Early detection is one of the cornerstones of early intervention in first-episode psychosis (Reading & Birchwood, et al, 2005), yet there have been relatively few evaluations of strategies to improve early detection (Reference Falloon, Coverdale and LaidlawFalloon et al, 1998; Reference Krstev, Carbone and HarriganKrstev et al, 2004; Reference Melle, Larsen and HaahrMelle et al, 2004; Reference Tait, Lester and BirchwoodTait et al, 2005; Reference Chong-Siow, Mythily and VermaChong-Siow et al, 2005; Reference Malla, Norman and ScholtenMalla et al, 2005). There is even less research on whether early detection strategies impact on clinical outcome (Reference Melle, Larsen and HaahrMelle et al, 2004; Reference Johannessen, Larsen and JoaJohannessen et al, 2005). The main strategies employed by early detection programmes aim to raise awareness among referrers and provide rapid easy access to mental healthcare and/or early intervention teams. Some programmes focus on one particular step in the pathway to care, for example primary care to mental healthcare (Reference Tait, Lester and BirchwoodTait et al, 2005), whereas others attempt to broadly target all the steps through intensive community health education programmes (Reference Johannessen, Larsen and JoaJohannessen et al, 2005). The former may only have limited impact on the overall delay, while the latter may prove very expensive to administer and result in many inappropriate referrals. Both are likely to require significant ongoing investment to maintain awareness and facilitate easy and rapid access to treatment. Determining the relative benefits of each will be an invaluable guide to future service provision.
There is now a substantial body of evidence demonstrating that delays in accessing care are significantly associated with time to treatment response, remission rates, and relapse rates in these patients (Reference Marshall, Lewis and LockwoodMarshall et al, 2005). These delays in treatment, as measured by the duration of untreated psychosis (DUP), are an average 1 year in nonaffective psychosis, with a median of 3–6 months. If the preceding prodromal period is included (which is typically 1 year), then the total delay amounts to approximately 2 years. These delays are indicative of major shortcomings in the provision of mental healthcare and are associated with a significant level of distress and morbidity.
The DUP represents the accumulated delay in each step in the pathway to care, starting with the delay in patients' own responses to the onset of their psychosis and finishing with the delay in mental health services' engagement of patients in treatment. There are six main steps in the pathway (see Fig. 1), relying on the recognition, decisions and actions of (a) the patient, then (b) the carer, friends and associates, (c) non-health professionals such as community agencies, (d) health professionals such as general practitioners, accident and emergency staff, and (e) mental health professionals. Most patients are likely to move through each of these steps, facilitated at each step by the processes of help-seeking, engagement, recognition, services provided, and referral to the next step. Exactly where obstacles and delays occur within each step or which steps provide the greatest potential for reducing the DUP remains unclear. But studies suggest that as many as 45% of cases with psychosis in the general population never actually reach the final step of successfully engaging in treatment (Reference Link, Dohrenwend, Dohrenwend, Dohrenwend and GouldLink & Dohrenwend, 1980). This proportion appears to have dropped markedly for more recent and younger generations as social trends in accessing mental healthcare services have generally improved.
General practitioners represent an important step in the pathway to care (see steps 4 and 5: Fig. 1) and are often the first point of contact with health services by patients with psychosis (Reference Cole, Leavey and KingCole et al, 1995). There is evidence that patients with GPs have shorter DUPs and as a group are less likely to avoid health threats (Skeate et al, 2002). GPs are well placed to play a greater role in early detection. However, recognising the initial signs of first-episode psychosis remains a challenge for many GPs and they are unlikely to refer without a better understanding of how best to access specialist mental health services (Reference Shiers and LesterShiers & Lester, 2004; Reference Tait, Lester and BirchwoodTait et al, 2005).
