In order to reduce the risk of CVD, the UK Scientific Advisory Committee on Nutrition (SACN) recommends a population reduction of dietary saturated fat (SFA) intake to an average of < 11 % of food energy and a minimum daily intake of 0·45 g of the long-chain n-3 PUFA (LC n-3 PUFA), EPA and DHA(1). There is a rapidly increasing body of evidence on the significant impact of genetic variation and other physiological and lifestyle factors on an individual's response to dietary manipulation, and a recognition of the large inter-individual heterogeneity in response to dietary change. In light of this, it is predicted that a more personalised/stratified approach to nutritional advice may be more effective in the reduction of disease risk(Reference Lovegrove and Gitau2) relative to the more generic advice currently provided. Available evidence examining genotype–diet–phenotype associations is largely derived from epidemiological studies, with data from ‘fit-for-purpose’ randomised controlled trials distinctly lacking.
ApoE is a structural component of TAG-rich lipoproteins required for lipid transport and clearance. There are a number of SNP of the gene encoding for this apolipoprotein. The most studied are the APOE epsilon missense mutations rs429358 and rs7412 that give rise to three common isoforms (Apoɛ2, Apoɛ3 and Apoɛ4). These isoforms are coded by three separate alleles, E2, E3 and E4, with the resulting proteins differing at amino acid positions 112 and 158, with apoE2 having cysteine at both positions, apoE3 having a cysteine at position 112 and arginine at position 158 and apoE4 having arginine at both positions. ApoE4 carriers, estimated at a frequency of about 30 % in the UK population(Reference Song, Stampfer and Liu3), have been reported to have higher plasma total cholesterol, LDL-cholesterol (LDL-C) and TAG concentrations(Reference Ordovas and Mooser4). A meta-analysis has estimated a 40–50 % higher CVD risk in E4 carriers relative to the E3/E3 wild-type genotype(Reference Song, Stampfer and Liu3). Furthermore, there is some evidence to suggest that E4 carriers may be more responsive to dietary fat manipulation, with elevated LDL-C concentrations with a high SFA intake and greater LDL-C reductions following the switch to a low-fat diet in this subgroup relative to non-apoE4 carriers(Reference Sarkkinen, Korhonen and Erkkila5). In addition, high-dose DHA supplementation (>2 g/d) has been reported to have a LDL-C-raising effect in E4 carriers only(Reference Olano-Martin, Anil and Caslake6). However, to date, the majority of trials have been conducted in small groups in whom genotyping was carried out retrospectively. This has often resulted in insufficient statistical power to draw definitive conclusions. Also, although SFA and LC n-3 PUFA intakes represent key nutritional targets for CVD risk reduction, the combined impact of SFA and DHA on the CVD risk phenotype, and in particular according to the APOE genotype, is unknown. Therefore, there is a recognised need for suitably powered, prospectively genotyped human dietary intervention studies in this area, which will inform future population and personalised/stratified dietary fat composition recommendations.
The aim of the SATgenɛ (SATurated fat and gene APOE) study was to investigate the effects of three isoenergetic diets differing in fat quantity and quality on fasting and postprandial lipid concentrations and other CVD risk markers in free-living individuals. A dietary exchange strategy was developed to allow manipulation of fat quantity and profile without changing other components of the diet. This facilitated the implementation of specific fat manipulation without confounding effects of other dietary changes. Dietary strategies developed within our group have been published previously using specially formulated products to achieve specific dietary fatty acid compositions(Reference Shaw, Tierney and McCarthy7, Reference Moore, Gitau and Goff8). These strategies have been adapted for the SATgenɛ study in which only commercially available products were used as intervention foods. The present study describes and evaluates the use of the SATgenɛ dietary exchange strategy to implement a low-fat (LF), high-SFA (HSF) diet and a high-SFA diet with 3 g DHA/d supplementation (HSF-DHA) in free-living participants over a 24-week period.
