Introduction
The importance of advance care planning (ACP) has been gaining more and more attention. ACP can improve patient–clinician communication quality, improve the quality of end-of-life (EOL) care (e.g. reducing unwanted hospital admissions, increasing the use of palliative care), and increase patients’ satisfaction and quality of life (Brinkman-Stoppelenburg et al. Reference Brinkman-Stoppelenburg, Rietjens and van der Heide2014; Rietjens et al. Reference Rietjens, Sudore and Connolly2017; Schrijvers and Cherny Reference Schrijvers and Cherny2014; Wright et al. Reference Wright, Zhang and Ray2008). Although ACP can be performed under various physical conditions and at any stage of treatment, it becomes more important toward the EOL (Rietjens et al. Reference Rietjens, Sudore and Connolly2017).
Discussing EOL issues with patients, such as prognosis, code status, and hospice referral, remains challenging for clinicians, and tends to occur later in the disease progression (Levin et al. Reference Levin, Li and Weiner2008; Mack et al. Reference Mack, Cronin and Taback2012; Mori et al. Reference Mori, Shimizu and Ogawa2015). Both physician and patient factors are contributed to barriers to EOL discussions (Bernacki and Block Reference Bernacki and Block2014; Mori et al. Reference Mori, Fujimori and van Vliet2019b, Reference Mori, Shimizu and Ogawa2015; van Vliet et al. Reference van Vliet, van der Wall and Plum2013). Physicians’ factors include discomfort in discussing delicate issues, and fear of causing patient distress (Bernacki and Block Reference Bernacki and Block2014; Mori et al. Reference Mori, Shimizu and Ogawa2015; You et al. Reference You, Downar and Fowler2015). As for the patient side, it is considered that there are potentially varying preferences with different coping styles (Mori et al. Reference Mori, Fujimori and Ishiki2019a, b; van Vliet et al. Reference van Vliet, van der Wall and Plum2013). Patients’ preferences vary when discussing prognosis including explicit disclosure such as median survival, typical range (Clayton et al. Reference Clayton, Butow and Arnold2005; Mori et al. Reference Mori, Fujimori and van Vliet2019b; van Vliet et al. Reference van Vliet, van der Wall and Plum2013), best/worst cases (Kiely et al. Reference Kiely, McCaughan and Christodoulou2013; Mori et al. Reference Mori, Fujimori and Ishiki2019a), or probability of living for a certain period (Hui Reference Hui2015; Umezawa et al. Reference Umezawa, Fujimori and Matsushima2015), and nonexplicit disclosure such as the possibility of living until a certain event (Clayton et al. Reference Clayton, Butow and Arnold2005) and unit of time frames (Clayton et al. Reference Clayton, Butow and Arnold2005; Umezawa et al. Reference Umezawa, Fujimori and Matsushima2015).
In this study, the EOL disclosure is defined as the notice of prognosis and prospects to patients and/or their families to start the EOL discussion. The way of disclosure is influenced by culture (Mori et al. Reference Mori, Shimizu and Ogawa2015; Schrijvers and Cherny Reference Schrijvers and Cherny2014). In daily life, Japanese people often use vague or roundabout expressions in conversation. In addition to that, according to a nationwide research on the concept of “a good death,” the majority of the general population in Japan considered “dying without the awareness that one is dying” as an important factor to achieve what they considered to be a good death (Miyashita et al. Reference Miyashita, Sanjo and Morita2007). Also, approximately half of the subjects took into consideration that “not being informed of bad news” was a critical issue during the final days of life. Considering these results, some physicians may use vague phrases to reduce the burden on the patient in the EOL disclosure.
Moreover, there have been few studies that investigated the actual expressions of EOL disclosure in clinical practice. In the current study, we have aimed to clarify the specific expressions of EOL disclosure. We especially focused on how and when euphemistic expressions are used. Further, we investigated whether the use of euphemisms in EOL disclosure has any association with the participation of the patients in the EOL discussions and the timing of such discussions. We hypothesized that using euphemistic expressions, which potentially reduce the burden of bringing up the topic of EOL for physicians, facilitates EOL discussions from an earlier stage of illness and promotes patient participation in the discussion.