There are at least four published evaluations of early detection programmes in first-episode psychosis populations, showing variable results. The most impressive is the TIPS study from Norway (Reference Larsen, McGlashan and JohannessenLarsen et al, 2001), reporting a reduction in the DUP from a mean of 114.2 weeks (median 26.0, s.d.=173.6) to 25.3 weeks (median 4.5, s.d.=61.7) after the introduction of an early detection programme (intensive community education campaign and access to an early detection team on weekdays to lower the threshold of entry into specialised mental health services). The study also demonstrated a shorter DUP and better outcome in Positive and Negative Syndrome Scale (PANSS) and Global Assessment of Functioning (GAF) score at 3-month follow-up (Reference Melle, Larsen and HaahrMelle et al, 2004), although the outcomes were not maintained at 1 year, with the intervention having a small effect on negative symptoms (Reference Larsen, Melle and AuestadLarsen et al, 2006). In Singapore, the Early Psychosis Intervention Clinic programme reported a lowering of the median DUP from 12 months to 4 months following the introduction of a public health campaign and GP education programme. In Melbourne, a GP education programme run by the Early Psychosis Prevention and Intervention Centre similarly reported results that were confounded by the engagement of previously undetected patients with long DUPs in the intervention sector and when patients with very long DUPs were excluded from the analysis the DUP in the intervention sector was significantly shorter (Reference Krstev, Carbone and HarriganKrstev et al, 2004). The remaining study in Canada reported no difference in DUP with a community-wide education programme run by the ECIP programme in London Ontario (Reference Malla, Norman and ScholtenMalla et al, 2005). Indeed, it appeared that the intervention may bring into treatment patients who have been ill for long periods of time and have higher levels of psychopathology. They suggested a more targeted approach directed at primary care and emergency services.

Fig. 1 Measurement of duration of untreated psychosis (DUP) and delays in the pathway to care. BLIP, brief limited intermittent psychosis; MHS, mental health service, i.e. any mental health professional.
The aim of this study is to determine two main factors. First, whether providing GP training in recognising early psychosis results in these GPs (a) referring a greater proportion of the first-episode patients that they see and (b) making these referrals more quickly to mental health services. Second, whether providing GPs with direct access to an early detection team results in a quicker engagement in (a) initial assessment and/or (b) treatment. Overall, these interventions might result in first-episode patients who attend their GPs experiencing less delays in accessing specialist treatment.
METHOD
Setting
The borough of Lambeth (population 267 000) is an inner city suburb with a high level of social deprivation and a high proportion of migrants and people from minority ethnic groups. It has a high incidence of psychosis and social morbidity (Reference Garety and RiggGarety & Rigg, 2001). Lambeth's initial community mental health services are provided through five sector multidisciplinary assessment and treatment teams. Emergency after hours assessments are provided by mental health staff at accident and emergency departments and emergency clinics. In-patient services are based at Lambeth Hospital, St. Thomas' Hospital and the Maudsley Hospital. The borough has a well-established tertiary care early intervention service, the Lambeth Early Onset (LEO) service, which comprises an 18-bed acute in-patient unit, the LEO Unit, and an assertive outreach recovery team, LEO Community Team, which provides follow-up for 2 years (Reference Craig, Garety and PowerCraig et al, 2004; Reference Garety, Craig and DunnGarety et al, 2006).
Prior to the LEO CAT study all newly presenting patients with first-episode psychosis had to be referred and assessed first by one of the Lambeth's five sectors' assessment and treatment teams. All admissions of patients with first-episode psychosis were referred to the LEO In-patient Unit and subsequently followed-up by the LEO community team if meeting their criteria. There was no specific GP education or early detection programme in operation. LEO CAT was a new team established to provide a gateway into the LEO service and to link closely with GPs. It was funded for 2 years by the Guy's and St Thomas' Charity through a service development grant. A closely associated service (OASIS) for those with an at-risk mental state for psychosis (i.e. ultra-high risk) also commenced in south London at the same time as LEO CAT. The two teams worked closely together in providing GP education and assessments of those with suspected first-episode psychosis.
Design
The study involved a cluster randomised trial of GP education plus assignment of the practice to the early detection team (LEO CAT). GP practices randomised into the intervention group received both the GP education training and direct access to the LEO CAT team for referrals. GP practices in the control group received standard local mental health services (as described above) without the addition of GP training.
