Many doctors like to routinely order an electroencephalogram (EEG) as part of a diagnostic work-up for patients with psychiatric disorders. Often, the reason given is to exclude epilepsy as a cause of the symptoms. When is an EEG justified? How often does it produce a result that the doctor was not expecting or potentially contribute to management of the disorder?
Method
We carried out a simple retrospective analysis of 187 consecutive EEG requests to the Department of Clinical Neurophysiology at Royal Victoria Infirmary, from 22 general adult psychiatrists for a period of 12 months. Subjects were both in-patients and out-patients. All EEGs were reported by one of two consultants in clinical neurophysiology. Data were extracted from the EEG request form, which asked for the clinical reason for the test and the nature of any other medical or psychiatric diagnoses.
Results
There were 104 requests for males and 83 for females. The median age was 32 years (range 16-67). The reasons for the EEG request are listed in Table 1.
Table 1. 187 consecutive electroencephalogram (EEG) referrals from psychiatry — reasons for referral
| Does the patient have epilepsy or not? | 132 (71%) |
| Is there evidence of organic brain disease? | 41 (22%) |
| Has known epilepsy changed? | 6 (3%) |
| Localisation of known epilepsy? | 4 (2%) |
| Has the patient's EEG improved? | 2 (1%) |
| Does the patient have episodic dyscontrol? | 1 (0.5%) |
| Is the patient over-medicated? | 1 (0.5%) |
Further analysis of the request form was carried out for patients in whom the test was to determine whether or not the patient was suffering from epilepsy. Table 2 lists the clinical features on the request form in the 132 patients who fell into this category.
Table 2. 187 consecutive electroencephalogram referrals from psychiatry — clinical features on the request form for 133 patients in whom epilepsy was suspected (some requests had more than one feature)
| Hallucinations (all) | 40 (30%) |
| — auditory | - 21 (16%) |
| — olfactory | - 16 (12%) |
| — visual | - 16 (12%) |
| Attack with loss or alteration in consciousness | 32 (24%) |
| — with jerks | - 3 (2%) |
| — with incontinence | - 3 (2%) |
| Episodic aggression or impulsivity | 25 (19%) |
| Psychosis | 24 (18%) |
| Panic/anxiety attacks | 13 (10%) |
| Confusion | 11 (8%) |
| Aura | 11 (8%) |
| Derealisation/depersonalisation | 9 (7%) |
| Episodes of amnesia | 9 (7%) |
| Unusual nocturnal behaviour | 4 (3%) |
| Personality change | 4 (3%) |
| Episodes of faintness | 4 (3%) |
| Fugue states | 3 (2%) |
We classified the EEG results blind to the details on the request form (Fig. 1). Fifty-eight per cent of the EEGs were normal. Non-diagnostic abnormalities such as diffuse slowing, diffuse excess of fast activity and temporal lobe dysfunction were seen in 36%. In 11 patients (6%), the EEG raised the possibility of a liability to epilepsy. Ten of these 11 patients were being investigated for the possibility of epilepsy. Three of the 11 had already undergone EEGs in the past that were similar, four of them were on therapeutic doses of anticonvulsants prior to the test and two of them already had a diagnosis of epilepsy. However, only in one patient did the EEG show a clear epileplogenic focus — a 46-year-old woman with schizophrenia who did not have a previous diagnosis of epilepsy. Unfortunately, clinical follow-up on these patients was not available.
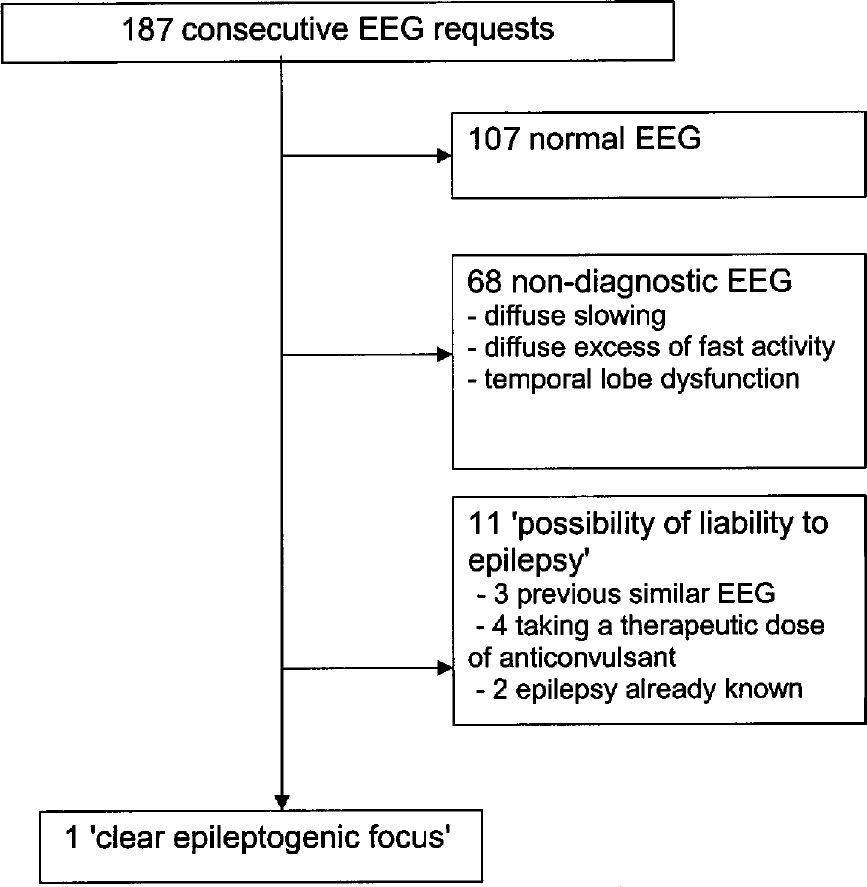
Figure 1. Diagnostic yield in 187 electroencephalogram (EEG) referrals from psychiatry.