Methods
This retrospective chart review study was conducted at Keio University Hospital, a university-affiliated teaching hospital (tertiary medical facility) in Central Tokyo, Japan. The details of the methods were reported elsewhere (Abe et al. Reference Abe, Kobayashi and Kohno2021). In short, the eligible patients were all those who were hospitalized and died at the study site during the period from April 2018 to March 2019. The following patients were excluded: (1) cardiopulmonary arrest on arrival (CPAOA); (2) stillbirth; (3) under 18 years old at the time of death; and (4) refusal by their bereaved family.
The presence or absence of the discussion where a clinician disclosed that the patient is at his/her EOL stage (EOL disclosure) and cardiopulmonary resuscitation (CPR)/do-not-attempt-resuscitation (DNAR) discussion was investigated. The EOL disclosure was defined as a discussion where a treating clinician informed that the patient’s death was approaching (usually within weeks or months) and aggressive life-prolonging treatment was not considered useful. In the case where EOL disclosure was made, the specific expression used in the disclosure was investigated, along with the date of the disclosure, and whether the patient himself/herself participated in the discussion.
To categorize the expressions of EOL disclosure, 2 physicians (AA and TM) first reviewed and discussed specific expressions of EOL disclosure for 30 patients. After the categories were defined, the 2 physicians classified all other cases independently into those categories. When the results were not concordant, a discussion was held until an agreement was reached.
Statistical analysis