Participants
Patients. All patients aged 16–35 years, living in the south London borough of Lambeth and presenting to local mental health services (between June 2003 and August 2005) for the first time with first-episode psychosis were eligible for inclusion in the study. Psychosis was defined as a period of more than one week of unremitting psychotic symptoms meeting the criteria for ‘transition psychosis’ as defined by the Comprehensive Assessment of At-Risk Mental States (CAARMS) (Reference Yung, Yuen and McGorryYung et al, 2005). Patients consenting to the research interview formed the study sample. Patients were excluded if it was not their first treated episode or presentation, i.e. they had a history of contact with mental health services for psychosis for more than 6 months or antipsychotic treatment for more than a month (with greater than 50% treatment adherence).
GP practices. There were 62 GP practices in Lambeth prior to the start of the study and these were approached to formally consent to the study. Four practices refused, citing reasons such as ‘due to close shortly’ or ‘never see patients with psychosis’. The consenting 58 practices were grouped into 46 clusters as 12 practices had GPs common to more than one practice. The result was 23 clusters of practices in the intervention group and 23 in the control group. The randomisation was performed by an independent statistician.
The intervention
The intervention group practices were approached by LEO CAT and all staff offered one practice-based lunchtime training session in early detection. This involved showing a 10-min video, ‘A stitch in time: Psychosis, Get Help Early: a video for general practitioners’ (Early Psychosis and Intervention Centre, 1994) plus a 15-min presentation about LEO CAT and discussion about identifying the early signs of psychosis. Leaflets on LEO and reminders were distributed to these practices and the practices were encouraged to display them in their surgeries and waiting areas. Further follow-up and reminders about the benefits of early detection was provided on a case-by-case basis, with verbal feedback and discussions around individual cases referred. Six practices declined the formal lunchtime sessions citing time and work pressure constraints. The rest received the lunchtime sessions within the first few months of the study. All intervention group practices were provided direct access to LEO CAT for any of their referrals of suspected first-episode psychosis.
The control group practices did not receive any formal training sessions or leaflets apart from standard health information circulars. They were encouraged to continue to refer new suspected cases of psychosis to the standard assessment and treatment teams. Once their assessment was completed, then first-episode cases (meeting the study criteria) were referred straight to LEO CAT for initial treatment and follow-up.
LEO CAT was available for new referrals from any source between 09.00 and 17.00 h weekdays. It provided rapid home-based assessment and engagement. If first presentation first-episode psychosis was confirmed, then LEO CAT provided initial home-based acute phase treatment before handing over to the LEO community team for follow-up. All patients had the same access to the LEO in-patient unit.
Assignment
For the purposes of the study there were two categories of patient: those in the intervention group (registered with intervention group GPs), and those in the control group (registered with control group GPs). Patients registered with other GPs or not registered with a GP were excluded from the study (although in practice they were offered the same service as the intervention group).
LEO CAT recorded and tracked details of all new referrals of suspected first-episode cases and data were entered on a Microsoft Access 2000 database. A leakage study was undertaken (by A.S.) to identify any cases that might have been missed.
The research workers (N.R., H.F. and M.R.) worked in collaboration with the clinical teams. They approached patients for consent and interview assessments after confirmation of meeting the LEO criteria and commencing treatment. The researchers were not masked to the assignment. The ratings were completed usually within a month of their first commencement on antipsychotic medication. For patients who did not consent to the study, anonymous clinical data were recorded as part of the LEO service clinical audit database.
Outcome measures
The outcome measures included GP practice rates of referral, and patients' duration of untreated psychosis (DUP), delays in the pathways to care, mental health service provision, and service engagement. Ratings of DUP, pathways to care, and service provision were operationalised using a new combined rating scale designed specifically for this study. This proved necessary as a pilot study identified problems with inconsistent definitions of DUP and the inability of pre-existing ratings to cross-reference components of DUP with steps in the pathway to care, and with services received (Reference Power, Russell and FisherPower et al, 2004). The new combined DUP, pathway to care, and service receipt measure relied on data gathered from structured interviews with three different sources (patient, carer and clinician) as well as medical files, thus allowing for a more detailed measure of DUP and delays in each step of the pathways to care.
