Introduction
In the UK, 7.9% of 11- to 16-year-olds meet diagnostic criteria for an anxiety disorder (Vizard et al., Reference Vizard, Pearce, Davis, Sadler, Ford, Goodman and McManus2018). While 21% of adolescents in the general population experience sleep problems (Short et al., Reference Short, Gradisar, Gill and Camfferman2013), these problems are more common amongst adolescents with anxiety (Alfano et al., Reference Alfano, Ginsburg and Kingery2007). In adolescents aged 12–16 years with high levels of anxiety symptoms, 38.1% met criteria for insomnia (i.e. difficulty initiating or maintaining sleep or early wakening), 34.8% reported short sleep duration ( < 7 hours per night), and 83.1% reported long (>30 minutes) sleep onset latency (i.e. time to fall asleep) (Haugland et al., Reference Haugland, Hysing, Baste, Wergeland, Rapee, Hoffart and Bjaastad2021). The recommended amount of sleep for adolescents is 8–10 hours per night (Paruthi et al., Reference Paruthi, Brooks, D’Ambrosio, Hall, Kotagal, Lloyd and Rosen2016), although worldwide, between 32 and 86% of adolescents obtained recommended sleep on school nights and between 79 and 92% on weekends (Gariepy et al., Reference Gariepy, Danna, Gobiņa, Rasmussen, de Matos, Tynjälä and Schnohr2020). Evidence suggests that the relationship between sleep problems and anxiety symptoms in adolescents may be bi-directional (Dahl and Lewin, Reference Dahl and Lewin2002), with anxiety symptoms predicting sleep problems (Johnson et al., Reference Johnson, Roth and Breslau2006), and childhood sleep problems predicting adolescent anxiety symptoms (Orchard et al., Reference Orchard, Gregory, Gradisar and Reynolds2020). Both anxiety and sleep problems in adolescents are associated with poor academic, social and health outcomes (Sadler et al., Reference Sadler, Vizard, Ford, Marchesell, Pearce, Mandalia and McManus2018), emphasising the need for effective treatments. This makes it important to investigate whether treating one may have a positive impact on the other.
Using subjective and objective measurement, several sleep difficulties have been identified in young people with anxiety disorders, but the extent to which this generalises to adolescents specifically is unclear as studies have typically included children and adolescents across broad age ranges. For example, in children and adolescents with anxiety disorders aged 6–17 years, according to parents and clinicians, difficulties initiating or maintaining sleep, nightmares, and resistance to sleeping alone, were highly prevalent, with 88% experiencing at least one sleep problem and 55% experiencing three or more (Alfano et al., Reference Alfano, Ginsburg and Kingery2007). Forbes et al. (Reference Forbes, Bertocci, Gregory, Ryan, Axelson, Birmaher and Dahl2008) extended the work through self-report of sleep and polysomnography in children and adolescents (7–17 years) with anxiety disorders. Both objective and subjective measures revealed an increased sleep onset latency in children and adolescents with anxiety disorders, versus control participants. Objective evidence indicated frequent night-time awakening in those with anxiety disorders compared with those without.
Sleep difficulties in adolescents may differ from those experienced by children due to biological processes, such as the normal shift (delay) in circadian rhythm that occurs in puberty (Crowley et al., Reference Crowley, Wolfson, Tarokh and Carskadon2018). There may also be external factors that are specific to adolescents (e.g. greater homework, and academic workload, use of electronic media, and increased caffeine intake in the evenings; Owens and Weiss, Reference Owens and Weiss2017). Further research is therefore required to better understand the nature of sleep difficulties in adolescents with anxiety disorders. Given the differences in sleep patterns on weekday and weekend nights for children with anxiety disorders (e.g. Hudson et al., Reference Hudson, Gradisar, Gamble, Schniering and Rebelo2009), it would also be important to explore this further in adolescents. Due to these biological and environmental changes, it might be expected that adolescents would suffer with decreased total sleep time and increased sleep onset latency on weekdays when they must get up early for school, but not weekends, where they may ‘catch up’ on sleep.