The characteristics of the patients were compared between each explanatory pattern. Categorical and continuous variables were compared using the Chi-square test and nonparametric tests, respectively. A p-value <0.05 was considered statistically significant. All analyses were conducted using the IBM SPSS versions 24.0 and 25.0 (IBM Corp., Armonk, NY, USA).
Results
The participants’ characteristics
During the study period, 377 patients died in the hospital. Of them, 19 were excluded (CPAOA: n = 12, stillbirth: n = 2, and under 18 years old: n = 5). Of the remaining 358 patients, 17 did not have an opportunity for EOL disclosure and were excluded, resulting in 341 patients subjected to analyses (Figure 1).
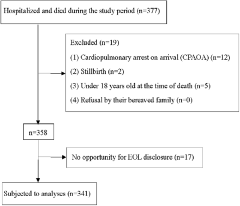
Figure 1. Flow diagram.
The patients’ characteristics are shown in Table 1. Two-thirds of the deceased patients were male, and the patients’ mean age was 70 years. Approximately 60% of the patients died of cancer. The percentage of patients who participated in the initial EOL disclosure themselves was 40.2%.
Table 1. Demographic and clinical characteristics of the patients (n = 341)
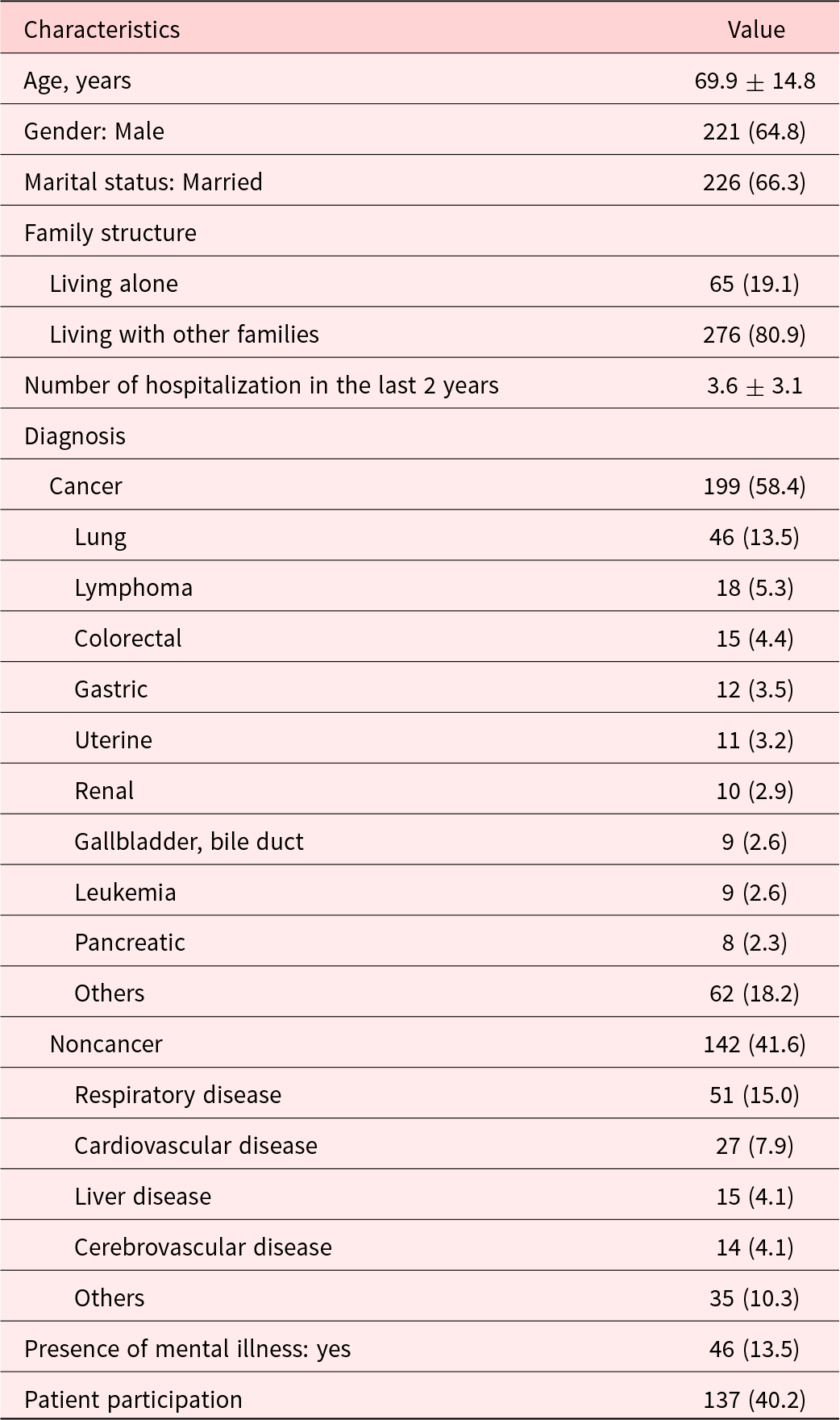
Data are represented as mean ± SD or n (%). SD = standard deviation.
Explanatory patterns of the EOL disclosure
Four explanatory patterns for expressions of EOL disclosure were identified. Examples of expressions used in the initial EOL disclosure are shown in Table 2.
Table 2. Specific examples of expressions used in the initial EOL disclosure
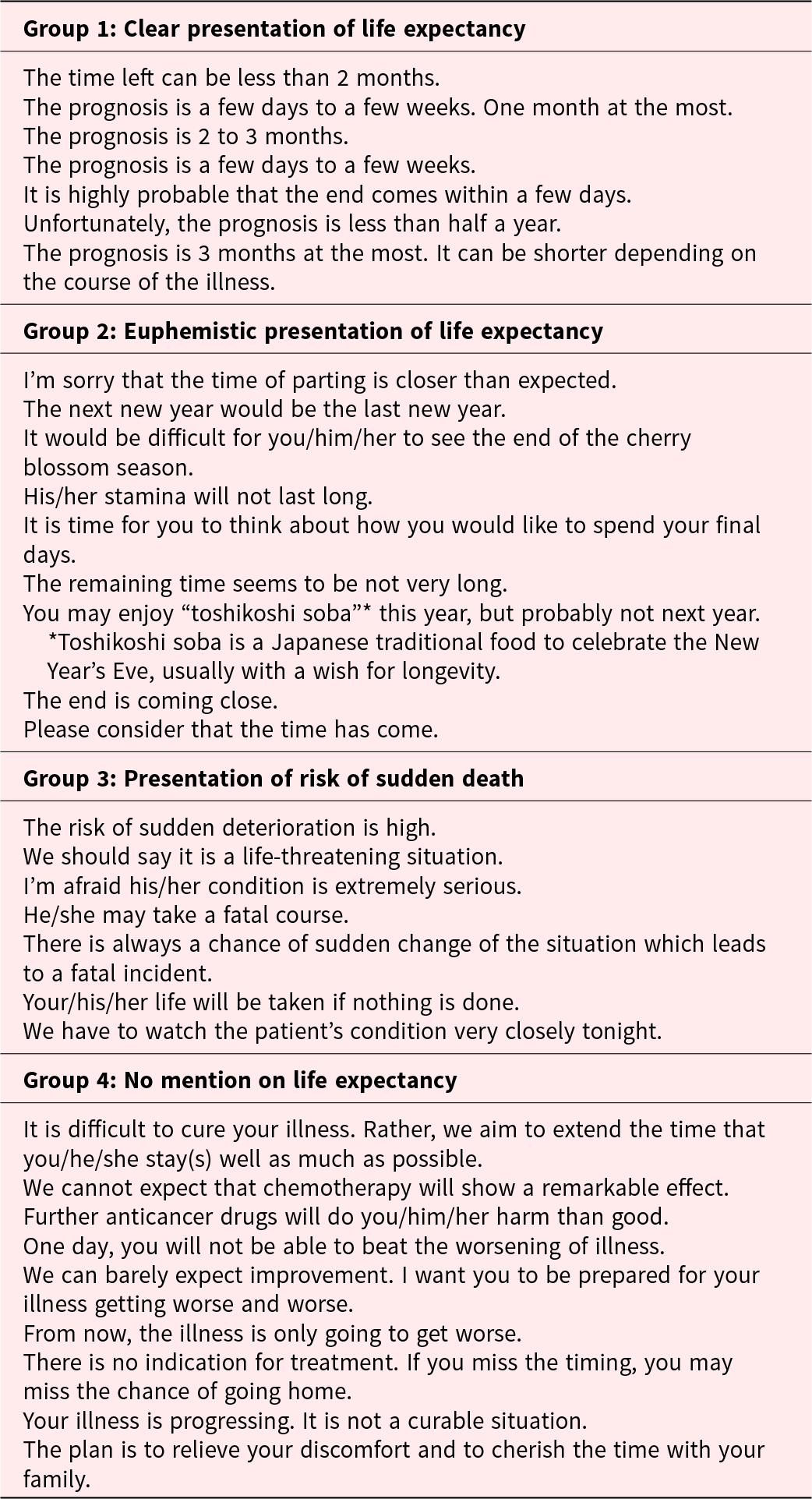
Group 1: Clear presentation of life expectancy (n = 106; 31.1%)
Patients’ life expectancy was expressed in concrete numbers or concrete units of time.
Group 2: Euphemistic presentation of life expectancy (n = 24; 7.0%)
Patients’ life expectancy was expressed implicitly.
Group 3: Presentation of risk of sudden death (n = 147; 43.1%)
