Long-term follow-up studies of juvenile depression have emphasised the increased risk of adult major depression (Reference Harrington, Fudge and RutterHarrington et al, 1990; Reference Rao, Ryan and BirmaherRao et al, 1995; Reference Pine, Cohen and GurleyPine et al, 1998; Reference Weissman, Wolk and GoldsteinWeissman et al, 1999; Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue). This study specifically investigated the impact of comorbid conduct disorder on psychiatric outcomes in adult life following an index episode of major depression in childhood or adolescence. In the first report (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue), we found that relapse rates for adult major depression were high and unaffected by comorbidity status. However, significantly increased rates of alcoholism, drug misuse and dependence, and antisocial personality were found in the comorbid group. This study examines other adult outcomes with respect to suicidality over the life span, adult social adjustment, social and personality dysfunction, and criminality in the long term. The hypothesis was that youths with depression and comorbid conduct disorder would have worse adult outcomes than their counterparts with depression but without conduct disorder.
METHOD
Participants
Details of the participant selection process are provided elsewhere (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue). In brief, 245 patients who attended the Maudsley Hospital in London between 1970 and 1983 were selected as they met DSM-IV criteria (American Psychiatric Association, 1994) for major depressive disorder (MDD) either with (n=97) or without (n=148) conduct disorder. These individuals were traced for follow-up interview. Eight had died during the follow-up interval and 48 could not be traced despite repeated attempts. Of the remaining 189 subjects, 40 either refused to be interviewed or repeatedly defaulted on appointments made by interviewers. The remaining 149 individuals were successfully interviewed. No association was found between interview status and baseline clinical features within each diagnostic group. Data collection procedures have been reported earlier (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue).
Measures
Childhood measures
Maudsley item sheet database. Clinical data have been recorded over time in the Maudsley item sheet database. Scale scores were constructed to assess specific dimensions of psychopathology at presentation. The suicidality item ‘suicidal ideas, attempt or threat’ was also used to describe patient status at referral (see Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue, Table 2).
Table 1 Sample characteristics at follow-up (n=149)
| MDD (n=96) | CD-MDD (n=53) | P | |
|---|---|---|---|
| Age (years), mean (s.d.) | 34.7 (4.1) | 34.4 (4.0) | 0.65 |
| Follow-up interval (years), mean (s.d.) | 20.9 (3.9) | 20.3 (3.8) | 0.38 |
| Marital status | |||
| Married/cohabiting | 54 (56.3) | 18 (34.0)[UNK] | |
| Single | 30 (31.2) | 26 (49.0)[UNK] | 0.032 |
| Divorced/separated/widowed | 12 (12.5) | 9 (17.0)[UNK] | |
| Ethnic group | |||
| White | 83 (86.5) | 42 (79.2)[UNK] | |
| UK Black | 10 (10.4) | 9 (17.0)[UNK] | 0.49 |
| Other | 3 (3.1) | 2 (3.8)[UNK] | |
| Educational level1 | |||
| None | 38 (39.6) | 31 (59.6)[UNK] | |
| CSE | 12 (12.5) | 8 (17.3)[UNK] | |
| O levels | 24 (25.0) | 9 (15.4)[UNK] | 0.037 |
| A levels or more | 22 (22.9) | 4 (7.7)[UNK] | |
| Social class | |||
| I, II | 31 (32.3) | 8 (15.1)[UNK] | |
| III non-manual | 21 (21.9) | 6 (11.3)[UNK] | |
| III manual | 7 (7.3) | 4 (7.6)[UNK] | 0.017 |
| IV, V | 8 (8.3) | 5 (9.4)[UNK] | |
| Not employed | 29 (30.2) | 30 (56.6)[UNK] | |
| Housing tenure (% owners) | 51 (53.1) | 14 (26.4) | 0.002 |
| Employment | |||
| Full-time | 55 (57.3) | 18 (34.0)[UNK] | |
| Part-time | 11 (11.5) | 5 (9.4)[UNK] | 0.009 |
| Unemployed | 30 (31.2) | 30 (56.6)[UNK] | |
| Income (weekly)1 | |||
| £ 0-175 | 20 (23.5) | 23 (47.9)[UNK] | |
| £ 176-450 | 31 (36.5) | 13 (27.1)[UNK] | 0.015 |
| >£ 450 | 34 (40.0) | 12 (25.0)[UNK] |