Experimental methods
Participants and study design
Over 250 individuals were screened for the study, of which 100 free-living participants were selected to take part after meeting specific inclusion criteria. Subjects were aged 35–70 years; BMI 20–32 kg/m2; blood pressure < 100/160 mmHg; generally fit and healthy and taking no antihypertensives, 3-hydroxyl-3-methylglutaryl-CoA reductase inhibitors or antithrombotic agents; had not suffered a stroke or myocardial infarction in the previous 12 months; were not pregnant or breast-feeding; did not have to follow a special diet, did not consume excessive amounts of alcohol (more than 21 units per week for men and 14 units per week for women) and were not taking fish oil supplements. A screening blood sample was collected to ensure that fasting TAG was between 1 and 4 mmol/l, total cholesterol 4·5–8 mmol/l, glucose < 7 mmol/l, γ-glutamyltransferase < 80 U/l and Hb 125–180 g/l in men and 115–160 g/l in women. Equal numbers of E4 carriers (i.e. E3/E4 or E4/E4) and the wild-type E3/E3 genotype were recruited, with the two genotypic subgroups matched for age and BMI.
The study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the University of Reading Research Ethics Committee. Written informed consent was obtained from all subjects. SATgenɛ is a registered clinical trial (Clinicaltrials.gov ID NCT01384032).
A sequential study design, employed in previous dietary studies such as Dietary Approaches to Stop Hypertension(Reference Sarkkinen, Korhonen and Erkkila5, Reference Svetkey, Sacks and Obarzanek9) and a study investigating the effect of the APOE genotype on serum lipid response to the dietary fat and cholesterol modification(Reference Sarkkinen, Korhonen and Erkkila5), was used due to inherent difficulties during fat manipulation studies for volunteers to return to their habitual diet during washout periods if a cross-over design is used. All participants followed three prescribed diets each for 8 weeks in the same order. Participants completed a 1-week run-in period during which they were instructed to consume their habitual diet plus 2 g of control capsules per d containing palm olein and soyabean oil in the ratio 4:1, providing a fatty acid profile of the typical UK diet (44 % SFA, 39 % MUFA and 17 % n-6 PUFA). These capsules were also consumed during the subsequent LF and HSF 8-week dietary periods. The first diet was a LF diet (target composition: 24 % of energy (%E) from fat, 8 %E from SFA, 8 %E from monounsaturated fat (MUFA), 6 %E from polyunsaturated fat (PUFA) and 59 %E from carbohydrate (CHO)); the second was the HSF diet (target composition: 38 %E from fat, 18 %E from SFA, 12 %E from MUFA, 6 %E from PUFA and 45 %E from CHO) and the third was identical to the HSF diet in composition but with the addition of 6 g DHA-enriched fish oil capsules (DHA-rich oil comprised 5·7 % SFA, 11·6 % MUFA, 82 % PUFA, 8·3 % EPA, 3·1 % docosapentaenoic acid and 57·5 % DHA), which provided 3 g DHA/d. All diets were designed to be isoenergetic with identical protein intakes.
Fasting blood samples, blood pressure, anthropometrics and a measure of arterial stiffness (Digital Volume Pulse; Micro Medical Limited) were taken during four clinical visits, one at baseline and one at the end of each 8-week dietary periods for the determination of biomarkers of CVD. Total cholesterol and LDL-C represented the primary outcome measures. The results of all clinical measures will be published separately.
Food exchange model to achieve dietary targets
A food exchange model based on the National Diet and Nutrition Survey of UK adults aged 19–64 years(Reference Henderson, Gregory and Irving10) was developed from a method used in previously published strategies from our group(Reference Shaw, Tierney and McCarthy7, Reference Moore, Gitau and Goff8). This served to establish that the composition of the three different diets was achievable within a free-living UK population using commercially available products (Table 1). The basic concept was that certain fat-containing foods could be removed from the diet and replaced by specifically chosen products in order to manipulate the overall fatty acid composition. The amount of exchangeable fat in the UK diet was calculated as the sum of the non-intrinsic fat present in the form of milk, cheese, spreads, oils, biscuits, cakes, pastries, buns and savoury snacks (Table 2). Intrinsic fat derived from other foods (such as meat products) was not included in the model, as this would be more difficult to manipulate and would result in unwanted confounding dietary changes. A change in CHO intake was also required in order to allow the three diets to remain isoenergetic despite the change in fat content. Commercially available high-fat and very-low-fat snacks were tested in the model in order to assess their efficacy in aiding the achievement of dietary targets before the final selections were made. The composition of all study foods is shown in Table S1 of the supplementary material (available online at http://www.journals.cambridge.org/bjn).
