A 62-year-old male presented subacutely to a tertiary medical centre after experiencing sudden-onset dysarthria and right arm weakness. The entirety of the symptoms lasted 30 minutes before partially resolving, leaving the man with a minimally weak and clumsy right hand. Initial noncontrast computed tomography (CT) of the head showed no acute findings and CT angiogram (CTA) showed a severely stenosed (80%) proximal left internal carotid artery (ICA) with an associated free-floating thrombus (FFT), which extended 15 mm caudally from its attachment to the posterior aspect of the proximal ICA (Figure 1). The patient was started on intravenous unfractionated heparin and aspirin and was admitted to the stroke service for further observation and workup.

Figure 1 Free-floating thrombus (FFT) visualized by CTA in the left ICA in the axial (A) and sagittal (B) plains. Circumferential blood flow and the elongated nature of the thrombus are depicted in A and B, respectively.
Magnetic resonance imaging of the brain showed multiple acute infarcts scattered throughout the left middle cerebral artery vascular territory, suggestive of an atheroembolic shower.
On the third day, the patient experienced fluctuating neurologic symptoms consisting of dysarthria and dense right arm hemiparesis, despite being normotensive and having a therapeutic activated partial thromboplastin time. Repeat noncontrast computed tomography showed no new acute features, and CTA showed no large vessel occlusion or change in the FFT. The symptoms resolved shortly thereafter. A similar event occurred on day 4 and a transcranial Doppler (TCD) was placed for emboli detection. Over a course of 1 hour, 84 high-intensity transient signals (HITS) were recorded. An oral load of clopidogrel 600 mg was given to the patient and aspirin was discontinued. TCD for emboli detection 4 hours later showed no further HITS over a 1-hour recording period (Figure 2). Repeat emboli detection the next day again showed no HITS over a 1-hour period. No fluctuations in neurological status were noted after the clopidogrel load. Repeat CTA performed the following day showed partial resolution of the FFT and ICA stenosis.
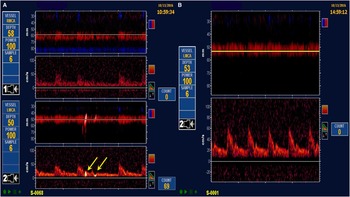
Figure 2 TCD studies before and after clopidogrel load. Multiple HITS, as depicted by yellow arrows, were observed in the left middle cerebral artery territory before loading (A). Four hours after clopidogrel load, no further HITS were detected (B).
TCD ultrasound is frequently used to detect microembolic signals (MES) in ischemic stroke, especially in the setting of extracranial large artery disease,Reference Babikian, Hyde, Pochy and Winter 1 although they have been recorded in other embolic etiologies as well.Reference Tong and Albers 2 MES have been shown to be an independent risk factor for recurrent ischemic stroke in both symptomaticReference King and Markus 3 and asymptomatic carotid disease,Reference Markus, King and Shipley 4 and can be thought of as a surrogate marker of cerebral infarction.Reference Wong 5
There are currently no guidelines regarding treatment of FFTs; as such, optimal treatment regimen is unclear. Interestingly, dual antiplatelet therapy has been shown to decrease the burden of MES in those with either extracranialReference Markus, Droste and Kaps 6 , Reference Wong, Chen and Fu 7 or intracranial carotid disease,Reference Wang, Lin and Zhao 8 but not necessarily associated with FFTs. Furthermore, this decrease in embolization occurs over a period of days, not hours. The addition of a clopidogrel load to aspirin monotherapy has also been shown to decrease the number of asymptomatic MES in those with symptomatic extracranial carotid disease.Reference Tsivgoulis, Kerasnoudis and Krogias 9 A clopidogrel load of 600 mg was chosen because it has been shown to have greater platelet activation with faster onset of action compared to 300-mg loads.Reference Montalescot, Sideris, Meuleman, Bal-dit-Sollier, Lellouche and Steg 10 Dual antiplatelet therapy has also been shown to predict decreased infarct burden on postcarotid stenting magnetic resonance imaging of the brain.Reference Almekhlafi, Demchuk and Mishra 11
Clopidogrel loading added to existing antithrombotic therapy may help decrease the burden of symptomatic and asymptomatic MES in a matter of hours, as suggested by this case given the temporal association between clopidogrel load and MES cessation. It further demonstrates the importance of using real-time monitoring of therapeutic interventions with TCDs. However, because treatment guidelines for FFTs are currently nonexistent, we would suggest caution in initiating triple antithrombotic therapy without careful consideration due to increased risk of bleeding.
Disclosures
The authors do not have anything to disclose.
Statement of Authorship
BRG and BKM were both involved in the care of the patient in this report. BRG prepared the manuscript and BKM proofread and revised it. Both authors read and approved the final manuscript.