Cognitive behavioural therapy (CBT) is an empirically supported treatment for anxiety disorders, with remission rates around 50% for primary anxiety disorders in children and adolescents (James et al., Reference James, Reardon, Soler, James and Creswell2020). Furthermore, adolescent treatments that are brief, intensive, or concentrated have been developed and found to be effective (e.g. Stjerneklar et al., Reference Stjerneklar, Hougaard, McLellan and Thastum2019). However, the extent to which CBT resolves sleep problems within adolescents is still largely unknown.
Within broad age samples combining children and adolescents, studies of CBT for anxiety disorders provide preliminary evidence of improvements in sleep difficulties post-treatment. In a sample of children and adolescents, aged 7–17 years, with a primary diagnosis of social phobia, generalised anxiety disorder, or separation anxiety disorder, Caporino et al. (Reference Caporino, Read, Shiffrin, Settipani, Kendall, Compton and Keeton2017) found that both CBT and sertraline, and CBT alone, produced significant reductions in sleep problems, with small to medium effect sizes. Peterman et al. (Reference Peterman, Carper, Elkins, Comer, Pincus and Kendall2016) also investigated the effectiveness of CBT on sleep problems, amongst children and adolescents with anxiety disorders (7–17 years). They found that parent-reported sleep problems (but not child-reported sleep problems), improved following CBT for anxiety disorders; specifically, sleep issues (medium to large effect sizes) around bedtime (e.g. bedtime resistance, sleep anxiety), rather than quantitative sleep variables (e.g. sleep latency, sleep duration). Nevertheless, parent-reported mean scores on the Children’s Sleep Habits Questionnaire were still around the clinical cut-off, suggesting that many sleep difficulties persisted. Notably, however, none of the studies reported baseline and outcome data for adolescents specifically.
The negative consequences of sleep problems (Sadler et al., Reference Sadler, Vizard, Ford, Marchesell, Pearce, Mandalia and McManus2018) and the bi-directional relationship between sleep problems and anxiety symptoms (Dahl and Lewin, Reference Dahl and Lewin2002), make it important to investigate whether psychological treatments based on CBT for anxiety disorders effectively improve sleep in adolescents with anxiety disorders. Currently, however, research on the link between anxiety and sleep problems is primarily focused on groups involving both children and adolescents, and less is known about the nature of sleep problems experienced by adolescents with anxiety disorders (rather those with high levels of symptoms), how sleep changes between weekdays and weekends, and whether sleep improves through treating anxiety disorders.
The present paper aims to build upon previous research by improving our understanding of sleep problems (for weekday and weekends nights) in a sample of adolescents with an anxiety disorder and by examining whether CBT for the treatment of the anxiety disorder has a positive impact on the adolescents’ sleep. Accordingly, we set out to examine the following questions amongst adolescents seeking treatment for an anxiety disorder:
-
(1) What is the presentation of sleep patterns and insomnia symptoms amongst adolescents with an anxiety disorder for weekdays and weekends at baseline?
-
(2) Are there significant differences in sleep patterns between weekdays and the weekend at baseline?
-
(3) Are there significant improvements in sleep patterns and insomnia symptoms following CBT for an anxiety disorder?
Based on previous research, we hypothesised that pre-treatment adolescent sleep patterns would be significantly worse on weekdays versus weekends, and that following CBT, sleep patterns and insomnia symptoms in adolescents would significantly improve.