Table 2 Suicide attempts in childhood and adult life
| MDD | CD-MDD | Odds ratio1 | 95% CI | |
|---|---|---|---|---|
| (n=96) (%) | (n=53) (%) | |||
| Suicide attempt in the course of index | ||||
| episode | 22.9 | 56.6 | 5.0 | 2.3-10.6 |
| Suicide attempt after age 17 years (SADS-L) | 14.6 | 35.9 | 3.7 | 1.6-8.5 |
| Lifetime history of suicide attempts | 32.3 | 66.0 | 4.9 | 2.3-10.4 |
Ratings of medical notes. All medical, social, educational and psychological data concerning the participants were extracted on an ad hoc questionnaire. As neither the item sheet measure of suicidality nor the relevant DSM-IV diagnostic criterion for MDD differentiated suicidal cognitions or threats from actual suicidal attempts, a separate rating of suicide attempt was made allowing such distinction. For this rating, any occurrence of suicidal attempt either before initial presentation, at initial assessment or during the later course of the index episode counted towards a positive rating. This rating is used hereafter as an index of childhood suicidality.
Adult follow-up measures
Schedule for Affective Disorders and Schizophrenia-Lifetime version. Lifetime rates of specific psychiatric disorders were measured with a revised semi-structured version of the Schedule for Affective Disorders and Schizophrenia-Lifetime version (SADS-L; Reference Harrington, Hill and RutterHarrington et al, 1988). To maintain blindness during the assessment, all interviews started with the SADS-L focusing on life after the respondent's 17th birthday. The SADS-L included a question on the occurrence of suicide attempts since age 17 years, which is used subsequently as an index of suicidality in adult life.
Adult Personality Functioning Assessment. The Adult Personality Functioning Assessment (APFA) is an investigator-based interview devised to assess dysfunction in six key domains of adult life: work, love relationships, friendships, non-intimate social contacts, negotiations and everyday coping (Reference Hill, Harrington and FudgeHill et al, 1989). Ratings were made for a baseline period (age 21-30 years) and when applicable (i.e. for subjects aged over 30 years) for the ‘current’ (preceding 5 years) period. Each domain was scored on a sixpoint scale ranging from 0 (unusually effective, substantially above average) to 5 (failure of role performance). A rating for each domain was reached in reference to explicit coding procedures and to a dictionary. Ratings from 0 to 2 are within the normal range, a 0 rating signalling particularly good functioning and a 2 rating indicating some difficulties on a background of generally satisfactory functioning. Ratings of 3 or more are indicative of dysfunction and major problems, with higher scores indicating more serious and pervasive dysfunction. For each domain, the principal type of dysfunction (discordance/aggression v. avoidance/apathy) was noted. The APFA was administered after the SADS-L interview in order to identify any period of the respondent's life where functioning might have been altered by psychiatric symptoms or disorders. When applicable, these periods were noted and ratings were focused on periods free from frank psychiatric disorder. The scores for the six domains were combined into a total score, a score of 16 or greater indicating generalised dysfunction. Further details on the development and properties of the APFA can be found elsewhere (Hill et al, Reference Hill, Harrington and Fudge1989, Reference Hill, Fudge and Harrington1995). The subject version of the APFA was used except in a few cases when interviews were carried out with relatives using the informant version. After each interview a detailed vignette was written, which was independently rated by the first author and the interviewers, blind to the original childhood diagnosis and to other followup data. Discrepancies were resolved through discussion and consensus. Rating meetings were organised throughout the period of collection of data to minimise interviewer ‘drift’ in the administration and rating of the schedule.
