Background
Primary health care is regarded as a fundamental constituent of the health care system in Sweden. It provides ambulatory care outside hospitals and general practice is the core medical speciality. This care is provided by more than 4000 general practitioners (GPs) who carry out about 12.2 million consultations per year (Landstingsförbundet, 1999). Statistics from primary health care in Sweden (Department of Public Health, 2001), as well as from other Nordic countries (Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996; Tyssen, Reference Tyssen2001), have been sparse. The number of clinical problems per encounter has been reported in some countries (Pringle et al., Reference Pringle, Ward and Chilvers,1995; Månsson et al., Reference Månsson, Marklund and Hultborn,2001), and statistics concerning managed morbidity are found in several studies (Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996; Keast et al., Reference Keast, Marshall, Stewart and Orr,1999; Department of Public Health, 2001; Grimsmo et al., Reference Grimsmo, Hagman, Falko, Matthiessen and Njálsson,2001; Britt et al., Reference Britt, Miller, Knox, Charles, Valenti, Henderson, Pan, Sutton and Harrison,2002). Gender and other characteristics of the GP and their effect on conditions managed, medications prescribed, preventive screening, time spent in encounters, and patient characteristics have also been studied (Britt et al., Reference Britt, Bhasale, Miles, Meza, Sayer and Angelis,1996; Sayer and Britt, Reference Sayer and Britt,1997; Henderson and Weisman, Reference Henderson and Weisman,2001; Tabenkin et al., Reference Tabenkin, Goodwin, Zyzanski, Stange and Medalie,2004).
The health care system is undergoing rapid change, and we will continue to see changes involving both organisation and new techniques. The use of electronic patient records (EPR) by GPs is almost universal in Sweden, as is also the case in several other countries such as the UK and the Netherlands. In Swedish everyday clinical practice there is a widespread tradition of using a primary care version of the International Classification of Diseases and Related Health Problems for diagnostic coding (ICD-10) (Socialstyrelsen, 1997; Nilsson et al., Reference Nilsson, Åhlfeldt and Strender,2002). In the future, the EPR will be an increasingly important source of information (Grimsmo et al., Reference Grimsmo, Hagman, Falko, Matthiessen and Njálsson,2001). In one study of the accuracy of EPR, a vast majority of the diagnostic codes in the records were found to be correct when compared with the textual content (Nilsson et al., Reference Nilsson, Åhlfeldt and Strender,2003). No important lapses in the recording of health problems and diagnoses were found when compared with the actual consultation process (Pringle et al., Reference Pringle, Ward and Chilvers,1995). Today these records are used mainly in the clinical care of patients, and have little to offer regarding the future reuse of data.
The general aim of this study was to investigate EPR in everyday general practice. In the first phase we investigated the structure and textual content of the records, and the accuracy of diagnostic codes (Nilsson et al., Reference Nilsson, Åhlfeldt and Strender,2003). The aim of this part of the study was to investigate types of encounters, managed diseases and health problems, and characteristics of patients and GPs.
Methods
Participating GPs
The GPs were chosen from 6072 registered specialists in family medicine in Sweden who were under the age of 65 years. We randomly selected 26 who lived in Stockholm and who were professionally active in general practice in that city (with permanent employment status or contracts for longer than six months), and they were asked to provide data for this study. Twenty GPs (response rate 76.9%) from 20 different primary health care centres agreed to do so. The GPs in the area work in team with district nurses, and provide primary care for a specified population.
Procedure
Twenty direct encounters (ie, face-to-face meetings between a patient and a GP) between November 1999 and October 2000 (one-year study period) were randomly selected and examined retrospectively for each GP, for a total of 400 EPR. To identify each record we used random numbers, firstly to select a specific day and secondly to select a specific encounter that day. All records were printed on paper and anonymised. The type of encounter was derived from a model used in the area that differentiates between home and office encounters, and planned and unplanned (ie, appointment made the same day) encounters.
The number of health problems, defined as all problems mentioned in the free text part of the record and/or as diagnostic codes, was determined in each record. The available diagnostic codes were registered, and health problems with a missing diagnostic code were coded by one of the authors (GHN). All diagnostic codes were thereafter analysed according to their frequencies and distribution in ICD-10 chapters.
The regional ethical review board in Stockholm approved the study.
Statistical analysis
When comparing participating and non-participating GPs, independent two-sample t-tests were used to compare age and χ 2 was used to test differences in sex.