A physician told the patient or his/her family that the patient was in a serious situation and is at risk of sudden death, but did not refer to life expectancy.
Group 4: No mention on life expectancy (n = 64; 18.8%)
A physician told the patient or his/her family that the patient’s illness was serious and told there was no curative treatment for the disease. The physician may recommend the best supportive care.
Participants’ characteristics of each group
The characteristics of each group are shown in Table 3. The patients in Groups 1 and 2, who were informed of their life expectancy, were more likely to be male, while those in Groups 3 and 4, who were not informed of their life expectancy, were more likely to be female. The proportion of male patients in Group 2 was particularly high. The patient participation rate was 30.2% for Group 1, 50.0% for Group 2, 26.5% for Group 3, and 84.6% for Group 4, respectively. The participation rate was highest in Group 4, which was followed by Group 2. The patient participation rates by gender in each group were as follows: Group 1: male 35.6%, female 18.2%, p = 0.070, Group 2: male 52.6%, female 40.0%, p = 0.50, Group 3: male 29.0%, female 22.2%, p = 0.37, Group 4: male 83.3%, female 85.7%, p = 0.54. Only Group 1 tended to have higher participation rate for men. Group 4 had the longest period from the diagnosis to the death with a median of 880 days, and Group 3 had the shortest with 208 days. The rate that the EOL disclosure and the DNAR discussion took place on the same day was highest in Group 3 (62%), while the rates were only approximately 30% in other groups (Groups 1, 2, and 4). The majority of the cancer patients fell into Groups 1 and 4, while Group 3 alone accounted for 70% of the noncancer patients.