Criminal and death records. Criminal records were accessed from the Central Criminal Records Office at the Home Office in London. As data on court appearances are usually several months in arrears, criminal history data on the participants were updated at the end of the study. Criminal history was coded with the standard list of offences of the Offenders Index. For these analyses, minor offences (police cautions and minor crimes such as traffic offences) and convictions before the 17th birthday were excluded. Death records were obtained on eight individuals who had died during the follow-up interval.
Interrater reliability
Excellent reliability was obtained for SADS-L ratings of adult suicide attempts (κ=0.94). Reliability for other psychiatric outcomes has already been reported (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue). Interrater reliability for APFA ratings was very good for five domains (work, 0.904; love relationships, 0.858; friendships, 0.871; non-intimate social contacts, 0.842; negotiations, 0.813) and good for the sixth domain (everyday coping, 0.729). Consistent with published data on the reliability of APFA scores (Reference Hill, Harrington and FudgeHill et al, 1989), the intraclass correlation coefficient (ICC) for the APFA total score was excellent (0.920). When scores were dichotomised according to the published threshold of 16, interrater agreement on the presence or absence of severe social dysfunction was very good (κ=0.79).
Statistical analyses
Univariate comparisons were performed with the χ2, Fisher's exact and Student's t tests. Interrater reliability was assessed with Cohen's κ coefficient for categorical measures, and with the intraclass correlation coefficient for scale scores (Reference Bartko and CarpenterBartko & Carpenter, 1976). The effect of comorbid conduct disorder on adult outcomes was assessed with logistic regression models, controlling for age and gender. The effect of comorbidity on APFA scores was analysed by a multivariate analysis of variance (MANOVA), followed by separate two-way (childhood diagnosis × gender) ANOVAs in order to limit the impact of missing data on statistical power. To adjust for unequal observation times, Cox proportional hazards models were fitted to criminal data, and relative risks of adult offences according to childhood comorbidity status were estimated. Survival functions were calculated with the Kaplan-Meier estimator, with age of onset at the first conviction as the dependent event. Subjects free of any conviction during their adult years were right-censored. Differences between survival functions were examined with the log-rank test. Throughout, a conventional P value of 0.05 was retained as the level of statistical significance.
RESULTS
Adult social adjustment
The main socio-demographic characteristics of the sample at follow-up interview are summarised in Table 1. On most indicators of social adaptation and adjustment, the CD-MDD group fared much worse than the MDD group, particularly regarding employment and income. Social class differences were entirely accounted for by the nearly two-fold increase in the proportion of participants not employed at follow-up in the CD-MDD group.
Completed suicide and lifetime suicide attempts
Of the 245 persons included in the study, 8 (5 men) had died by the time they were traced at follow-up. Of these, 6 deaths (4 men, 2 women) were probably suicide (mean age at death 24.4 years, range 16-35 years). Two subjects were patients at a different psychiatric hospital at the time of their death. Death certificates indicated the following causes of death: overdose with tricyclic antidepressants (n=2), hanging (n=1), multiple injuries, with one subject being struck by a train (n=2), and injection of a mixture of heroin and diazepam (n=1). Two death certificates clearly mentioned that the subject had taken his own life; the verdicts returned by the coroners were suicide (n=1), accidental death (n=2) and open verdict (n=3). The cumulative risk of suicide in this sample was 2.45% (6/245; 95% confidence interval 1.0-5.0%). Taking into account the length of the observation period for each individual, the annual suicide incidence rate in the whole sample was estimated at 120.2 per 100 000 (95% CI 48.7-250). Suicidal deaths were more characteristic of the CD-MDD group (5 out of 6). The annual incidence rate was much higher in the CD-MDD group (261.4 per 100 000) compared with the MDD group (32.5 per 100 000), a difference which was significant (incidence rate ratio 8.05, 95% CI 1.11-191.5, P=0.037). As expected, suicidal deaths were also more frequent in males (annual incidence rate 174.8 per 100 000, 95% CI 55.5-421.6) than in females (annual incidence rate 74.0 per 100 000, 95% CI 12.4-244.5) with a rate ratio of 2.36 (95% CI 0.4-18.4, NS).