Method
Participants
Data for 179 participants were gathered between April 2018 and November 2019, prior to the COVID-19 pandemic, from a regional out-patient child and adolescent mental health service that provides brief interventions to children and adolescents (7–17 years) for the treatment of a primary anxiety or depressive disorder in the Southeast of England. The service accepts referrals from primary and secondary care services and is funded through the UK National Health Service (NHS). Young people are not eligible for the service if they have been diagnosed with an autistic spectrum disorder, learning disabilities, suicidal intent, or recurrent or potentially life-limiting self-harm (i.e. current frequency of at least once per week or self-harm that requires medical attention), if they have been identified by social services as currently ‘at risk’ due to, for example, child protection concerns, or if they have been prescribed psychotropic medication.
To be included in this study, participants were required to be aged 11–17 years, with a primary diagnosis of one of the following DSM-5 (American Psychological Association, 2013) anxiety disorders: social anxiety disorder, generalised anxiety disorder, separation anxiety disorder, panic disorder, agoraphobia, or a specific phobia. Post-traumatic stress disorder and obsessive-compulsive disorder were excluded.
To be included in the analyses, participants were required to have completed baseline self-report sleep measures between April 2018 and November 2019. For the analysis of change in sleep patterns and insomnia symptoms following CBT for the treatment of an anxiety disorder, participants were included if they had completed a course of CBT and post-treatment self-report sleep measures. Participants were classed as ‘treatment completers’ if they attended at least 50% of the treatment sessions, as per the service’s guidelines. Table 1 provides demographic and clinical baseline data for participants who had completed pre- (n=135) and post-treatment data (n=73).
Table 1. Demographic and clinical data for those with completed pre- and post-treatment data

RCADS, Revised Child Anxiety and Depression Scale. Diagnoses of anxiety and externalizing disorders were assessed using the Anxiety Disorders Interview Schedule (ADIS-IV-C/P), and major and persistent depressive disorder and mania were assessed using the Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime.
Procedure
Adolescents and parents attended pre-treatment diagnostic assessments (reporting on the adolescent) separately and completed baseline self-report sleep and anxiety measures. All assessments were carried out by trained psychology graduates or clinicians working within the service. Assessors were trained to high levels of reliability and received supervision for every assessment from a clinical psychologist (or equivalent) with extensive experience of delivering and supervising diagnostic assessments and proven reliability. Following a diagnosis of a primary anxiety disorder, adolescents were then offered CBT within the service. If the adolescent was aged 12–17 years, it was delivered either individually or within a group, and if they were aged 11 years, it was delivered via their parent/carer. Forty-seven adolescents (12.6%) received parent-delivered treatment, and for 127 (84.1%), the treatment was delivered directly to the adolescent. All treatments were delivered by clinical psychologists or low-intensity CBT therapists (who had all completed a one-year postgraduate training programme) – either Psychological Wellbeing Practitioners (PWPs) with further in-service training in working with children and young people, or Children’s Wellbeing Practitioners (CWPs) (Health Education England, 2017; Wood & Turnbull, Reference Wood and Turnbull2023). Treatment was delivered between April 2018 and November 2019.
Once treatment ended, participants completed the same self-report questionnaire measures as provided prior to the initial assessment and were then discharged from the service. Due to resource limitations, diagnostic assessments were conducted only at pre-treatment.
Interventions
Overcoming group treatment for parents of adolescents (aged 11 years)
Adolescents aged 11 years were treated via guided parent-delivered group CBT (which is the standard treatment within the clinic for young people aged 7–11 years) (Halldorsson et al., Reference Halldorsson, Elliott, Chessell, Willetts and Creswell2021). Parents received five weekly group sessions, which each lasted 1.5 hours. A book (‘Overcoming Your Child’s Fear and Worries: A Self-Help Guide for Parents’; Creswell and Willetts, Reference Creswell and Willetts2012; updated to ‘Helping your Child with Fears and Worries: A Self-Help Guide for Parents’; Creswell and Willetts, Reference Creswell and Willetts2019) accompanied the treatment, which parents were required to read ahead of each session. Parents completed homework tasks between sessions, independently and with their child. The group involved supporting parents to work through the book, rehearse skills, and problem-solve difficulties.