Table 1 Sources of exchangeable fat in the UK diet*
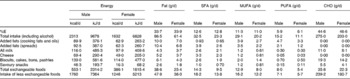
CHO, carbohydrate; %E, percentage of energy.
* Data sourced from the National Diet and Nutrition Survey(10).
Table 2 Replacement of exchangeable fat with the study foods

CHO, carbohydrate; LF, low fat; %E, percentage of energy; HSF, high saturated fat; HSF-DHA, high saturated fat plus DHA.
During the LF diet, participants were asked to consume the very-low-fat spread and spray cooking oil provided in place of all normally eaten spreads and oils. They were also asked to use low-fat dairy products and to consume two extra portions of CHO per d (e.g. two slices of bread, equivalent to 30 g CHO). Participants were allowed to consume a maximum of two of the LF snacks provided per d (e.g. flavoured rice cakes, cereal bars, pretzels) but were asked to avoid all high-fat snacks such as chocolate, crisps, biscuits, ice cream and cakes. Dietary advice was tailored to each individual based on their habitual diet and guidelines were flexible to accommodate food preferences. During the HSF diets, participants were asked to use the butter provided for spreading, cooking and baking, and to avoid all other spreads and oils. They were also instructed to consume one less portion of CHO per d (e.g. one slice of bread, equivalent to 15 g CHO) and to consume two of the HSF snacks provided in place of other normally consumed snacks (e.g. chocolate bars, biscuits, crisps). A wide range of sweet and savoury snacks were offered on both the LF and HSF diets in order to cater for the individual tastes and lifestyles of the participants. Spreads and oils were provided in quantities ample for the participants' entire household in order to aid compliance.
Dietary advice, food collection and compliance monitoring
Participants were advised to keep all remaining aspects of their diet unchanged, such as meat, fruit and vegetables and to try to maintain their weight throughout the study. Detailed dietary advice sheets indicating target intakes of study foods, items to choose and to avoid, advice for eating out and low-fat baking recipes were given to the participants and explained in detail by a researcher during clinical visits. The participants were supported in their dietary adherence by regular monitoring by the study investigators and were encouraged to contact the trained nutritionist if they required help and advice.
Participants attended the unit in order to collect their foods every 4 weeks. During this visit, compliance to the diets was encouraged and any problems with the diets were discussed and resolved. In addition, the participant's weight was recorded and in the event of any changes above ± 1 kg, subjects were advised to alter their snack or CHO intake accordingly. Capsules were returned at the end of each dietary period and counted to assess compliance.
Assessment of dietary intake
Participants completed four 3 d weighed diet diaries over two weekdays and one weekend day. The first was the habitual diet diary completed before undertaking the LF diet and one during weeks 4–5 of each of the three dietary periods. Participants were provided with scales, detailed instruction sheets and example diaries. Recipes used in cooking and packaging from processed foods were collected by the participants and added to the dietary database. Diet diaries were analysed using the software Dietplan 6.60 (Forestfield Software). For a small number of the low-fat study foods, full fatty acid profiles were not available on Dietplan because these products have only recently become available in the supermarkets. The composition of study foods was added to the database. In these cases, information derived from both food labels and personal communication with the food manufacturers was used to update the dietary analysis program. Where full fatty acid profiles could not be obtained from manufacturers, these were estimated using data from similar products listed in an International database provided by the Australian Food Standards Agency (NUTTAB 2006). Individual recipes used by participants were also added to Dietplan and cooking losses were automatically calculated by the software.