Table 2 presents rates of suicide attempt recorded during the depressive index episode in childhood and those reported at interview to have occurred during the follow-up period, together with a combined lifetime estimate. Over a third (34.9%) of the sample had made at least one attempt at the time of the index depressive episode, with a significantly higher rate in the CD-MDD group than in the MDD group. Suicide attempts through the follow-up period followed the same pattern, with 22.2% of subjects attempting suicide through follow-up and almost half the sample (44.3%) having made an attempt at least once in their life. The combined lifetime rates for suicide attempts testify to the long-term suicide risk carried over time by those with childhood and adolescent depression, and of the particular added vulnerability conveyed by comorbid conduct disorders. A robust gender effect was found for all three rates, with females being consistently at higher risk of suicide attempt (gender effect for lifetime history of suicide attempt: OR=3.7, 95% CI 1.7-8.0, P=0.001).
Adult social and personality dysfunction
One person in the CD-MDD group refused to complete this section of the interview. Because of unequal ages, scores were missing for current functioning for participants younger than 33 years at follow-up, for whom there are only baseline scores. Accordingly, analyses relied on baseline scores. Where scores for both periods were available, very high correlations were found between the baseline score (age 21-30 years) and the current scores within each of the six domains (work, 0.72; relationships, 0.68; friendships, 0.86; non-intimate contacts, 0.90; negotiations, 0.86; coping, 0.78), suggesting highly stable patterns of functioning in the 20— to 40-year age range. Thus, when baseline scores were missing (a relatively common occurrence for the work domain) but scores were available for the current period of functioning, we assigned the current value to replace the missing baseline score. In a few cases one domain score was still missing, and the average value of the other domain scores was input to that domain in order to calculate the total APFA score in a comparable fashion for all subjects.
The MANOVA with the six APFA domain scores as dependent variables showed a significant effect of childhood diagnosis (multivariate F statistic 2.77, d.f.=6,119, P=0.015). As subjects could not contribute to the multivariate test owing to some missing data in one domain (in particular the work domain), the effect of childhood diagnosis on both the total and the domain scores of the APFA was further examined in a series of two-way (childhood diagnosis × gender) ANOVAs (Table 3). For all six domains of social functioning, mean scores were significantly higher for the CD-MDD group than for the MDD group, this difference being greatest for the non-intimate social contacts domain. Half the mean scores of the CD-MDD group were in the dysfunctional range (3), whereas this was not the case for any domain for the MDD group. However, scores within the MDD group were the highest for the two domains involving interpersonal relationships (love relationships and friendships). The total score achieved a highly significant differentiation between the two adult groups; however, the mean total score in the MDD group was still elevated when compared with other adult control samples (Reference Hill, Harrington and FudgeHill et al, 1989), reflecting the clinical mode of case ascertainment. The APFA scores were remarkably parallel to those obtained in an earlier Maudsley investigation (Reference Harrington, Fudge and RutterHarrington et al, 1991). Using the published cut-off of 16, rates of pervasive social dysfunction were computed for each group (Table 3, last line). Again, the comorbid group showed a two-fold increase in social dysfunction when compared with the non-comorbid group (OR=3.15 adjusted on gender, 95% CI 1.5-6.4, P=0.002). Between-group differences are summarised in Fig. 1, which shows, separately for each diagnostic group, the proportion of subjects with no or up to six domains of social dysfunction (defined as a domain score of 3 or more). Again, groups differed significantly in the numbers of deviant domain scores (χ2=19.7, d.f.=6, P=0.003), with a pattern of multiple dysfunction being more characteristic of CD-MDD subjects. Over half (58.3%) of the MDD sample had two or fewer domains with social dysfunction, in comparison with only 28.8% of the CD-MDD group.