For the purposes of this study two definitions of DUP were used. The first, traditional DUP, is defined as the time from first psychotic symptom (as opposed to psychosis) to the first contact with mental health services. The second, contemporary DUP, is defined as the time from the ‘transition to psychosis’ (unremitting psychotic symptoms for 1 week) to the commencement on antipsychotic medication (greater than 50% treatment adherence for a minimum of 1 month). Using the contemporary DUP will result in a significantly shorter duration than the traditional DUP when used in the same sample (Reference Power, Russell and FisherPower et al, 2004). The contemporary DUP definition/measure is the one referred to in the analysis below unless otherwise specified.
Delays in the ‘pathway to care’, i.e. steps 1–6 (see Fig. 1) occurring during the DUP were measured by calculating the number of days between the dates of the onset of the acute psychotic episode (transition to psychotic) and the start of the steps in the pathway to care. In a small number of cases one or more of these measures resulted in a negative value, e.g. if a patient had already begun to attend their GP for advice before their transition to psychosis. In these cases the negative values were converted to zero.
Statistical analysis
We predicted that 85% of patients with first-episode psychosis would be registered with a GP and that 80% of the eligible patients would consent to the study. A power calculation estimated that we needed to recruit 175 patients into the study in order to reliably identify a significant difference between the intervention and control group based on a 25% reduction in the mean log DUP or other measures of delay.
Data were analysed using the Statistical Package for the Social Sciences (SPSS) version 13.0 for Windows. Group differences were analysed by χ2 or t-tests. Given the skewed distribution of DUP and delay data, measures were converted into a log value by a formula, e.g. log(DUP+1). P values equal to or lower than 0.05 were considered statistically significant.
RESULTS
During the 27-month study period, 394 patients with suspected first-episode psychosis were referred to Lambeth's mental health services (see Fig. 2) for assessment. There were 334 patients (84.7%) who had GPs (44.3% intervention group GPs; 41% control group GPs; 11.9% non-Lambeth GPs; and 2.4% non-trial Lambeth GPs); 40 patients (10.1%) had no GP and another 21 patients (5.3%) could not confirm registration with a GP.
Out of all referrals (n=394) 22 failed to engage before a clinical assessment could be completed and 17 were still being assessed (by the time the study finished. For the remaining 355 referrals that were clinically assessed, 73 were found not to be psychotic. Of the remaining 282 who presented as psychotic, 85 did not meet the study criteria (29 who lived outside Lambeth or were homeless, 5 over 35 years of age, 1 with severe learning disability, 28 on antipsychotic treatment for more than one month, and 22 in contact with mental health services for more than 6 months). The remaining 197 patients met the study criteria and were therefore eligible for the LEO service.
There were 152 of the 197 eligible patients who consented to the research interviews, with 2 dropping out, leaving 150 patients (76%) whose research interviews were completed. Of the other 45 patients: (a) 24 proved too difficult for the research worker to approach (4 quickly moved overseas, 10 disengaged from the service, and 10 could not be approached until after the initial window period of ratings had expired), (b) 21 were formally approached by the research worker but 14 formally refused to consent to the research ratings, 6 failed to attend subsequent interviews, and 1 was deemed unable to give informed consent.
Of the consenting 150 patients, 113 (75.3%) patients were registered with GPs in either the intervention (n=50) or control (n=63) practices. A further 21 (14%) patients were registered with non-trial practices (outside Lambeth or non-consenting Lambeth practices) and 16 (10.7%) patients had no GP.
For the purposes of the rest of the analysis patients not registered with intervention and control GPs (i.e. trial GPs) were excluded. There was no difference between the demographic characteristics of these excluded patients and the patients registered with trial (treatment or control) GPs. Nor was there a difference in the mean DUP between patients registered with trial and non-trial GPs. The excluded group of patients with no GP (n=16) appeared to have a longer mean DUP (mean DUP = 98.4 weeks, s.d.=230) than the patients registered with trial GPs (n=113) (mean DUP = 50.2 weeks, s.d.=147.7), but the difference was not statistically significant.