Assessment of plasma phospholipid fatty acid status
Fasting plasma phospholipid fatty acids were measured to provide an objective indication of dietary compliance to the fat manipulation. Lipid extraction, phosphatidylcholine isolation using solid-phase extraction, transmethylation and methyl ester separation by gas-phase chromatography were carried out using methods described previously(Reference Bondia-Pons, Morera-Pons and Castellote11). Fatty acid methyl esters were identified by comparison of retention times against known standards, Supelco 37 component FAME mix and PUFA-3 Menhaden oil (Supelco). Due to previous findings that changes in lipid profile in response to DHA supplementation differ between apoE4 carriers v. non-carriers(Reference Olano-Martin, Anil and Caslake6, Reference Caslake, Miles and Kofler12, Reference Minihane, Khan and Leigh-Firbank13), phospholipid fatty acid status was analysed with respect to genotype in order to ascertain whether the E4 isoform may alter incorporation of LC n-3 PUFA into phospholipids. To our knowledge, only two studies have examined phospholipid fatty acid status with respect to genotype(Reference Olano-Martin, Anil and Caslake6, Reference Plourde, Vohl and Vandal14), both with relatively small subject numbers (n 8 carriers, n 20 non-carriers and n 18 carriers, n 20 non-carriers, respectively).
Statistical analysis
SPSS (version 17.0; SPSS, Inc.) was used to perform all statistical analysis. Variables which were not normally distributed (determined by the Shapiro–Wilk test) were subjected to either logarithmic (ln or log10) or square-root transformation. A general linear model was used to compare the dietary data at baseline and during the three dietary periods. Significant differences were explored using paired t tests with a Bonferroni correction. Variables which could not be normalised (%E alcohol, %E protein, %E non-milk extrinsic sugar, vitamin D, %E MUFA, %E n-3 PUFA, %E n-6 PUFA, Na, EPA, docosapentaenoic acid, phospholipid fatty acid data) were compared using Friedman's non-parametric test and significant differences were explored using Wilcoxon's signed-rank test with Bonferroni correction. Sex and genotype were examined as between-participant factors. Plasma phospholipid fatty acid data were not normally distributed and so were compared using Friedman's non-parametric test, and significant differences were explored using Wilcoxon's signed-rank test with Bonferroni correction. Differences in the phospholipid fatty acid data between the genotype groups were determined using a Mann–Whitney U test. P values ≤ 0·05 were deemed to be significant.
Results
Of the total participants, eighty-eight, n 44 E3/E3 (twenty-two males and twenty-two females) and n 44 E3/E4 (twenty-five males and nineteen females), completed the study. Participants who dropped out of the study cited difficulties complying to either a LF or HSF diet, or problems with swallowing the study capsules. In those who completed the study, capsule compliance rates determined by the number of returned capsules were 95·0 % for the LF diet, 93·8 % for the HSF diet and 86·2 % for the HSF-DHA diet. Of a possible 352, 322 diet diaries were completed and returned by the participants for analysis. The reported habitual diets of the participants were comparable with the typical UK diet(Reference Bates, Lennox and Swan15) (see Table S2 of the supplementary material, available online at http://www.journals.cambridge.org/bjn).
Dietary data
Diet × genotype interactions were not observed for either the total energy or macronutrient intakes. Therefore, the nutrient intake for the group as a whole is presented in Table 3. Total energy intake (both including and excluding alcohol) was significantly higher during the HSF and HSF-DHA dietary periods compared with the LF dietary period and at baseline. Total dietary fat (%E) was significantly reduced from 37·1 %E for the habitual diet to 25·1 %E during the LF diet (target 24 %), and then significantly increased to 42·8 and 41·0 %E for the HSF and HSF-DHA diets, respectively (target 38 %E). CHO was significantly increased from 45·4 %E at baseline to 55·1 %E during the LF diet (target 59 %E), and then significantly reduced to 42·2 and 43·6 %E during the HSF and HSF-DHA diets, respectively (target 45 %). Dietary protein intake was significantly lower in the HSF diets. SFA was significantly reduced from 13·2 to 8·3 %E (target 8 %E) during the LF dietary period, and significantly raised to 19·3 and 18·6 %E, respectively, on the HSF and HSF-DHA diets (target 18 %E).
Table 3 Reported composition of the diets (Mean values with their standard errors)

LF, low fat; HSF, high saturated fat; HSF-DHA, high saturated fat plus DHA; %E, percentage of food energy; CHO, carbohydrate; DPA, docosapentaenoic acid; NMES, non-milk extrinsic sugars.
a,b,c Mean values within a row with unlike superscript letters were significantly different.