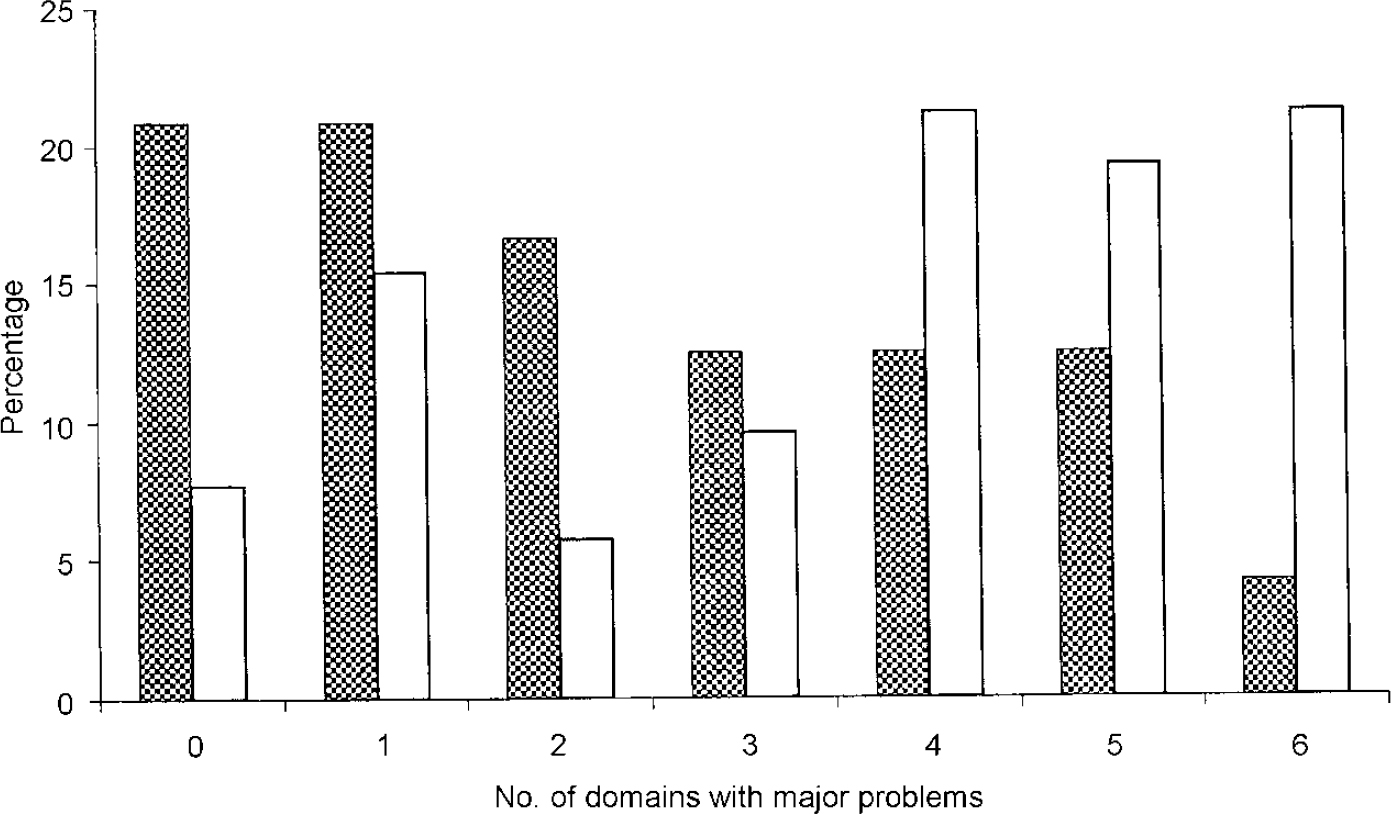
Fig. 1 Domains of social dysfunction in adult life for study groups with major depressive disorder, with (□) or without ([UNK]) conduct disorder.