We have a multi-level model with three levels: diagnoses, patients/encounters and GPs. In this study we have only one encounter per patient, so that in the patient/encounter level, patients and encounters have the same value. At one encounter several diagnoses may be managed. We used regression models to investigate correlations while compensating for a higher level. In multiple regression analyses, nominal variables were treated as dummy variables. When the dependent variable was dichotomous, multiple logistic regression was used.
The first regression model had patient sex as the dependent variable and ICD-10 chapters (dummy variable), patient age, GP age and sex (dummy variable) as independent variables. In the second regression model where encounter constitutes the basic level and GPs the second level, we used the number of diagnoses in the encounter as the dependent variable and the GPs’ propensity to manage health problems in each encounter (the mean number of diagnostic codes among 20 encounters) as the independent variable. Other independent variables were the age and sex of the patients (dummy variable) as well as the age and sex of the GPs. In the third regression model the GPs’ sex was the dependent variable and the patient’s age and sex (dummy variable) were independent variables. In the fourth regression model the GPs’ propensity to manage many health problems in each encounter was the dependent variable, and the GPs’ age and sex (dummy variable), and the mean age and sex ratio among the GPs’ patients as independent variables.
Comparisons between participating and non-participating GPs were analysed using the SPSS® software programme version 11.0 (SPSS, 2001). For multiple regression and logistic regression, the Epi-Info™ version 3.3 (CDC, Atlanta, GA, USA) was used.
Results
No significant differences with respect to age and sex were found between the participating GPs and the six non-participating GPs. Twelve of the 20 GPs were females and the mean age was 51.3 years. All GPs used the Swedish primary care version of the ICD-10 for labelling health problems (Socialstyrelsen, 1997). Coding of health problems in clinical practice was done by the GPs.
Five (1.3%) of the 400 encounters were home encounters and the others were office encounters. One hundred and ninety (47.5%) of the encounters were planned, 168 (42.0%) were unplanned, and whether the others (10.5%) were planned or unplanned could not be determined.
Diseases and health problems
A total of 422 diagnostic codes were identified. A further 135 health problems were only described in free text (and these were coded afterwards within the study). Thus, a total of 557 clinical problems, as defined above, were identified in the 400 records. The mean number of clinical problems per encounter was 1.4 (95% confidence interval (CI) 1.3–1.5). One health problem/diagnostic code was identified in 73.5% of the encounters, two in 17.3%, three in 7.0%, four in 1.5%, five in 0.5% and seven in 0.3% of the encounters.
The most frequent diagnostic codes were for essential hypertension (9.3% of the encounters) and acute upper respiratory infections at multiple and unspecified sites (Table 1). Fourteen diagnoses accounted for about one-third of the managed problems.
Table 1 The 15 most common diseases and health problems managed in 400 encounters, across ICD-chapters (in the Swedish Primary Health Care version of ICD-10) in descending order
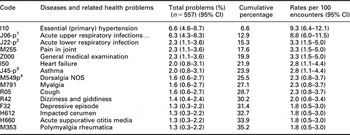
1Includes J00 and J06 in ICD-10.
2Includes J20, J21 and J22.
3Includes J45 and J46.
4Includes M540, M541, M548 and M549.
The most frequent ICD-10 chapters were diseases of the musculoskeletal system (22.0% of the encounters), diseases of the respiratory system, diseases of the circulatory system, and symptoms and abnormal clinical findings (Table 2).
Table 2 Distribution of diseases and health problems managed in 400 encounters, across ICD-chapters in the Swedish primary health care version of ICD-10 (in which there is no chapter 20)
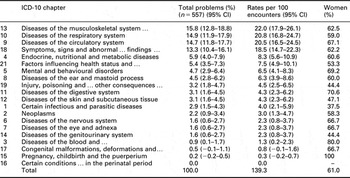
In the first regression model male patients, as compared with female patients, less often received a diagnostic label from chapter 5 (Mental and behavioural disorders, odds ratio 0.24, 95% CI 0.064–0.94, P = 0.040), chapter 9 (Diseases of the circulatory system, odds ratio 0.24, 95% CI 0.075–0.79, P = 0.018) and chapter 13 (Diseases of the musculoskeletal system and connective tissue, odds ratio 0.31, 95% CI 0.099–0.97, P = 0.045).
Characteristics of the patient
The mean age of the patients was 51.2 years (95% CI 48.6–53.7) and 57.5% were women (95% CI 50.4–64.6). The predominant age group was 75+, accounting for 30.2% of the encounters, whereas the age group 0–14 years accounted for 9.4%. In all, 61% of the health problems concerned women (Table 2).
In the second regression model higher patient age was strongly associated with having more problems managed at a single encounter to a GP (P = 0.000001).