In none of the 33 patients where aggression was mentioned on the request form was the EEG result diagnostic.
Conclusions
This study has shown that EEG is still a popular investigation in patients with psychiatric disorder. The two main ways in which the test is used are to look for evidence of epilepsy or to gain evidence that the patient has an organic brain disorder. Although progress continues to be made in the use of sophisticated EEG techniques such as quantitative EEG in the research of psychiatric disorders (Reference Hughes and JohnHughes & John, 1999), a routine EEG in clinical practice has limited value.
In this sample, there was a disappointing yield of one patient with a clear epileptogenic focus. This is similar to the prevalence of such abnormalities in normal subjects (0.5-2%) (Reference Gregory, Oates and MerryGregory et al, 1993). Other recent studies in psychiatry are in keeping with these findings. A study in San Diego found that of 150 EEG requests in their service, 11% were abnormal, but no new diagnoses were made and clinicians ignored the results of three positive EEGs (Reference Lam, Hurwitz and WadaLam et al, 1988). A similar study in Houston found that although 31% of 698 psychiatric inpatient EEGs were abnormal, only 1.7% led to a change in diagnosis (Reference Warner, Boutros and PeabodyWarner et al, 1990). On the other hand, some authors have argued that the yield does justify its use, although they have tended to emphasise the frequency of abnormalities rather than utility (van Sweden et al, 1986).
This study is hampered by the lack of clinical follow-up. We therefore do not know whether the abnormalities that were picked up turned out to be clinically relevant. We also did not set out to determine how useful the clinicians found the EEG results obtained. It may be that a normal or non-diagnostic EEG was helpful to some clinicians. A normal EEG does not strictly exclude any pathology, but the presence of diffuse slowing may reinforce a diagnosis of delirium. This may be particularly true for younger patients whose EEG will not be confounded by age-related changes. In this group, the EEG may be particularly useful in distinguishing between organic conditions, such as early encephalitis, and psychiatric ones such as psychogenic coma. The diagnosis of the acutely abnormal mental state is perhaps the most useful function of the EEG in psychiatry.
An intriguing finding of the study is the lack of any diagnostic EEG information in the 33 patients where aggression had been mentioned on the request form. Aggression seems to be frequently thought of as a possible symptom of epilepsy. Of course, aggression can rarely occur with epilepsy, either as non-directed ictal rage, during postictal confusion or psychosis or as an interictal phenomenon, particularly in patients with temporal lobe epilepsy. However, these scenarios are rare compared with other causes of aggression. For example, in one series, postictal aggression occurred in only six out of 1300 patients with epilepsy, usually after an obvious cluster of seizures (Reference Gerard, Spitz and TowbinGerard et al, 1998). Episodic dyscontrol cannot be diagnosed using an EEG (Reference Drake, Hietter and PakalnisDrake et al, 1992). These results suggest that EEG is only useful in patients with aggression if there is other supporting evidence for epilepsy.
Epilepsy remains foremost a clinical diagnosis made on the basis of the history taken from the patient or witnesses. The false negative rate of interictal EEGs is around 50% (Reference Hopkins, Garman and ClarkeHopkins et al, 1988). In addition to the false positive rate of 2% in the general population, in a psychiatric population non-diagnostic EEG abnormalities, such as temporal lobe dysfunction in bipolar disorder and schizophrenia, may make this false positive rate even higher (Reference Hughes and JohnHughes & John, 1999). Any discussion about the utility of EEG also has to consider the average cost of the test — typically between £100-150 in a UK NHS setting.
All doctors ordering an EEG should be aware of its limitations and continue to rely on a patient's history to make or refute a diagnosis of epilepsy.






eLetters
No eLetters have been published for this article.