Table 3 Social dysfunction in adult life: Adult Personality Functioning Assessment (APFA) scores
| MDD (n=96) | CD-MDD (n=52) | F 1 | P 1 | |||
|---|---|---|---|---|---|---|
| Mean | s.d. | Mean | s.d. | |||
| Work | 1.8 | (1.1) | 2.6 | (1.5) | 10.8 | 0.001 |
| Love relationships | 2.9 | (1.1) | 3.5 | (1.1) | 9.1 | 0.003 |
| Friendships | 2.4 | (1.3) | 3.0 | (1.3) | 7.3 | 0.008 |
| Non-intimate social contacts | 2.3 | (1.1) | 3.1 | (1.2) | 16.2 | 0.001 |
| Negotiations | 2.2 | (0.9) | 2.9 | (1.2) | 13.8 | 0.001 |
| Everyday coping | 2.0 | (1.0) | 2.5 | (1.3) | 7.2 | 0.008 |
| Total APFA score | 13.9 | (4.6) | 17.8 | (6.1) | 21.1 | 0.001 |
| Percentage above cut-off score of 16 | 37.5 | 65.4 | 0.0022 | |||
With the exception of the work and love relationships domains, gender effects were significant in the ANOVAs for the remaining four domains and the total scores of the APFA; all differences reflected higher scores in men than in women.
Criminal records
Consistent with their high rates of anti-social personality disorders, subjects in the CD-MDD group had significantly higher conviction rates in adult life for all types of offences, compared with the MDD group (39.6% v. 15.6%; χ2=10.7, d.f.=1, P<0.001). The proportional hazard models confirmed the raised risk of criminality in the CD-MDD group (relative risk adjusted on gender 2.9, 95% CI 1.5-5.6); risk was significantly higher for men than for women (relative risk 3.5, 95% CI 1.7-7.0). Similarly, a significant difference was found between the two survival curves (log-rank test 12.05, d.f.=1, P=0.0005) (Fig. 2). The proportions of subjects who remained free of conviction through the follow-up interval were 81.7% in the MDD group and 60.1% in the CD-MDD group.
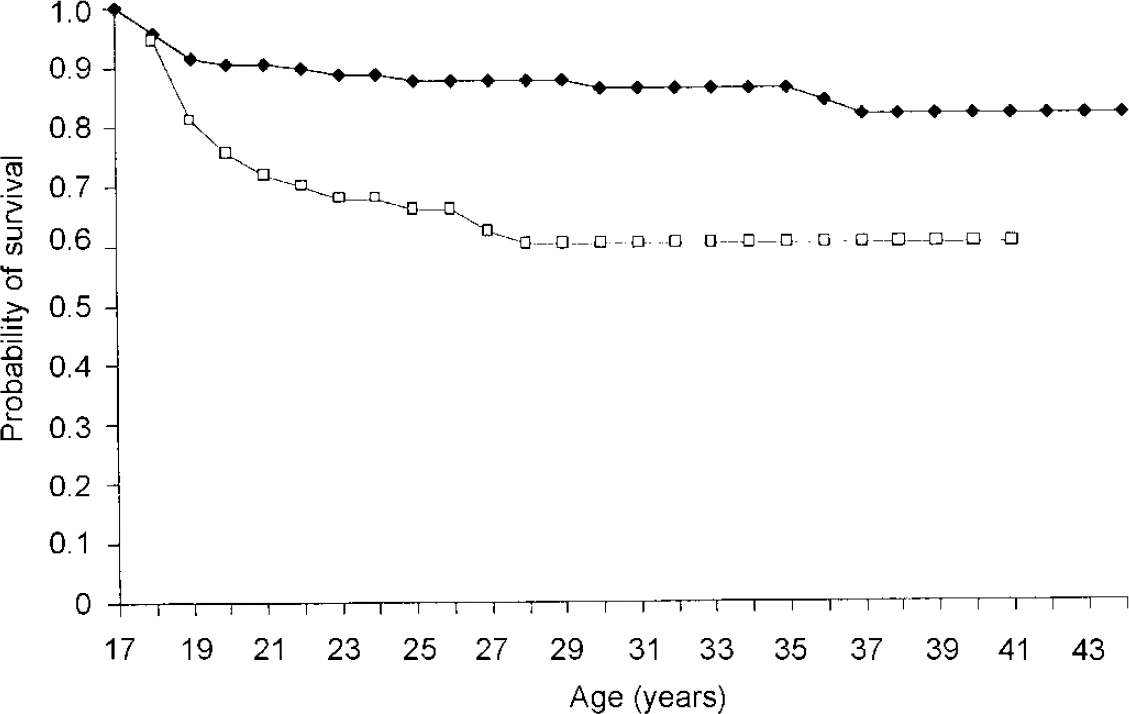
Fig. 2 Survival from criminal offences (Kaplan-Meier estimation) for major depressive disorder subjects with (□) or without (♦) conduct disorder.