Table 3. The characteristics of each group
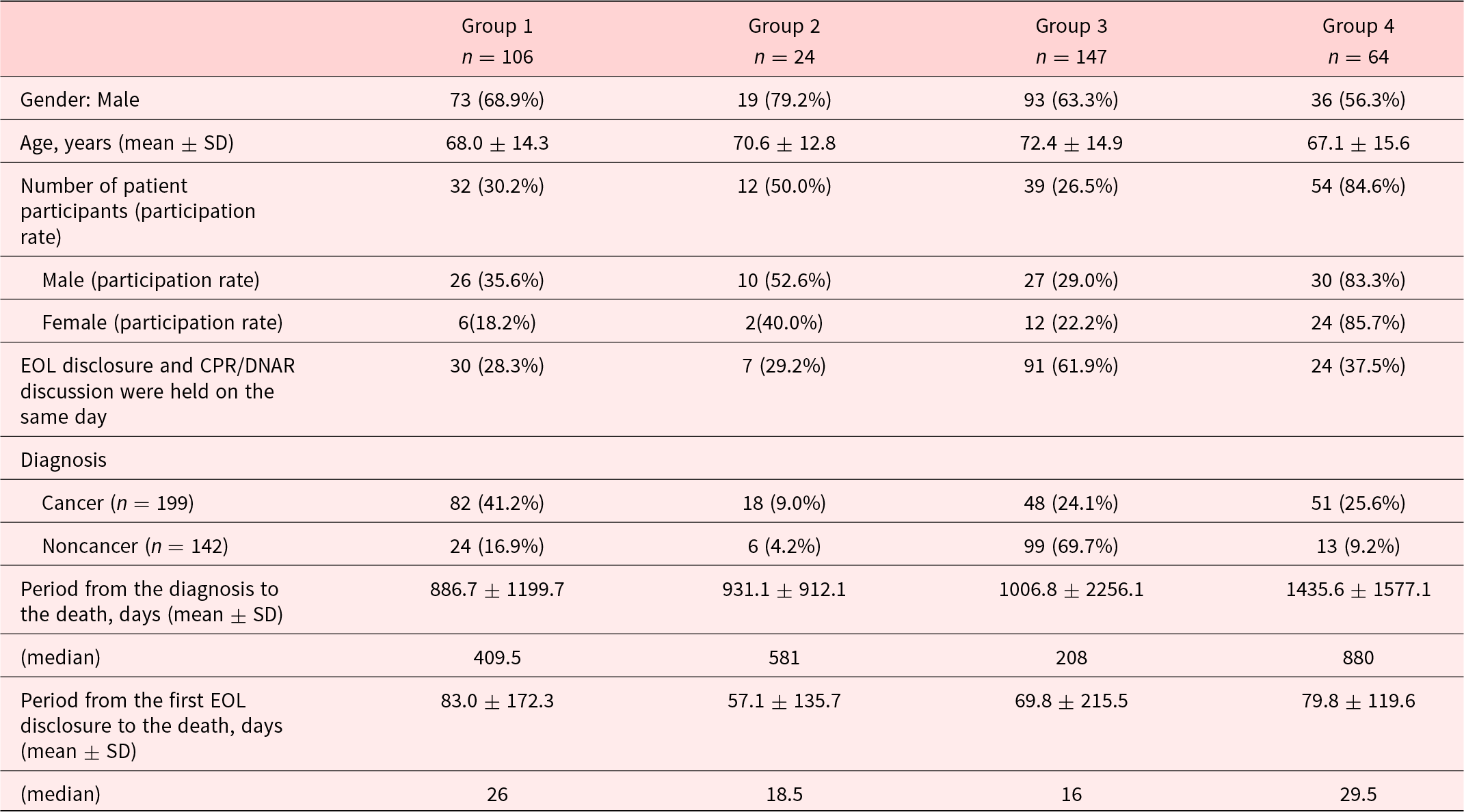
SD = standard deviation, CPR = cardiopulmonary resuscitation, DNAR = do-not-attempt resuscitation.
Association of explanatory patterns and duration from EOL disclosure to death and patient participation
Figure 2 shows the distribution of the 4 explanatory patterns over the length of time from EOL disclosure to death and the patient participation rate, divided by cancer and noncancer.
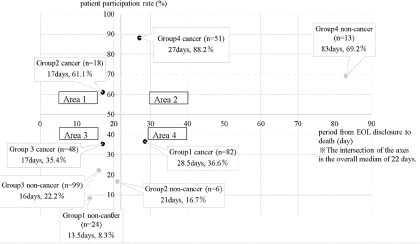
Figure 2. Period from EOL disclosure to death and patient participation rate.
Cancer cases
Cancer cases showed a higher patient participation rate, both overall and for each group than noncancer cases. Specifically, Group 4 showed the highest participation rate (88%) followed by Group 2 (61%). The patient participation rate was lower in Groups 1 and 3 (approximately 35% in both groups). The median times from EOL disclosure to death were approximately 1 month for Groups 1 and 4, while they were as short as 17 days for Groups 2 and 3.
