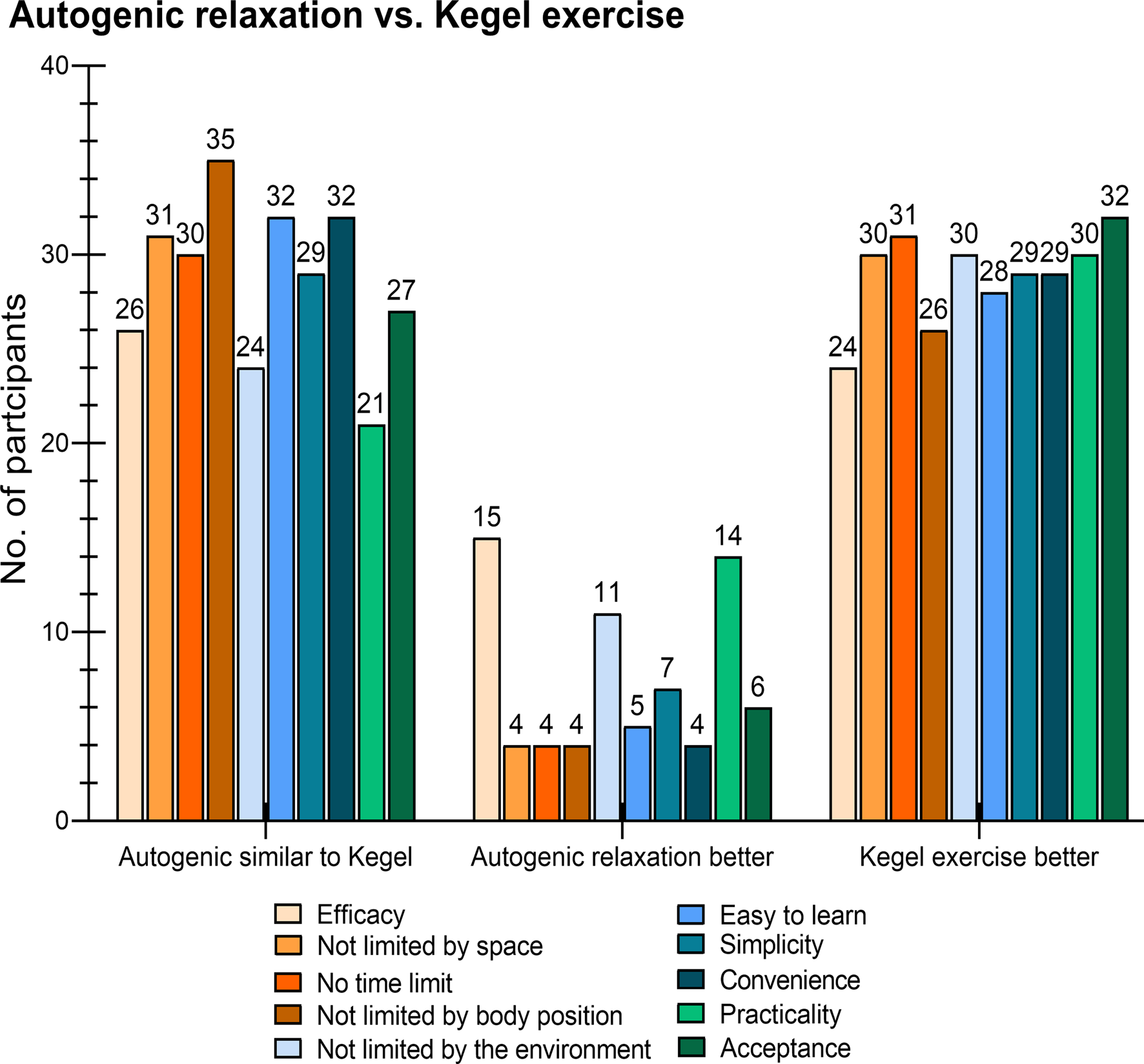
Fig. 2. Frequencies for each dimension of autogenic relaxation and Kegel exercise in 65 participants.