DISCUSSION
Completed suicide and suicide attempts
A high annual incidence of suicidal death during the follow-up period was found (120 per 100 000), representing roughly a six-fold increase of the averaged population rate over the study period for men and women of the same age group (Reference Charlton, Kelly and DunnellCharlton et al, 1992). Our cumulative rate of suicide (2.45%) is comparable to that (2.5%) derived from an earlier follow-up study conducted at the same site (Reference Harrington, Fudge and RutterHarrington et al, 1990). Other studies conducted in the USA have yielded slightly higher suicide risks for youths who had had depression, such as the 4.4% rate in a 10-year follow-up of 159 children and adolescents with MDD (Reference Rao, Weissman and MartinRao et al, 1993) or the 7.7% rate in an extended 10— to 15-year follow-up of the same sample but limited to adolescents (Reference Weissman, Wolk and GoldsteinWeissman et al, 1999). Differences between these two clinical samples are difficult to interpret. Perhaps it should be borne in mind that youth and young adult suicide rates have typically higher baseline values in the USA than in the UK, and that the youths in the two UK studies were in their teenage and young adult years two decades ago, at a time when the upward trend in suicide rates had not yet occurred. In contrast, US studies were conducted on younger subjects and some time after the secular increase in suicide rates which occurred in the late 1950s in the USA. At any rate, all the studies concur in indicating a strong increase in risk of suicidal death associated with child and adolescent depression, a risk which extends much beyond the teenage years.
As in most other studies of youths with depression assessed in clinical settings (Reference Garber, Kriss and KochGarber et al, 1988; Reference Myers, McCauley and CalderonMyers et al, 1991; Reference Kovacs, Goldston and GatsonisKovacs et al, 1993), rates of suicide attempts were very high during the index depressive episode. Suicide attempts were also a feature observed throughout adult life, with nearly half the sample having made a suicide attempt during their lifetime. At each measurement point, however, rates of suicidal behaviours (deaths and attempts) were much higher in the CD-MDD group, a result consistent with psychological autopsy studies which show risk associations with both depression and disruptive disorders (Reference Shaffer, Gould and FisherShaffer et al, 1996), and with other follow-up studies of clinical samples of youths with depression (Reference Kovacs, Goldston and GatsonisKovacs et al, 1993). As no conduct-disorder group without depression was available in this study, the specific effect of comorbid depression on rates of suicidal behaviours in conduct-disorder groups cannot be directly estimated. These findings on increased rates of suicidal behaviours through follow-up in the subjects with comorbid depression are somewhat at variance with those of the previous Maudsley follow-up study (Reference Harrington, Bredenkamp and GroothuesHarrington et al, 1994), although the power to detect such an association was greatly reduced in this earlier investigation.