Fig. 2 Recruitment into the LEO CATstudy.
1. represents the proportion of patients not registered with treatment or control GPs.
Intervention and control GP patients
Patient characteristics
Of the 113 patients, 81 (71.7%) were males; the mean age was 23.92 years (s.d.=5.27). The ethnic origins were 26% Black African, 26% Black Caribbean, 7% Black British, 18% White British, 11% White non-British, 9% Asian, and 4% mixed. Thirty-five percent were born overseas (44% in Africa, 10% in the Caribbean, 26% in Europe, 7.6% in East Asia, 5% Middle East, and 7.6% in the Americas); mean age of migration was 16.5 years (s.d.=7.8). Eighty-eight per cent were single and 20% were living alone; 26% currently had a partner/spouse; 29% had children. Seventy-three per cent had been educated beyond the age of 16 and 8.8% were still students. Seventy-eight per cent had been employed in the past but only 14% were still employed. Thirty per cent had a history of criminal convictions and 48 (42.5%) reported being victims of crime. There was no difference in these characteristics between the two samples.
DUP
The mean ‘traditional DUP’ was 101 weeks (s.d.=204.4); median ‘traditional DUP’ was 21.7 weeks, with a range of zero to 24 years; mean ‘contemporary DUP’ was 50.2 weeks (s.d = 147.7); median ‘contemporary DUP’ was 10.1 weeks, with a range of zero to 24 years. Two of the intervention group and 2 control group patients had to be excluded as they never commenced antipsychotic treatment. Using the ‘Contemporary DUP’ as a definition of DUP rather than the ‘traditional DUP’ resulted in a significantly shorter mean DUP measure.
Delays in pathways to care
Seven patients (2 intervention & 5 control) were first seen by mental health services during their prodrome phase (mean duration of prodrome for all patients was 105.1 weeks, median 30.7 weeks, s.d.= 186.8, range 1–974 weeks). A further 13 patients had made contact during their prodrome with a health agency and 4 other patients with non-health services. The rest were first seen by services either at or after their transition to psychosis. Patients first attended any agency (health or non-health professional) on average 36.6 weeks after the transition to psychosis (median 18.9 weeks, s.d.=204.5, range 0–1293 weeks), with a further delay of 4.5 weeks on average (median 2.25 weeks, s.d.=24, range 0–163.7 weeks) before contact specifically with a health agency.
Patients seen by GPs
Seventy-one (62.8%) patients were seen by GPs during the DUP period. GPs first saw these patients on average 29.2 weeks after their transition to psychosis (median 3.1 weeks, s.d.=80.8). In the majority of cases (79%), patients had referred themselves to their GP. As a group, those who attended their GP did not experience a shorter DUP than those who did not.
Approximately the same proportion of intervention and control group patients attended their GP (36/50 and 35/63 respectively) during their DUP period. There was no significant difference in the mean DUP between intervention and control groups. Neither was there a significant difference between the groups in the mean delay from ‘transition’ to their first contact with a GP. The mean delay patients experienced from the time they were first seen by the GP to the first assessment by mental health services was 26.3 days (median 14 days, s.d.=39.6) for the intervention GP patients and 92.3 days (median 22 days, s.d.= 222.8) for the control GP patients. Similarly, the delay between first seen by GP and starting antipsychotic medication was 51.1 days (median =36 days, s.d.= 74.1) for intervention GP patients and 111.0 days (median 37 days, s.d.=227.2 days) for control GP patients. There was no significant difference in the means when these measures were converted to their log format. However, significantly fewer of the intervention group experienced long delays (over 6 weeks) between first contact with GP and being assessed by mental health services (13.9% intervention GP patients v. 37.1% control GP patients, χ2=3.92, d.f.=1, P<0.05). Similarly, fewer experienced delays of greater than 3 months in starting antipsychotic medication after first seeing the GP (5.9% intervention GP patients v. 27.3% control GP patients, χ2=4.13, d.f.=1, P<0.05).