Habitual LC n-3 PUFA intakes of 69·8 mg/d (total EPA, docosapentaenoic acid and DHA) were evident, an amount marginally lower than observations in the general UK population (the SACN reported an intake of 0·1 g/d in 1994(1)). Inclusion of the study DHA-rich capsules increased intakes to 3·8 g/d, of which 80·3 % was DHA. When the supplement intake is excluded, dietary DHA intake was not significantly different across all diets. Fibre, starch and sugar intakes were significantly higher during the LF diet compared with the other diets.
Apart from a difference in overall energy intake and fibre, there were no significant differences in the dietary intake between the male and female participants during the intervention period, which suggests equal compliance to the diets (data not shown).
To assess the quality of the dietary data, Schofield equations were used to estimate BMR. Values were multiplied by a physical activity level of 1·6 to calculate the participants' average energy requirements. Based on these calculations, participants appear to have under-reported their energy intakes both at baseline and during the LF diet, as reported energy intakes were lower than required energy intakes by 16·9 and 24·0 %, respectively. Similarly during the HSF and HSF-DHA diets, values of under-reporting were 3·1 and 7·4 %, respectively. However, these conclusions are based on the assumption that the participants maintained a constant body weight throughout the intervention. In the case of the LF diet, there was a small reduction in the body weight of approximately 1 kg, which was clinically insignificant, but did reach statistical significance (P < 0·001). The mean body weight of the participants was as follows: visit 1 (baseline) 76·5 (sd 1·6) kg, visit 2 (post-LF diet) 75·7 (sd 1·5) kg, visit 3 (post-HSF diet) 76·5 (sd 1·5) kg, visit 4 (post-HSF-DHA diet) 77·5 (sd 1·5) kg. This suggests that 24 % under-reporting during the LF dietary arm was an overestimate.
Phospholipid fatty acid composition
At baseline, 44·9, 13·6 and 41·5 % of plasma phospholipids were SFA, MUFA and PUFA, respectively, with no significant diet × genotype interaction evident for these fatty acid classes during the sequential dietary intervention. In the group as a whole, the proportion of EPA (2·9 % v. 5·1 %, P < 0·001) and DHA (8·2 % v. 4·1 %, P < 0·001) increased by 2-fold following consumption of DHA-rich capsules for 8 weeks (Fig. 1(a) and (c), respectively). There was no significant change in any other measured plasma phospholipid fatty acids in the group as a whole or according to the APOE genotype (Fig. 1).

Fig. 1 Mean proportions of (a) EPA, (b) DPA (docosapentaenoic acid) and (c) DHA in plasma found in the group as a whole (■), E3/E3 individuals (□) and E3/E4 individuals (![]() ). LF, low-fat diet; HSF, high-saturated fat diet; HSF-DHA, high-saturated fat plus DHA diet. Values are means, with standard errors represented by vertical bars. * Proportions of EPA and DHA were significantly higher after the HSF-DHA diet v. the other dietary periods (P < 0·001).
). LF, low-fat diet; HSF, high-saturated fat diet; HSF-DHA, high-saturated fat plus DHA diet. Values are means, with standard errors represented by vertical bars. * Proportions of EPA and DHA were significantly higher after the HSF-DHA diet v. the other dietary periods (P < 0·001).
Discussion
Achievement of dietary targets
The dietary strategy developed for the SATgenɛ study was successfully implemented using commercial food items and dietary targets were broadly met. In general, compliance of the participants lead to overachievement of the targets particularly with regard to fat intake, where the mean %E from fat intake during the HSF diets was 42·8 and 41·0 % for HSF and HSF-DHA, respectively (target 38 %). These results can probably be attributed to the high motivation among the participants, the continuous support and encouragement supplied by researchers, and also the careful selection of a wide range of desirable study foods in order to prevent ‘product boredom’. However, it must also be pointed out that there may be inaccuracies in the dietary data due to ‘desirability bias’, i.e. participants recording what they had been asked to consume rather than what they actually had eaten. Compared with other dietary manipulation strategies, the SATgenɛ exchange model was unique because commercially available products were exclusively used to aid achievement of dietary targets as opposed to using products specifically formulated for the study(Reference Shaw, Tierney and McCarthy7, Reference Moore, Gitau and Goff8, Reference Nydahl, Smith and Kelly16). The advantage of using commercial products available in the supermarkets is that the specified diets used in SATgenɛ could be easily used by other investigators wishing to investigate similar dietary targets. Furthermore, the diets were palatable, well tolerated and acceptable to the study participants, although many of the HSF products were more popular among the volunteers than the LF products. The results illustrate that marked dietary manipulation can be successfully implemented, using commercial foods over a relatively long dietary intervention period.
