We are reporting on a 22-year-old female, native of Burundi, who presented to the emergency department with a 2-week history of severe bilateral cervico-occipital pain and nuchal rigidity. She denied any fever, rashes, neurological deficits, trauma, or recent infections. She was afebrile and hemodynamically stable. Physical examination revealed nuchal swelling, tenderness, and rigidity. There were no lymphadenopathies or focal neurological deficits. Laboratory investigations revealed leukocytosis at 14.4 × 109/L. Serologies for HIV, hepatitis, and syphilis were negative.
The patient had been discharged from the emergency department 2 weeks prior with a diagnosis of occipital neuralgia. However, clinical presentation and nuchal rigidity were concerning for an infectious process, and a CT scan was ordered prior to lumbar puncture.
Imaging demonstrated evidence of abscess formation in the semispinalis capitis muscles (Figure 1). The abscess was surgically drained and cultures grew Staphylococcus aureus. She rapidly improved on intravenous Ceftriaxione, Vancomycin, and Metronidazole and was discharged on a 2-week course of Cloxacillin.
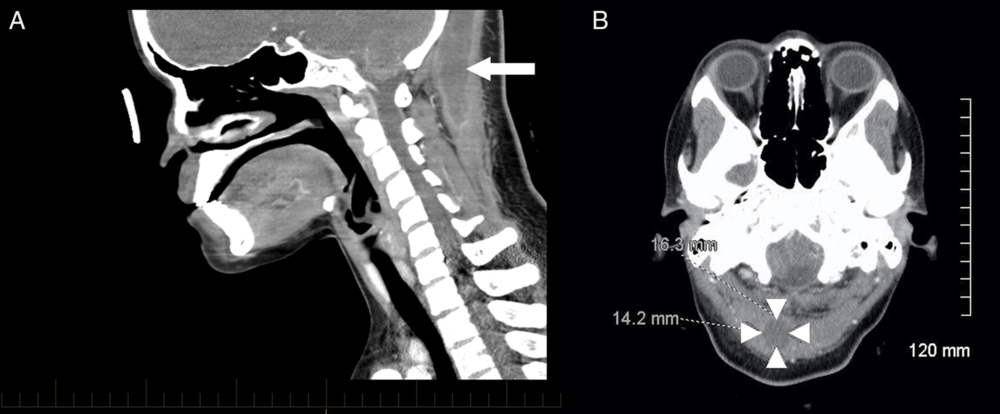
Figure 1: Computed tomography of the head and neck with intravenous contrast showed a 37 × 17 × 8 mm homogenous hypodense collection with ring enhancement extending from the occiput to the cervical spine C3-4 level. (A, sagittal view, arrow). The collection was located predominantly within the right semispinalis capitis muscle (B, axial view, arrowheads) with a smaller extension in the upper left semispinalis capitis muscle.
The patient presented with unprovoked cervico-occipital pain. An infectious process was not initially suspected as she was afebrile. Classically, patients with pyomyositis present with fever, myalgia, and localized tenderness.Reference Chauhan, Jain and Varma1 Pyomyositis is most frequently seen in tropical regions, occurs in males aged 20–40 years, and most commonly affects lower limb muscles.Reference Chauhan, Jain and Varma1 Pyomyositis can occur in healthy individuals, but often predisposing factors such as immunodeficiency, trauma, injection drug use, concurrent infection, and malnutrition can be identified.Reference Crum2
Pyomyositis is thought to arise via hematogenous spread and leads to multiple abscess formation.Reference Stevens, Bisno and Chambers3 It can be complicated by local destruction of the vertebrae, septic shock, endocarditis, septic emboli, brain abscess, or rhabdomyolysis.Reference Lin, Rezai and Schwartz4S. aureus has been implicated in 75–90% of cases.Reference Crum2 Early diagnosis and source control via high-dose antibiotics plus either percutaneous drainage or surgical intervention are necessary to reduce the risk of morbidity.Reference Chiedozi5
The initial misdiagnosis as occipital neuralgia underlines the importance of considering this rare condition in the differential diagnosis of cervicalgia in the emergency setting, even in healthy immunocompetent patients.
Acknowledgments
The authors wish to acknowledge the contribution of Dr Sebastian Demyttenaere, Department of General Surgery, and Dr Joe Dylewski, Division of Infectious Diseases, St Mary’s Hospital Centre, Montreal, to the clinical care of this patient.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
HG is involved in initial clinical evaluation, literature review, and drafting of the manuscript and revision. MGZ supervised clinical evaluation and management of the patient and contributed to drafting and final review of the manuscript.