Patients seen and referred by GPs directly to mental health services
GPs referred 54 patients (76.1% of those seen by GPs) directly to mental health services. Intervention group GPs were significantly more likely to refer their patients (31/36, 86.1%) than control group GPs (23/35, 65.7%) (χ2=4.1, d.f.=1, P<0.05).
There was no difference in the mean DUP (or the mean log[DUP +1]) between the intervention and control GP referred samples (intervention group mean DUP= 239.9 days, s.d.=537; control group mean DUP=245.3 days, s.d.=526.9). Nor was there a significant difference in the mean delay from ‘transition’ to first contact with GP, i.e. Steps 1–3 (see Fig. 1).
Intervention group GPs referred their patients to mental health services (see Step 4, Fig. 1) on average 12.2 days (median 1 day, s.d. = 30.6) after they were first seen, whereas control group GPs referred their patients on average after 78.1 days (median 6 days, s.d=242.1 days). Similarly, intervention GP patients were assessed by mental health services (including LEO CAT) (see Step 5, Fig. 1) on average 14.0 days (median 7 days, s.d.=26.8 days) after the GP referral, whereas control GP patients were seen on average 31.2 days (median 7 days, s.d.=53.5 days) after referral. There was no significant difference found in the means when these delays were converted to their log format. Intervention GP patients started medication on average 53.1 days (median 36 days, s.d.= 79.5) after first seeing their GPs, whereas for control GP patients this was after 114.1 days (median 37 days, s.d. = 264.1). Again, there was no significant difference in the means when these measures were converted to their log format.
Proportion of DUP affected by health service delays in the pathway to care
The relevant proportions of DUP affected by the health service delays (see Steps 4, 5 and 6 in Fig. 1) are represented in Fig. 3 for patients who were seen by their GPs. For Steps 4, 5 and 6, each step's percentage of DUP was calculated for every case. Their mean percentage of DUP is displayed in Figure 3.
Health service delays (i.e. Steps 4–6: from first seen by GP to starting antipsychotic medication) on average accounted for 57% of the DUP in the control GP group and 45.6% of the DUP in the treatment group. Steps 4 and 5 (from first seen by GP to first assessed by mental health services) combined percentage of DUP was significantly lower in the intervention GP patients than in the control GP patients (mean percentage 20.9% for treatment group v. 37% for control group, P=0.02). There was no difference in the mean percentages of Step 6 (both groups were usually started on treatment by LEO CAT).
Use of accident and emergency departments and in-patient services
Significantly more of the control group, i.e. 30 (47.6%), were eventually referred to mental health services by accident and emergency departments or emergency medical services, whereas this was the case for only 6 (12%) of the treatment group (P<0.05). Four control group GPs referred patients directly to accident and emergency departments and 2 initiated mental health act assessments, whereas none of the treatment group GPs did this.
In total 58 (51.3%) of patients were hospitalised (46% of intervention group v. 55.6% of the control group) during the initial weeks of contact with mental health services. Patients who saw their GP during the DUP were less likely to be hospitalised (35.2%) than those who were not seen (78.6%) (P<0.001). Similarly, only 5 (31.3%) of the 16 patients referred directly to LEO CAT by Intervention Group GPs and none of the 8 patients seen initially by OASIS were hospitalised.
DISCUSSION
This is one of the few studies in first-episode psychosis to determine whether (a) educating GPs improves detection and referral to mental health services (see Step 4, Fig. 1) and (b) providing a specialist early detection and treatment team then speeds up the initial assessment by mental health services (Step 5) and commencement of treatment (Step 6). The results of this study suggest positive effects in these steps, despite the fact that the study was underpowered. GPs with training in early detection referred a greater proportion of their first-episode cases, and less of their patients experienced lengthy delays in initial assessment and treatment by the early detection team. For the untrained GPs with standard mental health services, the health service delays accumulated to 3 months on average and represented over half of the DUP.