In the third regression model a tendency was seen for patients to encounter a GP of the same sex (odds ratio 1.5, 95% CI 1.00–2.26, P = 0.053). Furthermore, there was a weak tendency for older patients to encounter male GPs (P = 0.099).
Characteristics of the GPs
The GPs’ propensity to manage a problem differed; the average number of managed problems in an encounter varied between 1.0 and 2.1. The proportion of female patients varied between 45% and 80% for different GPs, and the mean age of their patients varied between 31.0 and 64.3 years.
The fourth regression model showed that GPs with older patients tended to manage more health problems than GPs with younger patients (P = 0.005). Furthermore, there was a tendency for male GPs to manage an average of 0.27 fewer health problems in each encounter than female GPs (P = 0.057).
Discussion
We found that two diagnoses, four diagnostic groups, women and the elderly were predominant. Female and male patients had different diagnostic panoramas and they had a tendency to encounter a GP of the same sex. Different GPs’ patients differed regarding sex, age and number of health problems managed.
Methodological aspects
An advantage of our study is that the selection of GPs and encounters was done randomly, and that it is based on a one-year study period. We believe, therefore, that the results are fairly representative for the area, and partially representative for urban general practice in Sweden. However, the small sample size is a limitation of the study and makes the reliability of some of the results questionable.
The study required manual reading of all the free text in all the records investigated during the one-year period. Thus, for practical reasons the sample size was limited and only 26 GPs were invited to participate, each with 20 randomly selected encounters.
Since this study uses a two-stage cluster sampling approach, we end up with data in multiple levels. All data processing aimed at producing a P value adjusted for both levels of this multi-level model. Multi-level models can be handled in different ways. The basic structure of a multi-level model is an extension of ordinary least squares regression. Advanced extensions are found in specialised software, and common statistical programs such as SPSS have developed specialised commands to perform some multi-level modelling. However, in less-complicated models an ‘ordinary’ regression model may be used (Rice and Leyland, Reference Rice and Leyland,1996), which is the approach we applied in this study.
It can be assumed that the coding of diseases and health problems seen in our study is fairly accurate in terms of the actual care process. In the first phase of this study, a vast majority of the diagnostic codes in the records used in our study were found to be highly complete and correct compared with the textual content (Nilsson et al., Reference Nilsson, Åhlfeldt and Strender,2003). The complementary coding of health problems in our study has further improved the completeness of coding, but this limits the comparability of results from other studies using a different approach since the correctness of coding may have been affected to a limited degree.
Diagnoses and health problems
The mean number of clinical problems per encounter (1.4) is in accordance with figures of 1.2–1.6 reported in other studies (Pringle et al., Reference Pringle, Ward and Chilvers,1995; Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996; Månsson et al., Reference Månsson, Marklund and Hultborn,2001; Britt et al., Reference Britt, Miller, Knox, Charles, Valenti, Henderson, Pan, Sutton and Harrison,2002). However, comparing statistics on diagnostic codes and groups is somewhat problematic, as clinical concepts (eg, dyspepsia) can often be found in several ICD-10-chapters (Rector, Reference Rector2000), and consequently the results can partially reflect the individual GPs’ tradition of diagnostic coding. Further, comparisons with data from outside Sweden are limited, since most countries use the International Classification of Primary Care (ICPC-2) (WICC, 1998). The different chapter distribution in ICPC-2 makes comparisons at the chapter level particularly troublesome. Morover, comparisons are complicated by many differences between urban and rural areas.
The results concerning diagnostic groups (ICD-10 chapters) are roughly similar to those obtained in other studies (Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996; Department of Public Health, 2001; Grimsmo et al., Reference Grimsmo, Hagman, Falko, Matthiessen and Njálsson,2001). One Swedish study in Tierp reported much lower figures for diseases of the circulatory system (7.7% of all problems) than in our study (Department of Public Health, 2001), while the figures for injuries (10.2%), diseases of the genitourinary system (6.1%) and diseases of the eye (4.5%) are markedly higher than in our study. This indicates that these health problems account for a lesser proportion of the clinical workload by GPs in our study. This is possibly due to the availability in this part of the country of a large number of specialists in these areas (ie, gynaecologists and ophthalmologists) in primary health care, and easy access to hospital emergency departments. Our figures for the diagnostic groups musculoskeletal system and circulatory system are markedly higher compared with the study in Iceland, where these groups accounted for only 9.0% and 4.8% of all problems, respectively (Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996). Further, our figures for diseases of the skin and subcutaneous tissue are markedly lower in comparison with the study in Australia, where these diseases accounted for as much as 11.2% of all problems (Britt et al., Reference Britt, Miller, Knox, Charles, Valenti, Henderson, Pan, Sutton and Harrison,2002). This is likely to be due to the use of the different classifications. In ICD-10 all skin malignant neoplasms are classified in the neoplasm chapter, several symptoms from the skin in the symptom chapter and all skin injuries in the injury chapter, whereas in ICPC-2 all these go into the skin chapter.