‘Chilled’ group CBT treatment for adolescents (aged 12 and above)
The Adolescent version of the Cool Kids Child and Adolescent Anxiety Program (Rapee et al., Reference Rapee, Lyneham, Schniering, Wuthrich, Abbott, Hudson and Schniering2006), known as ‘Chilled’, is a well-established anxiety management program that teaches CBT techniques for managing anxiety. This was adapted to be delivered in eight group sessions lasting from 90 minutes to 2 hours, and a booster session after 3 months. The groups included the following topics: psychoeducation, thoughts and feelings, realistic thinking, exposure, managing emotions, problem solving and, at the final session, relapse prevention. Treatment was delivered by two clinicians in small groups of around five adolescents. There were also two parent sessions, to help parents learn how to support in treatment, which ran alongside the adolescent’s session.
Individual treatment for adolescents (aged 12 and above)
This treatment was delivered individually to adolescents, and parents were included in line with the preferences of the young person and their needs. Sessions included the development of a formulation based on the person’s own beliefs, safety behaviours and symptoms, testing beliefs through behavioural experiments, and the development of a blueprint at the end of treatment. The treatment involved six sessions of between 60 and 90 minutes delivered over 10 weeks, with a further booster session 12 weeks after treatment completion. Each session lasted between 1 and 1.5 hours.
Measures
Diagnostic assessment
The pre-treatment diagnostic assessment used sections from two validated semi-structured interview schedules to determine whether the young person met diagnostic criteria for an anxiety/depressive disorder: the Anxiety Disorders Interview Schedule (ADIS-IV-C/P; Silverman et al., Reference Silverman, Albano and Barlow1996) (adapted for DSM-5) and the Kiddie Schedule for Affective Disorders and Schizophrenia Present and Lifetime (K-SAD-S-PL; Kaufman et al., Reference Kaufman, Birmaher, Brent, Rao, Flynn, Moreci and Ryan1997). Within the service, the ADIS is used to assess DSM-5 diagnoses of anxiety and externalising disorders in young people. This tool has excellent inter-rater reliability (Lyneham et al., Reference Lyneham, Abbott and Rapee2007) and concurrent validity (Wood et al., Reference Wood, Piacentini, Bergman, McCracken and Barrios2002). The K-SAD-S-PL was used to assess DSM-5 major and persistent depressive disorder and mania. This instrument has good concurrent validity of screens and K-SAD-S-PL diagnoses, and excellent inter-rater and test–retest reliability (Kaufman et al., Reference Kaufman, Birmaher, Brent, Rao, Flynn, Moreci and Ryan1997).
Using parent and adolescent reports, clinicians assigned clinical severity ratings (CSRs) to diagnoses (as is standard practice with the ADIS) using a 9-point scale (0–8), with ‘0’ indicating no impairment and ‘8’ indicating severe impairment. Impairment is defined as affecting the young person’s life and/or creating significant distress. A CSR ≥4 signifies a clinical diagnosis. The disorder with the highest CSR was allocated as the primary diagnosis.
Symptoms of anxiety and depression
Pre- and post-treatment anxiety and depression symptoms were assessed using the Revised Child Anxiety and Depression Scale, Child Version (RCADS-C; Chorpita et al., Reference Chorpita, Yim, Moffitt, Umemoto and Francis2000). The RCADS is a 47-item questionnaire measure of symptoms of anxiety and depression in young people, aged from 8 to 18 years. It consists of six subscales: separation anxiety disorder, social phobia, obsessive-compulsive disorder, panic disorder, generalised anxiety disorder, and major depressive disorder. Respondents rate how often each item applies to them/their child, using a 4-point scale from 0 (‘never’) to 3 (‘always’). The RCADS has been shown to have good psychometric properties in a clinical sample (Chorpita et al., Reference Chorpita, Moffitt and Gray2005). In the current study, it had excellent internal consistency for both the Anxiety Total score (Cronbach’s α: pre=.998, post=1.00) and the overall Total score (Cronbach’s α: pre=.998, post=1.00).