In the present study, subjects were required to record 3 d diet diaries during each of the intervention periods. Limitations of this approach include the chance of missing less frequently consumed foods such as fish. In addition, the available nutrient databases contain incomplete information on the LC n-3 PUFA content of some foods, which may have contributed towards an underestimation of LC n-3 PUFA consumption in our subjects. These issues should be addressed in future dietary intervention studies.
There are significant seasonal effects on dietary intake which can be an important confounder in dietary intervention studies, particularly those which are not randomised. The nature of the present study design did not allow random allocation of participants to the diets. However, within the SATgenɛ study, seasonal influences were reduced by splitting the subject group into two cohorts, which commenced their sequential diets at different times of the year (July–January or January–July), and staggering the baseline dates of the volunteers. Each cohort was also balanced for sex and number of apoE3/E3 and E3/E4 individuals.
One of the aims of the present study was that the three diets were isoenergetic. However, according to the dietary data, energy intake (both including and excluding alcohol) was significantly higher during the HSF diets compared with the LF and habitual diets, possibly due to the desirability and overconsumption of the HSF snacks. Many volunteers also commented that being on the study gave them an ‘excuse’ to eat other high-fat foods in excess. The consequential lower dietary energy intake during the LF dietary period may have reflected the challenge of replacing the dietary energy from fat with sufficient energy from CHO. Both the RISCK(Reference Moore, Gitau and Goff8) and LIPGENE(Reference Shaw, Tierney and McCarthy7) multicentre dietary intervention studies have also reported that subjects had a lower energy intake while following LF diets compared with HSF diets despite the diets being designed as isoenergetic. The subjects' weight decreased by 1·1 % by the end of the LF dietary period and increased by 0·7 % by the end of the HSF-DHA dietary period. Although statistically significant, these weight changes would be predicted to have minimal clinical significance, as they equated to less than 1 kg in both cases. This magnitude of weight change was also observed during the LF diets of both the LIPGENE(Reference Shaw, Tierney and McCarthy7) and RISCK(Reference Jebb, Lovegrove and Griffin17) studies.
Protein intakes also varied during the intervention as higher levels were consumed during the HSF diets v. the LF diets. This could possibly have been due to the fact that, on average, there was a higher protein content in the LF snacks than in the HSF snacks (see Table S1 of the supplementary material, available online at http://www.journals.cambridge.org/bjn). As expected, replacing fat with CHO led to higher intakes of fibre, starch and sugar during the LF diet compared with the other diets. An inadvertent rise in both salt and non-milk extrinsic sugar intake during the HSF diets could be expected due to the nature of the snacks provided, yet Na was not significantly different across all diets. The %E from non-milk extrinsic sugar was in fact lower during the intervention diets compared with the participants' habitual diets. After examination of the diet diaries, it was evident that subjects followed the instructions to keep their fruit and vegetable intake constant throughout the intervention. The higher sugar intake reported during the LF diet could be attributed to an increase in milk consumption, which may have been associated with extra breakfast cereal eaten to achieve the advised increase in CHO intake. It should be noted that the manner in which subjects chose to increase their CHO intake may have differed since starchy foods were not provided as part of the study.