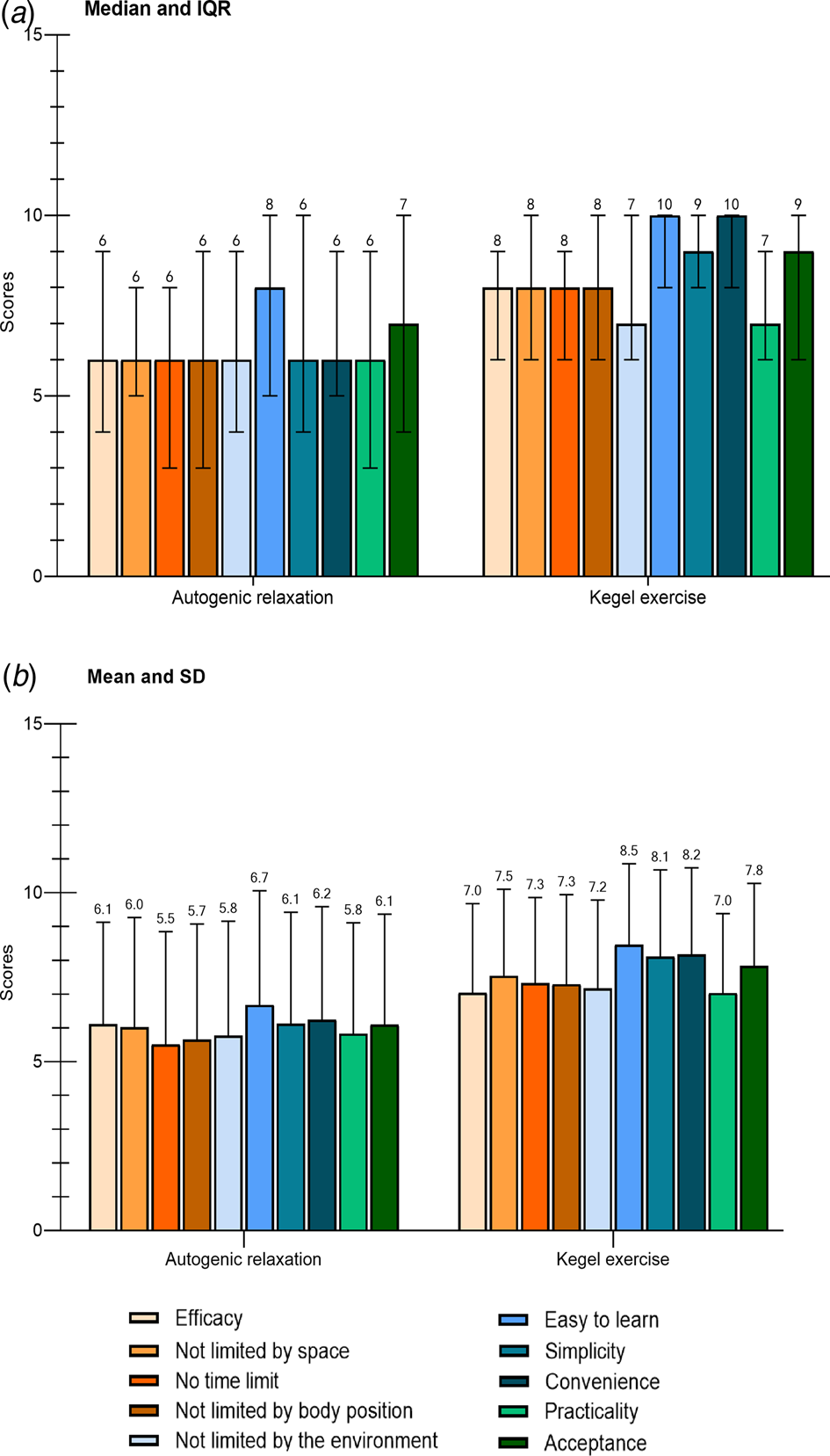
Fig. 3. Scores on 10 dimensions of (a) autogenic relaxation and (b) Kegel exercise in 65 participants. IQR = interquartile range; s.d. = standard deviation.
We further analyzed differences in 10 dimensions of the two selected relaxation techniques between those who had never experienced SARS or psychotherapy before COVID-19 (group 1, n = 49) and those who had exposed to SARS or psychotherapy (group 2, n = 16). Both groups considered that Kegel exercise and autogenic relaxation were not statistically different on all tested dimensions (Table 1).
Table 1. Differences on 10 dimensions of autogenic relaxation and Kegel exercise between participants who had never experienced SARS or psychotherapy training before COVID-19 (group 1) and those who had ever exposed to SARS or psychotherapy (group 2)<TE: Please take care to set shading in the table.>
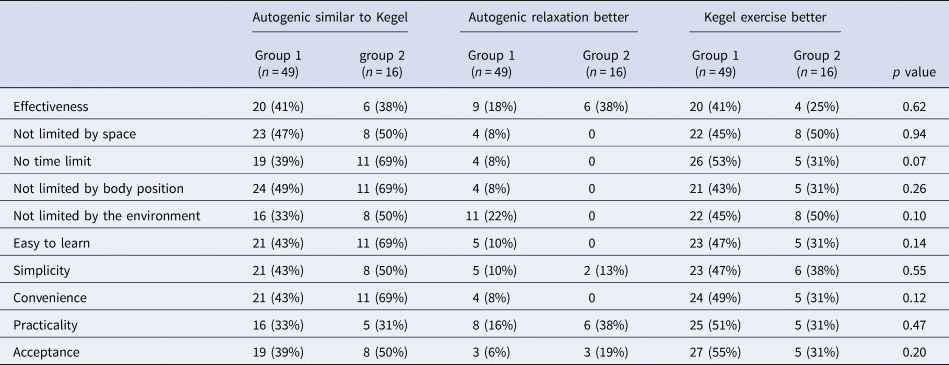
COVID-19, coronavirus disease 2019; SARS, severe acute respiratory syndrome.