Sleep questionnaire
The sleep questionnaire gathered self-report information regarding sleep patterns and insomnia symptoms. Items were adapted from the Sleep Habits Survey (SHS; Wolfson et al., Reference Wolfson, Carskadon, Acebo, Seifer, Fallone, Labyak and Martin2003) and the Insomnia Severity Index (ISI; Morin, Reference Morin1993). In this study, we examined responses to seven questions (taken from the SHS) about adolescent’s sleep patterns over the past 2 weeks, in which they reported their sleep and awakening times. Adolescents provided separate answers for weekday nights (Sunday to Thursday) and weekend nights (Friday and Saturday). Variables included: sleep onset latency (SOL; the difference between the time the participant got into bed and the time they fell asleep); frequency of night-time waking (number of times awake during the night); wake after sleep onset (WASO; total time spent awake during the night); and total sleep time (TST; time between sleep onset and waking time minus WASO).
We also examined a further two items regarding insomnia symptoms (adapted from the ISI; Morin, Reference Morin1993). The variables included: initial insomnia (‘Difficulty falling asleep’) and middle insomnia (‘Difficulty staying asleep’) and both items were scored on a 5-point Likert scale: 0 (‘no problem’), 1 (‘mild’), 2 (’moderate’), 3 (‘severe’) and 4 (‘very severe’). Initial insomnia and middle insomnia variables on the ISI do not distinguish between weekend and weekday nights The SHS has demonstrated good validity (Wolfson et al., Reference Wolfson, Carskadon, Acebo, Seifer, Fallone, Labyak and Martin2003), and the ISI total score has been shown to be both reliable and valid at detecting insomnia and is sensitive to treatment response in clinical patients (Morin et al., Reference Morin, Belleville, Bélanger and Ivers2011), including adolescents (Brooks et al., Reference Brooks, Sayers, Virani, Rajaram and Tomfohr-Madsen2019; Chahoud et al., Reference Chahoud, Chahine, Salameh and Sauleau2017; Wolfson et al., Reference Wolfson, Carskadon, Acebo, Seifer, Fallone, Labyak and Martin2003).
Power analysis
A power analysis using the G*Power computer program (Erdfelder et al., Reference Erdfelder, Faul and Buchner1996) indicated that to examine whether there were improvements in sleep patterns and subjective experiences of insomnia following CBT for an anxiety disorder, a total sample of 27 participants would be needed to detect a medium effect (d=.50) with 80% power using a paired sampled t-test between means with α at .05. A medium effect size was chosen as previous research (Caporino et al., Reference Caporino, Read, Shiffrin, Settipani, Kendall, Compton and Keeton2017; Peterman et al., Reference Peterman, Carper, Elkins, Comer, Pincus and Kendall2016) reported medium effect sizes. This study was powered to a small effect size.
Results
Data preparation and preliminary analyses
Data were analysed using SPSS (version 27). Prior to analyses, variables were screened for assumptions of normality, outliers, and missing data. A table on missing data can be found in the Supplementary material. All baseline and post-treatment variables violated the assumption of normality. Outliers were present for several baseline and post-treatment variables, but were not excluded from the analysis. All participants with baseline data were included in the study for research questions 1 and 2, but were excluded from the analysis for research question 3 if post-treatment sleep data were missing. Missing data at post-treatment was relatively high (45%). Missing data were excluded ‘listwise’ from the analysis rather than using multiple imputation, as multiple imputation procedures typically assume that data are normally distributed, so including non-normally distributed (as with the present data) would introduce bias (Sterne et al., Reference Sterne, White, Carlin, Spratt, Royston, Kenward and Carpenter2009).