The increase in EPA plasma phospholipid levels could be due to a combination of the 0·5 g/d of EPA present in the DHA-rich supplements and/or the endogenous retro-conversion of DHA consumed. This and the 2-fold increase in the proportion of DHA in plasma phospholipids provide evidence of capsule compliance. The observation that total SFA did not increase after the HSF and HSF-DHA diets supports previous studies that have indicated plasma saturated fat content is unlikely to reflect dietary intake since SFA can be synthesised endogenously(Reference Arab18). APOE genotype did not have an impact on baseline or post-treatment phospholipid fatty acid status. This supports data found in previous studies(Reference Olano-Martin, Anil and Caslake6, Reference Plourde, Vohl and Vandal14) in which similar proportions of EPA and DHA were observed in plasma phospholipids after supplementation with LC n-3 PUFA in E4 carriers v. non-carriers. Interestingly, in the study of Plourde et al. (Reference Plourde, Vohl and Vandal14), a genotype effect was observed on the EPA and DHA content of plasma NEFA and TAG, respectively, with a lower incorporation evident in E4 carriers v. non-carriers, a finding worthy of further investigation.
Challenges encountered
A number of challenges were encountered during the running of the SATgenɛ study. Keeping a large group of volunteers with varying lifestyles and dietary habits motivated to adhere to unfamiliar diets and consume often novel products during a 24-week intervention period was certainly a challenge. The first task was to select products that were palatable and sufficiently varied to promote compliance, and, overall, the diets had to be nutritionally adequate while achieving the required dietary targets. One problem experienced by the researchers was that some of the products used were discontinued by the manufacturers during the study and therefore no longer available to the participants. In such cases, similar alternative products were sought, but this did result in some products differing between the two cohorts. Providing a range of foods that was suitable for vegetarians was important so as not to exclude this group from the study.
Due to the 6-month duration of the intervention, most of the participants went on holiday during this period and were therefore unable to completely abide to the prescribed diets. Holidays and social events such as Christmas also added to weight fluctuations among the participants, which could not be controlled. Such problems were overcome by suggesting alternative foods that may be consumed if subjects were eating outside of the home. The fact that all study snacks could be stored at ambient temperatures meant that volunteers could easily take these on holiday with them.
Logistically, storage of foods can be a challenge for large human dietary studies where intervention foods are provided to the participants. In the case of the SATgenɛ study, storage of the snack foods required a large dry area at ambient temperature. Butter was purchased in large amounts and frozen at − 20°C until required for consumption when it was defrosted before distribution to the subjects. However, this method of storage was unsuitable for the very-low-fat spread and so a constant supply needed to be purchased and kept refrigerated at 4°C. Required food volumes were estimated based on the number of volunteers, but inevitably some snacks were more popular than others which led to wastage. Some of the baked goods had short shelf lives, which meant that these products often went past their ‘best before’ date before the subjects had a chance to consume them in the 4-week period between the food collection visits. In these cases, additional ‘in date’ snacks were delivered to, or collected by the subjects. Or, if more convenient, subjects were asked to purchase replacement snacks and the money spent was reimbursed. Supply of all intervention foods greatly improved compliance to the dietary instruction and allowed the dietary targets to be met.
In conclusion, the dietary exchange model and strategy employed to implement the diets of varying fat content and composition was successful using commercially available food items. This resulted in good compliance to dietary prescription with achievement of overall dietary target in the SATgenɛ study. Dietary analysis and plasma phospholipid fatty acid composition supported high compliance rates among the participants.
Acknowledgements
SATgenɛ was funded by the Wellcome Trust (WT085045MA). With many thanks to Croda Healthcare (UK) for supplying the DHA-rich capsules and for encapsulating the placebo oils supplied by AarhusKarlshamn UK Limited. We would also like to thank Yujie Liu and Julie Orsini who helped with the dietary analysis, Michelle Weech who helped with the GC analysis, Jan Luff for help with recruitment and all the volunteers for their time and dedication to the study. A. M. M., K. G. J. and J. A. L. designed the study. S. L. developed and implemented the dietary strategy and performed the statistical analysis. S. L. and M. T. performed the dietary analysis. A. L. C.-W., M. T. and S. L. performed the GC analysis. S. L. and J. A. L. prepared the manuscript. K. G. J., A. M. M. and A. L. C.-W. contributed to and approved the final manuscript. The authors had no conflicts of interest.