Noncancer cases
In noncancer cases in general, the rate of patient participation was lower, and the period from EOL disclosure to death was shorter than in cancer cases. The only exception was Group 4, whose period from EOL notification to death was significantly longer, and the patient participation rate was higher, at about 70%.
Discussion
In this study, we investigated the expressions used in EOL disclosure and examined the factors associated with the characteristics of such expressions. Four distinct groups of EOL disclosure were identified. The highest patient participation rate was in the group with “no mention of life expectancy.” We hypothesized that Group 2, where euphemistic expressions of life prognosis were used, would present a longer time between the EOL disclosure and death as compared to Group 1, where direct expressions of life prognosis were used, however, this was not the case. The situations where euphemistic expressions on life prognosis were used were likely to be the situations where the patient’s death was quite imminent. The use of euphemistic expressions seems to be a reflection of the physicians’ reluctance of presenting life prognosis explicitly with the fear of causing distress to their patients.
Characteristics of the expressions in 4 groups
As shown in Table 2, the ways to express EOL disclosure were classified into 4 categories – 2 of which were the cases that the period of life expectancy mentioned, and another 2 of which were otherwise. The former categories comprised clear presentation (Group 1) and euphemistic presentation (Group 2). There were 2 categories in the groups where life expectancy was not mentioned: one that mentioned the high risk of sudden change (Group 3) and the other that emphasized incurability of the illness and that does not refer to life expectancy (Group 4).
Group 1 corresponds to the cases where the patient’s life expectancy was indicated using concrete units of time. This group accounted for about 30% of the total discussions. The time units mentioned by the physician in the discussions ranged from a few days to a few months. Typical expressions that were used to describe “prognosis” were “the time left,” “the end,” and “the time of parting.”
Group 2 corresponds to the cases where the patient’s life expectancy was indicated with euphemistic expressions. Typical examples were euphemisms that focus on special times of the year. Expressions that are related to Japanese traditions were frequently used – for example, the New Year, ‘Toshikoshisoba’ (a traditional noodle dish eaten on New Year’s Eve in Japan), and cherry blossom season. There was no mention of the birthdays or anniversaries of the patients in our study, in contrast with a previous Australian study (13). In some cases, euphemistic expressions imply prognosis (e.g. by referring to cherry blossoms, the treating physician implies that the patient’s life expectancy is a few months). However, in the cases where expressions like “the remaining time is not long” and “the last moment is approaching” were used, the patients and/or their family might imagine an amount of time that was different from the health professionals’ intentions.
In Group 3, health professionals indicate that the patient’s condition is very serious and there is a high risk of sudden change. In this group, the expressions such as “The risk of sudden deterioration is high,” “We should say it is a life-threatening situation,” and “He/she may take a fatal course” were used. In Japan, it has been customary for health professionals to use an expression of “We have to watch the patient’s condition very closely tonight” to convey that there is a high risk of sudden changes in the patient’s condition. Physicians are trying to use these expressions to show there is possibility of imminent death.
In Group 4, health professionals indicate that there was no curative treatment for the disease and that there was no hope of improvement. In cancer cases, the remarks include a discussion of the discontinuation of aggressive cancer treatment such as anticancer drugs and sometimes focus on palliative care.
Associated factors of each group
As suggested in Table 3 and Fig. 2, there are some characteristics and related factors for each group.
Gender
The patients in Groups 1 and 2, who were informed of their life expectancy, were more likely to be male, while those in Groups 3 and 4, who were not informed of their life expectancy, were more likely to be female. The proportion of male patients in Group 2 was particularly high. Group 1, where specific life expectancy was discussed, had a large gender gap in patient participation rates, with male patients being twice as likely to participate. Male participants, either as a patient himself or as the husband or partner of female patients, seem to hope to be notified of concrete life expectancy. We speculate that there may be paternalistic perspectives in Japan where autonomy is emphasized more among men than women, while women need to be “protected” from serious medical information. It should be carefully addressed whether health professionals’ proneness of communication coincides with patients’ preferences, considering the individuality of each patient. Some previous studies suggested that there are gender differences in the preference for how to receive bad news. Previous Japanese studies indicated that female patients placed more importance on delivering bad news clearly in a manner that facilitates each patient’s full understanding, and explicit prognostic disclosure (Fujimori et al. Reference Fujimori, Akechi and Uchitomi2017; Mori et al. Reference Mori, Fujimori and van Vliet2019b), while male patients are more likely to adopt a passive role in their communication with physicians (Fujimori et al. Reference Fujimori, Akechi and Uchitomi2017). Also, a German study showed that male patients wish to avoid engagement in discussions about death and dying particularly if they are anxious about their EOL period (Seifart et al. Reference Seifart, Riera Knorrenschild and Hofmann2020).