The results concerning distribution of single codes are similar in some respects to results in the studies mentioned above (Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996; Department of Public Health, 2001; Grimsmo et al., Reference Grimsmo, Hagman, Falko, Matthiessen and Njálsson,2001). The most common single diagnostic code, essential hypertension, is, however, even more predominant in our study (6.6% of all problems), while accounting for only 2.9% in the Swedish study in Tierp and 2.4% in Iceland (Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996; Department of Public Health, 2001). Nevertheless, similar figures for hypertension (6.3%, including complicated hypertension) have been reported in Australia (Britt et al., Reference Britt, Miller, Knox, Charles, Valenti, Henderson, Pan, Sutton and Harrison,2002). On the other hand, figures for skin injuries are much higher (4.8%) in the Swedish study (Department of Public Health, 2001). The results for both upper (J06-p) and lower (J22-p) respiratory tract infections are in line with the studies mentioned above, and the total figure for these codes in our study is about 12% of all problems. The frequent use of GPs for these health problems can be explained by reports that most of these patients have complications rather than simple colds (Keast et al., Reference Keast, Marshall, Stewart and Orr,1999), and possibly also by the high rate of unplanned encounters (42%) in our study. At the time of the study, such easy access to general practice (without making an appointment by telephone) was stipulated as mandatory by the county council.
After compensating for patients’ ages and basic characteristics in the next data level, GPs’, it was found that female patients as compared with male patients more often received a diagnostic label from chapters 5, 9 and 13. This is somewhat in accordance with prevalence studies in primary health care, although not based on the ICD-10 or evaluated with a logistic regression model (Njálsson et al., Reference Njálsson, Sigurdsson and McAuley,1996; Tyssen, Reference Tyssen2001).
The patient view
The proportion of female patients was in line with other studies reporting 54–60% females (Department of Public Health, 2001; Grimsmo et al., Reference Grimsmo, Hagman, Falko, Matthiessen and Njálsson,2001; Britt et al., Reference Britt, Miller, Knox, Charles, Valenti, Henderson, Pan, Sutton and Harrison,2002). The elderly comprised a higher proportion than in one study reporting 12.3% in the age group 65–74 years and 12.8% in the age group 75+ (Britt et al., Reference Britt, Miller, Knox, Charles, Valenti, Henderson, Pan, Sutton and Harrison,2002).
Not surprisingly, this study showed that higher age in patients was strongly associated with a larger number of diagnostic codes in a single encounter. The tendency for patients to encounter a GP of the same sex has been reported elsewhere (Bensing et al., Reference Bensing, van den Brink-Muinen and de Bakker,1993), as has the weak tendency for older patients to encounter male GPs. That female GPs see different health problems than male GPs has also been reported (Bensing et al., Reference Bensing, van den Brink-Muinen and de Bakker,1993; Sayer and Britt, Reference Sayer and Britt,1996), with a predominance of mental and circulatory problems as in our study. However, the predominance of musculoskeletal problems found in our study was not seen in these studies. The question can be raised as to whether the gender differences in practice style may represent a choice made by the patient, the GP or another staff member assisting the GP.
The GP view
In our study GPs differ regarding their propensity to manage a health problem, the proportion of female patients they see, and the mean age of their patients. As expected, GPs with older patients have a greater propensity to manage a health problem. When adjusting for known variables in this multi-level model, female GPs tend to manage more health problems than male GPs, which has been reported previously (Bensing et al., Reference Bensing, van den Brink-Muinen and de Bakker,1993). This may reflect an unknown difference in patients handled by female as compared with male GPs, or suggest that female and male GPs act differently even when presented with similar patients (Britt et al., Reference Britt, Bhasale, Miles, Meza, Sayer and Angelis,1996).
Conclusions
We found that two diagnoses (essential hypertension and acute upper respiratory infections), four diagnostic groups, women and the elderly are predominant. Female and male patients have different diagnostic panoramas and they have a tendency to encounter a GP of the same sex. GPs differ regarding their patients’ characteristics, including sex, age and number of health problems managed at each encounter.
Acknowledgements
We thank all the GPs who participated in the study. The study was supported by grants from the Stockholm County Council.