Descriptive statistics examined baseline and post-treatment sleep patterns and insomnia symptoms. As assumptions for parametric tests were violated, non-parametric alternatives were used to conduct the analyses. The Wilcoxon signed rank test failed to meet an assumption whereby data distribution needed to be symmetrical. To examine differences between weekday and weekend nights for baseline sleep patterns and differences from pre- to post-treatment in sleep patterns and insomnia symptoms, the sign test was used as this is recommended when such assumptions are not met (Field, Reference Field2009) and data were reported significant if p < .01.
As sleep disturbance is one of the most common symptoms of adolescent depression (Goodyer et al., Reference Goodyer, Reynolds, Barrett, Byford, Dubicka, Hill and Senior2017; Orchard et al., Reference Orchard, Pass, Marshall and Reynolds2017), sensitivity analyses were conducted excluding adolescents with co-morbid, secondary depression diagnoses to check whether this changed the pattern of the findings. Sensitivity analyses were also conducted for treatment delivery, i.e. CBT delivered via the parent (for those aged 11) or adolescent (for those aged 12 and above). These were conducted by re-running analyses with and without depression and with and without those who received parent-led treatment.
Question 1: The presentation of sleep patterns and insomnia symptoms amongst adolescents with an anxiety disorder pre-treatment
Table 2 presents the means and standard deviations for weekday and weekend sleep pattern variables and insomnia symptoms (initial and middle insomnia). Across weekdays and weekends, adolescents reported taking over 1 hour to fall asleep on average. Weekday nights also revealed reduced total sleep time (< 7 hours) compared with weekends (>8 hours) and increased night-time waking, and wake after sleep onset times, than weekends. On the items from the ISI, adolescents’ average scores at baseline fell between the Likert scale scores of ‘mild’ to ‘moderate’ difficulties for initial insomnia and ‘none’ to ‘mild’ difficulties for middle insomnia.
Table 2. Baseline sleep patterns and insomnia symptoms for the whole sample
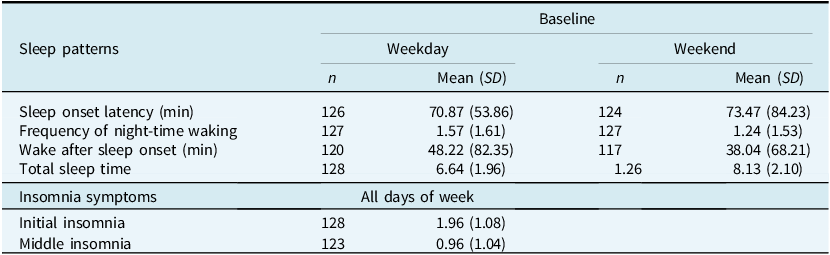
Question 2: Differences in sleep patterns at baseline between weekdays and the weekend
On weekday nights, compared with weekends, adolescents reported significantly less total sleep time (Z=–7.09, p < .001) and were significantly more likely to experience night-time waking (Z=–3.32, p < .001). However, there was no significant difference between weekday and weekend nights for sleep onset latency (Z=–.64, p=.525) and wake after sleep onset (Z=–1.96, p < .050). Sensitivity analyses for depression revealed no differences in the pattern of results.
Question 3: Improvements in sleep patterns and insomnia symptoms following CBT for an anxiety disorder
Table 3 presents the means and standard deviations for weekday and weekend sleep pattern variables and insomnia symptoms (initial and middle insomnia) for pre- and post-treatment. It also presents the clinical outcomes in relation to the adolescents’ anxiety and anxiety/depression symptoms following treatment and demonstrates significant improvements in anxiety/depression symptoms.
Table 3. Sleep patterns, insomnia symptoms, and symptoms of anxiety/depression pre- and post-treatment

Weekend nights include Friday and Saturday nights, and weekday nights incude Sunday to Thursday nights. Initial insomnia and middle insomnia variables did not distinguish between weekend and weekday nights and used a Likert scale from 0 to 4.