Discussion
At present, there is a lack of solid guidelines for favoring relaxation in medical health workers while wearing medical protective equipment, although this might be a helpful strategy to reduce distress and burnout risk in medical health staff.
The present study showed that Kegel exercise was an effective, simple, practical method of self-relaxation by medical health workers when they are at work and wear medical protective equipment. The main reasons of such a preference were: (1) more participants thought Kegel exercise was better than autogenic relaxation from 10 assessment dimensions; (2) scores on 10 dimensions on Kegel exercise were higher than those on autogenic relaxation; (3) Kegel exercise is not limited by body position, including sitting, standing, or walking. (4) Kegel exercise is a traditional method of strengthening the body, involving traditional Chinese medicine (Tsai et al., Reference Tsai, Lai, Lee, Chen, Lan, Yang and Chiang1995). On the contrary, during leisure time, autogenic relaxation was firstly preferred. Additionally, listening to music and physical exercise were self-relaxation techniques followed by autogenic relaxation used by medical staff during leisure time. Our results indicate that autogenic relaxation, listening to music, and physical exercise do have a role in reducing stress and protect brain and body proposed by the previously reported studies on other populations (Cervellin & Lippi, Reference Cervellin and Lippi2011; Klainin-Yobas et al., Reference Klainin-Yobas, Oo, Suzanne Yew and Lau2015; Nabi et al., Reference Nabi, Kivimäki, Batty, Shipley, Britton, Brunner and Singh-Manoux2013; Pospos et al., Reference Pospos, Young, Downs, Iglewicz, Depp, Chen and Zisook2018; Seo et al., Reference Seo, Hong, Choi, Kim, Brandt and Im2018; Silva et al., Reference Silva, Tortelli, Motta, Menguer, Mariano, Tasca and Silveira2019; Yang & Chen, Reference Yang and Chen2018). To be noted, participants of the study often stayed in hotel rooms in Hubei during their leisure time due to COVID-19's airborne transmission via aerosol and droplets (Izzetti, Nisi, Gabriele, & Graziani, Reference Izzetti, Nisi, Gabriele and Graziani2020; Zhang, Li, et al., Reference Zhang, Li, Zhang, Wang and Molina2020). This might have influenced their preferences. Furthermore, a broader approach such as sleep hygiene, social support, and facilitation from employer or organizer might be needed to reduce their stress when medical health workers were in their leisure time (Theorell, Reference Theorell2020). Moreover, Ost's applied relaxation, although not our relaxation methods in the study, might be a strategy to rapidly relax in an increasingly stressful situation (Hayes-Skelton, Roemer, Orsillo, & Borkovec, Reference Hayes-Skelton, Roemer, Orsillo and Borkovec2013; Ost, Reference Ost1987; Reference Ost1988).
Until now, few previous studies have reported how medical staff relieves their distress at work and during leisure times (Aronsson et al., Reference Aronsson, Theorell, Grape, Hammarstrom, Hogstedt, Marteinsdottir and Hall2017; Pospos et al., Reference Pospos, Young, Downs, Iglewicz, Depp, Chen and Zisook2018). Work environment can induce medical staff burnout symptoms (Aronsson et al., Reference Aronsson, Theorell, Grape, Hammarstrom, Hogstedt, Marteinsdottir and Hall2017), and seven web-based instruments and mobile utilizations were devised to lessen burnout, negative emotion, and even suicide among healthcare students and professionals (Pospos et al., Reference Pospos, Young, Downs, Iglewicz, Depp, Chen and Zisook2018). However, no studies on relaxation techniques suitable for medical staff while wearing medical protective equipment are available.
This is the first study to explore the possible simple self-relaxation method when people were in a strictly limited working environment. Our study sample of step 2 was strictly limited to medical health workers who volunteered to support medical service in Wuhan during the epidemic. Therefore, they were a typical representative group in a special environment, such as being a contracted condition. The present study has, however, limitations. First, a cross-sectional design was used, a pre- and -post design with specific questionnaires on the assessment of anxiety and tension, which might provide additional and stronger information. Second, except for the recruited 65 participants, it is unknown how many subjects who visited or accepted these recommended relaxation techniques and the online survey on their evaluations about these techniques. Third, the dimensions were assessed via a self-rated analogue scale, a clinician-rating method might be helpful to collect data more objectively.
Conclusions and implications
Kegel exercise was preferred for first-line medical health workers at working, while autogenic relaxation was preferred during leisure time among the pandemic. There is apparently room for proposing simple, easy, and practical self-relaxation techniques to first-line medical health workers while they must wear medical protective equipment in order to reduce their level of stress.
Acknowledgements
The authors are grateful for participants’ priceless time and excellent cooperation and their online informed consent.
Financial support
This work was supported by the National Key Research and Development Program of China (2017|YFC1310001, 2016YFC1307000), the National Natural Science Foundation of China (81771862), Beijing Science and Technology Project (Z171100000117016), and Beijing Hundred, Thousand, and Ten Thousand Talents Project (2017-CXYF-09).
Conflict of interest
None.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.