Patient’s participation rate and period from the diagnosis to the death
Patient participation rates were higher in Groups 2 and 4 than in Groups 1 and 3. Regarding the duration of illness, Group 4 was notably longer and Group 3 was the shortest. There was a tendency to avoid presenting life expectancy clearly (Group 4) and to use euphemisms (Group 2) when the patients themselves participated in the discussion. The highest participation rate (84.4%) was seen in Group 4 (“no mention of life expectancy”). Considering that the period from diagnosis to death of Group 4 is significantly longer than in other groups, we speculate that this may be a product of a tighter bond formed between treating physicians and patients, which results from the long process of fighting the illness together. We did not examine the bond between physicians and patients in this study, so this should be verified in future research.
On the other hand, Group3 (“presentation of risk of sudden physical change”) had the lowest patient participation rate and the shortest time from diagnosis to death. Two possible explanations are considered: first, the physical conditions of the patients in this group were so critical that the patients were physically unable to have conversation with their physicians (e.g. due to confusion, loss of consciousness, etc.). Second, physicians avoided direct expressions since the physical conditions of the patients were so serious that they intended not to discourage or frighten their patients by telling the truth.
Relationship between EOL disclosure and CPR/DNAR discussion
The percentage of which the EOL disclosure and CPR/DNAR discussion were held on the same day was highest in Group 3. This may be due to the fact that the EOL disclosure and CPR/DNAR discussion are often held on the same day when the patient’s situation is critical, such as in the case of Group 3. In contrast, EOL disclosure and CPR/DNAR discussion are usually held on different days in other groups. In other words, participating in the EOL disclosure does not equate to participating in the CPR/DNAR discussion. Discussions on CPR/DNAR are considered invasive to the patients and are not open to the topic at once; therefore, discussions on prognosis and CPR/DNAR take place at different stages of illness.
Relationship with a type of disease (cancer/noncancer)
The majority of the cancer patients fell into Groups 1 and 4, while Group 3 alone accounted for 70% of the noncancer patients. Generally, the course of cancer is more predictable than the course of noncancer diseases (Murray et al. Reference Murray, Kendall and Mitchell2017); therefore, it is easier for health professionals to estimate and convey the life expectancy in concrete terms (Group 1) as well as to discuss the strategy of treatment, such as discontinuation of anticancer drugs (Group 4) in cancer settings.
One of the possible reasons that noncancer patients are often classified as Group 3 may be that noncancer diseases include acute-onset diseases such as myocardial infarction and cerebrovascular disease, which are prone to sudden death. On the other hand, some noncancer diseases gradually progress with repeated exacerbations and remissions. Some of these diseases could have been classified as Group 3 by presenting an acute risk of sudden change during acute exacerbations. The possible scenarios in Group 4 cases are that the patients were informed that their illness entered the final refractory stage, but their life expectancy is still long.
Significance of euphemisms
According to the results observed, there are 2 main elements that arise in the use of euphemisms for EOL disclosure. First, regarding the timing of the first discussion, the median times from EOL disclosure to death were approximately 1 month for Groups 1 and 4, while it was as short as 18.5 days in Group 2 and 16 days in Group 3. Contrary to our hypothesis that using euphemistic expressions makes it easier for health professionals to conduct EOL discussions from an early stage, the timing of the EOL disclosure was quite late in the cases where euphemisms were used. The length of time from EOL disclosure to death was almost the same both in the cases using the euphemistic expressions of life expectancy and the cases mentioning the high risk of sudden change. In other words, physicians seem to have just rephrased “The risk of sudden change is high” to expressions such as “You can’t celebrate the New Year,” “You can’t see the next cherry blossoms,” and “You don’t have much time left.” Both expressions only inform the patients that their death is approaching and intend to indirectly make patients and their families aware of their situations.