Social adjustment
Compared with the MDD group, the overall outcome appeared worse in the CD-MDD group for a range of social, personal and familial indicators. Thus, the CD-MDD group reported higher levels of unemployment, lower income, less frequent housing tenure and lower rates of cohabitation compared with the MDD group. This long-term relationship between childhood diagnosis and adult social adjustment is striking, bearing in mind the considerable length of the follow-up interval. The lower social class status observed at follow-up in the comorbid group must be calibrated against the lack of social class differences at initial presentation between both groups (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue). Thus, the social drift observed through the 20-year follow-up interval is likely to be a direct consequence of childhood psychopathology and, more specifically, of conduct disorder. A health economics analysis is under way to explore these differences further.
Social dysfunction and criminality
On a standardised measure of social dysfunction, both groups had scores indicative of substantial social dysfunction. For the MDD group, social dysfunction tended to concentrate in a few domains, particularly those involving interpersonal relationships, with the majority having fewer than three dysfunctional domains. Similar specific areas of social dysfunction among adults with recurrent depression have been reported by other investigators (Reference Garber, Kriss and KochGarber et al, 1988; Reference Harrington, Fudge and RutterHarrington et al, 1991; Reference Rao, Ryan and BirmaherRao et al, 1995; Reference Weissman, Wolk and GoldsteinWeissman et al, 1999). In contrast, the CD-MDD group had both higher levels and more pervasive types of social dysfunction than the MDD group, and about two-thirds scored in the clinical range of the standardised measure. This figure must be compared with the rate of 45% reported in this group for adult anti-social personality disorder (Reference Fombonne, Wostear and CooperFombonne et al, 2001, this issue). Thus, it appears that adult dysfunction is underestimated when outcome is narrowly defined with diagnostic categories and that dysfunctional social outcomes are very common following conduct disorder. In addition, the rates of both antisocial personality disorder and of more global dysfunction are similar to those reported in follow-up studies of youths with conduct disorder but without comorbid depression (Reference Zoccolillo, Pickles and QuintonZoccolillo et al, 1992). Thus, it appears that comorbid depression exerted no attenuating influence on the outcome of conduct disorder in our sample; and negative psychiatric outcomes, such as the high rate of depressive relapse and the very high rates of suicidality in this group point towards the addition of negative effects in adult life of both comorbid childhood conditions.
The design of this study is inadequate to test the potential impact of the therapeutic measures used at the time of Maudsley attendance on long-term outcomes of adolescent depression. What the data undoubtedly show, however, is the longterm elevation of risk for a range of detrimental adult psychopathological and social outcomes in this sample of youths with depression. Evidence-based intervention strategies have now become available, including both pharmacotherapy (Reference Emslie, Rush and WeinbergEmslie et al, 1997) and time-limited psychotherapies (Reference Harrington, Whittaker and ShoebridgeHarrington et al, 1998; Reference Mufson, Weissman and MoreauMufson et al, 1999), which appear to improve short-term outcomes in adolescent depression. The challenge now is to devise and test the efficacy of interventions to reduce the high relapse risk carried forward into adult life. Considering the multiplicity of negative outcomes, interventions likely to achieve that goal should incorporate components addressing not only depressive symptomatology per se but also comorbid disorders and broader issues of social functioning. Suicide prevention programmes should also aim at targeting youths with depression, particularly those with comorbid disruptive disorders, as they appear to have a heightened risk of suicide morbidity and mortality.
Clinical Implications and Limitations
CLINICAL IMPLICATIONS
-
• Adolescent depression is associated with long-term maladjustment and interpersonal problems.
-
• Depression occurring with conduct disorder is associated with worse social outcomes than depression alone.
-
• Adolescents with depression and conduct problems should be targeted for suicide prevention.
LIMITATIONS
-
• Comparison groups with either conduct disorder only or non-affective psychiatric disorders were not available.
-
• Initial psychiatric assessments were based on medical notes.
-
• The impact of early psychiatric interventions could not be evaluated.
Acknowledgements
The authors thank Olive McKeown, Theresa Pearce, Karen Schepman, Debbie Heavey, Val Hicks and Felicity Whitton for their contribution to the study.








eLetters
No eLetters have been published for this article.