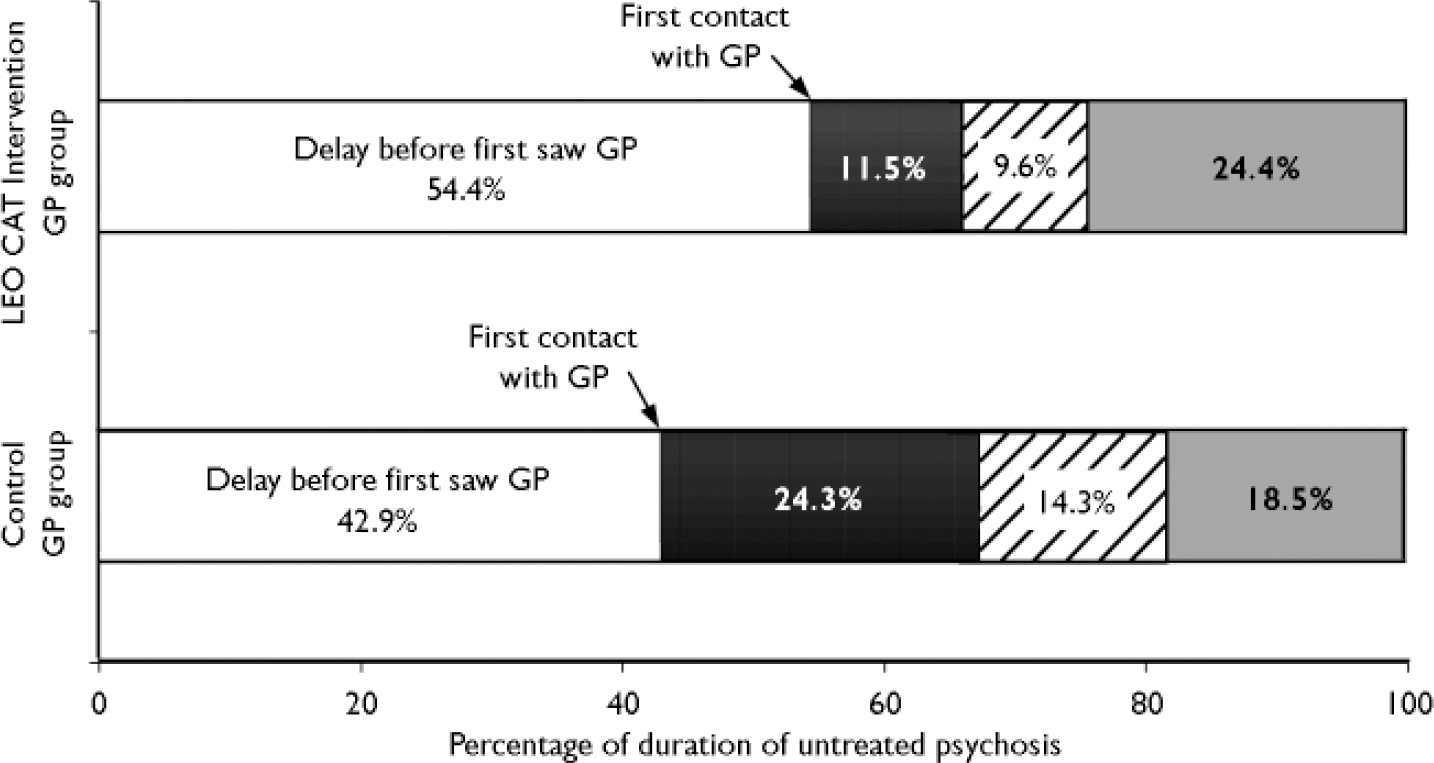
Fig. 3 Delays in the pathway from GP to treatment as a proportion of the
overall duration of untreated psychosis (DUP). Patients seen during
DUP by GPs (n=71). □, Steps 1–3: delay before first
saw GP; ▪, Step 4: delay in GP referral; ![]() , Step 5: delay in mental health service
assessment; ░, Step 6: delay in starting medication.
, Step 5: delay in mental health service
assessment; ░, Step 6: delay in starting medication.