The second element was regarding the patient participation rate. When the patient is present at the EOL discussion, the physicians tend to avoid direct expressions of life expectancy (Group 1; patient participation rate 30.2%) and the possibility of imminent death (Group3; 26.5%). When comparing Groups 1 and 2, in which the physician mentions their life expectancy, the patient participation rate in Group 2 (50.0%) was slightly higher than that in Group 1 (30.2%). This shows that the use of euphemisms did not have a significant effect on patient participation, in light of the highest participation rate being at 84% in this study. Rather, this reflected the physicians’ reluctance to use direct expressions of the patients’ life prognosis with a fear of causing distress to the patient.
Euphemistic expressions appear to be “gentle and kind” to the patients; however, they can be misleading and sometimes can result in situations where the patient or their family do not fully comprehend the seriousness of the situation. Previous studies show that there is a difference in prognosis perception and optimism between physicians and patients (Christakis and Lamont Reference Christakis and Lamont2000; Glare et al. Reference Glare, Virik and Jones2003; Hiratsuka et al. Reference Hiratsuka, Oishi and Miyashita2023; Maltoni et al. Reference Maltoni, Caraceni and Brunelli2005); even if physicians intend to “tell the fact accurately,” sufficient understanding may not be obtained between the physicians and the patients. For example, in a study targeted at heart failure patients, there was a substantial discrepancy between the amount and quality of information about the patient’s prognosis and the actual information provided by their treating physicians (Kitakata et al. Reference Kitakata, Kohno and Kohsaka2021). Further, a few studies have shown that explicit prognostic disclosure promoted better outcomes than nondisclosure (Mori et al. Reference Mori, Fujimori and van Vliet2019b; van Vliet et al. Reference van Vliet, van der Wall and Plum2013), and non-explicit disclosure using specific events such as “cherry blossoms” and “anniversaries” are not preferred by the patient (Mori et al. Reference Mori, Fujimori and Ishiki2019a). No matter how “creative” the health professionals are when informing their life expectancy to their patients, euphemisms may not be an effective communication tool. There is room for further investigation as to whether a doctor’s “compassion” leads to a higher quality of life, especially at the EOL.
Limitation
The current study has a few limitations. First, this is a single-center study of an urban university hospital. The study site was an acute-care hospital without a palliative care unit; therefore, the patients who were transferred to another hospital or a home-based hospice program at their EOL were not included.
Second, since this was a retrospective chart review study, communication between health professionals and the patients which were not documented in the medical record was not captured.
Third, there is no information on the doctors who deliver the notification in this survey. The way of disclosure and the expressions used in EOL discussion may be influenced by communication style and skills of treating physicians. Further, the doctor’s view of prognosis prediction may have affected their communication.
Finally, the current study did not assess patient preferences. In a previous Japanese study, the minority of patients strongly preferred to know their prognosis (Hamano et al. Reference Hamano, Hiratsuka and Morita2022).
Future research implications include exploring the relationship between the length of illness and the strength of the bond between the attending physician and the patient. Further, the relationship and strength of the connection between physicians and patients, preferences regarding the expressions of disclosure and communication style for both the physicians and the patients and patient satisfaction with these disclosures, should be examined.
Conclusions
Four patterns of expressions of life expectancy in the EOL disclosure were observed. In euphemistic expressions, some culturally unique expressions were observed. Patterns of communication are influenced by patients’ gender and type of illness (cancer or noncancer). As opposed to the authors’ hypothesis, euphemistic expressions do not seem to facilitate accurate and timely disclosure of life expectancy. Further, they do not facilitate the patient participation in a discussion. Although it is undoubtedly essential for health professionals to devise expressions to alleviate their patients’ distress when breaking bad news, the communication process and patient background must be considered when starting EOL discussions.
Acknowledgments
The authors thank Naho Ihara (Department of Anesthesiology, Keio University School of Medicine), Yoko Takino (Palliative Care Center, Keio University School of Medicine), Miwako Ohgishi (Palliative Care Center, Keio University School of Medicine), Sachiko Fujita (Department of Nursing, Keio University Hospital), and Ken Kaneko (Palliative Care Center, Keio University Hospital) for their support.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
The authors declare no conflict of interest.
Ethical approval
The study complied with the Declaration of Helsinki and was approved by the ethics committee of Keio University Hospital (Approval number: 20190034). Permission to collect and analyze data was given by the bereaved family by opt-outs.








