To the Editor:
We read with great interest the recent paper in your journal regarding the potential interest in pharmacogenetic testing for the guidance of psychiatric treatment.Reference Espadaler, Tuson, Lopez-Ibor, Lopez-Ibor and Lopez-Ibor1 It was the second articleReference Pérez, Salavert and Espadaler2 on this topic within a month, coming from the same country, confirming for us how useful pharmacogenetic testing can be in our daily practice. Reading these articles reminded us of a third, where we had the pleasure to revisit the process of clinical equipoise,Reference Stahl3 something that we believe should be an essential part of the modern model of psychiatric practice for treatment resistance.
We have been using the Portuguese version of Neuropharmagen® at our treatment-resistant schizophrenia outpatient clinic at the Hospital Júlio de Matos for a couple of years and would like to present herein a case report of successful treatment with this promising tool.
A 42-year-old man living as a homeless person for three decades was admitted for extreme self-neglect and aggressive behavior secondary to refractory persecutory delusional ideation. In his extensive clinical records, we found 85 psychiatric admissions over the last 25 years! We easily found enough information compatible with various episodes of both nonaffective and affective psychotic episodes (some manic, others depressive), suggesting a diagnosis of schizoaffective disorder. Nevertheless, the most disturbing aspect of this patient’s life was his complete selfish, hedonistic, irresponsible, drifting, and aimless lifestyle, along with a complete lack of hold on life or on his self. His life history led us to study the fascinating concept of Bleuler’s haltlose personality disorder,Reference Langmaack4 which came naturally as a comorbid diagnosis, based on some of the features now explained (Table 1).
Table 1 Haltlose personality disorder (adapted from Langmaack 2000)
The patient had been on many different combinations of benzodiazepines, antidepressants, mood stabilizers, and antipsychotics, aside from various attempts with psychotherapy, group therapy, occupational therapy, and electroconvulsive treatment. Full recovery was never achieved because of an insufficient gain in insight and poor treatment adherence to all proposed clinical treatments and social support.
He had been abandoned by his mother at 11 years of age and since then exploited in many ways by his antisocial and alcoholic father (also homeless), but there were no other known psychiatric illnesses in his family. The first behavior changes were present since age 16. At age 19, he was diagnosed and treated for toxoplasma chorioretinitis without further sequelae.
Throughout the 85 assessments, we found repeated and quite complete blood tests, EEGs, and brain CT and MRI scans, all without important findings, and there was only one urine sample positive for drugs (cannabis).
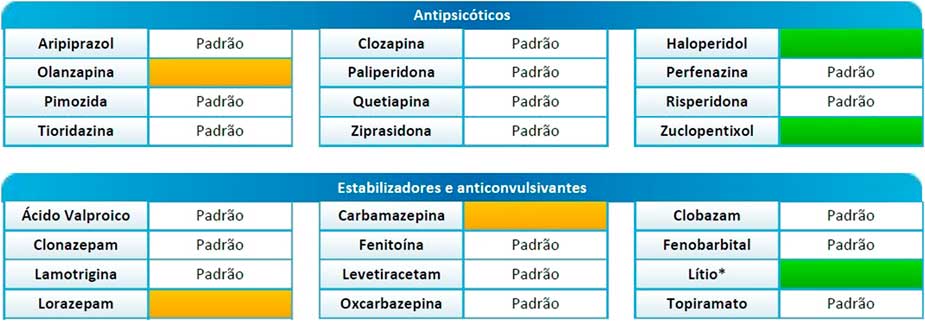
After careful review of the clinical records, we decided to use one of our Neuropharmagen® kits5 with this patient. We found a higher probability (see green color boxes in Figure 1) of positive response to treatment with haloperidol (favorable NEF3 gene polymorphism) and lithium (favorable CACNG2 gene polymorphism), while there appeared to be a normal pattern response (see white color boxes in Figure 1) to both clonazepam and clozapine. Ironically, the patient had been treated many times with some drugs that were not the best option (see yellow color boxes in Figure 1), as he presented fast metabolism of olanzapine (unfavorable CYP1A2 gene polymorphism), carbamazepine (unfavorable EPHX1 gene polymorphism), and lorazepam (unfavorable UGT2B15 gene polymorphism).

Figure 1 Neuropharmagen® pharmacogenetic testing result for antipsychotics (Anti-psicóticos), mood-stabilizers and anticonvulsants (Estabilizadores e Anticonvulsivantes).
After getting these results, his medication was changed to lithium carbonate modified-release 1200 mg AM, clonazepam 2 mg TID, haloperidol 10 mg TID, and clozapine 500 mg PM. Total remission of symptoms was achieved in 4 weeks, and oral haloperidol was then substituted by a monthly long-acting injectable formulation of haloperidol decanoate 300 mg, in order to guarantee maximum therapeutic adherence. Finally, after 25 years of erratic wandering between the urban homeless life and the psychiatric asylum environment, the patient got transferred to a rural charity community residence, where he has been without readmission for 2 years.
We believe that many patients could benefit from psychopharmacogenetics testing, and we eagerly look forward to a time when these kinds of tools will become easier to use.
Acknowledgments
I would like to express my thanks to Pedro Lages Martins (ExpatBiotics, Lisboa, Portugal) and Livia Chaves Pereira (AB-BIOTICS, Barcelona, Spain).
Disclosures
Dr. Gama Marques has nothing to disclose.