However, the overall length of patients' DUP was relatively unaffected by our intervention. This is because most of the DUP occurs before the first contact with primary care services and would thus be largely unaffected by any GP interventions. The DUP in our patient samples is very similar to that seen in the control areas (Ulleval, Norway and Roskilde, Denmark) of the TIPS study (Reference Larsen, McGlashan and JohannessenLarsen et al, 2001). The reductions in DUP reported with the TIPS intervention may well reflect the impact of broader community education programmes on earlier steps in the DUP pathway. By rolling our intervention out to a broader referral base we may see a similar reduction in the earlier steps in the pathway and thereby an overall reduction in DUP. However, such broad interventions might increase demands on any early detection team, with a large expansion in the proportion of inappropriate referrals or cases at high risk of psychosis. In the TIPS intervention, only one appropriate first-episode patient resulted from 8 referrals (Reference Johannessen, Larsen and JoaJohannessen et al, 2005). In our limited intervention targeting just GPs, there was no obvious increase in demands on mental health services. The rate of inappropriate referrals remained low and the same for both samples (50% of all referrals). It is possible that our intervention does prompt GPs to refer patients with an inherently more insidious onset of psychosis (as Fig. 3 appears to suggest) but this was not confirmed in the analysis.
GPs clearly provide a vital role in the pathways to care in psychosis. Sixty-three per cent of our patients with first-episode psychosis sought help (usually on their own initiative) from their GP before being referred to mental health services. Patients referred by GPs were less likely to be hospitalised and patients from practices with the study intervention were less likely to require emergency services. Even if GPs did refer a proportion of patients with no psychosis, a sizeable proportion of these were identified as being at ultra-high risk of psychosis. These patients are likely to benefit from mental health services in their own right (e.g. OASIS) to reduce their risk of developing psychosis (Reference Broome, Woolley and JohnsBroome et al, 2005).
The GP education programme was very brief and simple. It facilitated very constructive dialogues between the LEO CAT staff and GP practice staff. None the less, it did prove difficult and time consuming to organise at each practice (a requirement of the randomisation). It would have been more efficient to have provided larger training seminars to groups of practices, for example with the support of the College of General Practitioners. This could also have attracted accreditation for professional development points with funding through normal channels. In hindsight, this training may be best provided by a combination of an external academic with one of the early detection team clinicians to avoid any conflicts of interest between the imperatives of the trainer and the early detection team, for example if the team is busy it is likely to suspend the training component to avoid increasing referrals. Whichever format is used it would be essential to repeat the training on a regular basis, particularly in inner city areas where primary care staff turnover is high.
The LEO CAT team is now co-located with the OASIS team and both teams combine their early detection training into one programme for all referring agencies (e.g. schools and colleges). The plan is to recruit this next cohort of patients into a further study of DUP pathways to see if this broader early detection strategy brings with it the benefits seen in the TIPS programme and improves the detection of patients at earlier phases of psychosis.
Finally, an 18-month follow-up study of the LEO CAT trial cohort is near completion. One of its aims is to determine whether the early detection strategy and reduction in delays seen in this study are associated with better outcomes and overall service usage.
Conclusions
Brief GP education and the provision of a specialist early detection team appears to improve GP referral rates and reduce long delays in the later steps of the pathways to care for young people with first-episode psychosis. However, it does not impact significantly on the overall DUP. Providing GP education in early detection does not increase demand on mental health services rather it is associated with less use of emergency services. A more effective strategy to reduce the overall DUP may be to combine it with a broader public health education campaign and thereby also impact on the earlier steps in the pathways to care.
Acknowledgements
We are very grateful to the Guy's and St. Thomas' Charity, which funded the LEO CAT team and its study for the first 2 years. Special thanks to members of the LEO CAT team, the LEO Research Co-ordination Group, Abdi Sanati, the Primary Care Research Management Group, Lambeth GPs, the South London and Maudsley NHS Trust and Lambeth Primary Care Trust for their support and help with this study.






eLetters
No eLetters have been published for this article.