Following CBT, for weekday nights, adolescents reported a significant improvement from pre- to post-treatment for sleep onset latency (Z=–3.50, p < .001) and total sleep time (Z=–3.91, p < .001), with reduced sleep onset latency and increased total sleep time. Frequency of night-time waking (Z=–2.01, p < .045) and wake after sleep onset (Z=–1.64, p=.100) did not show significant improvements. For weekend nights, there was a significant improvement from pre- to post-treatment, for sleep onset latency (Z=–3.44, p < .001). There was no significant difference from pre- to post-treatment for frequency of night-time waking (Z=–.98, p=.327), wake after sleep onset (Z=–2.09, p=.074), and total sleep time (Z=–1.95, p=.052). Sensitivity analyses were broadly consistent with this pattern. While there was no difference in the patterns for participants with and without depression, when we excluded participants for whom the format was parent-led group CBT, there was a significant difference post-treatment in the frequency of night-time waking on weekday nights (Z=–3.578, p < .001), with a significant reduction in night-time waking on weekdays.
There was no significant improvement in insomnia symptoms in relation to difficulty falling asleep (Z=–1.95, p=.052, r=–.169) and in difficulty staying asleep (p=.405) from pre- to post-treatment. Sensitivity analyses for depression and treatment delivery format revealed no differences in the pattern of results for insomnia symptoms.
Discussion
This study examined the characteristics of sleep problems amongst adolescents with an anxiety disorder, and whether brief psychological treatments based on CBT for anxiety disorders also significantly improves sleep. Prior to treatment, adolescents reported mild to moderate initial insomnia (taking on average over 1 hour to fall asleep). As hypothesised, sleep was poorer on weekday nights compared with weekend nights in terms of total sleep time (<7 hours versus >8 hours) and greater night-time waking. However, unexpectedly, there were no differences between weekday and weekend nights for sleep onset latency and wake after sleep onset. We found that CBT was successful in treating the adolescents’ anxiety symptoms, with a large effect size. As hypothesised, following CBT, adolescents reported a significant improvement in sleep onset latency and total sleep time for weekday nights. However, there was no change in the frequency of night-time awakening or wake after sleep onset following treatment. This could perhaps be due to floor effects, such that if adolescents were reporting no night-time waking then this cannot be improved upon. For instance, the average frequency of night-time waking at baseline for weekday and weekend was reported as 1.57 and 1.24, respectively, indicating that adolescents self-reported mild difficulties with waking up during the night, therefore limiting the likelihood for further improvement.
Our findings that adolescents experienced sleep difficulties across a range of domains pre-treatment are consistent with previous research, such that Alfano et al. (Reference Alfano, Ginsburg and Kingery2007) and Forbes et al. (Reference Forbes, Bertocci, Gregory, Ryan, Axelson, Birmaher and Dahl2008) found difficulties in initiating and maintaining sleep in children and adolescents with anxiety disorders. However, baseline self-reported insomnia symptoms contrast with the above research, with adolescents reporting none to mild middle insomnia difficulties. This variation in results could perhaps be explained by age differences (i.e. this study focused on adolescents aged 11–17 years, whereas the previous research included children and adolescents aged 6–17 years) and measurement differences using polysomnography and questionnaires completed by children, parents and clinicians in previous research. It may also reflect differences in items administered, i.e. the current study used items from the Sleep Habits Survey (SHS; Wolfson et al., Reference Wolfson, Carskadon, Acebo, Seifer, Fallone, Labyak and Martin2003) and the Insomnia Severity Index (ISI; Morin, Reference Morin1993), whereas previous studies have used a sleep questionnaire with a visual analogue scale for sleep quality, ease of waking, number of awakenings, time awake, and sleep latency (Forbes et al., Reference Forbes, Bertocci, Gregory, Ryan, Axelson, Birmaher and Dahl2008) and a sleep measure made up of three separate measures: Pediatric Anxiety Rating Scale (Riddle and Greenhill, Reference Riddle and Greenhill2002), Hamilton Anxiety Rating Scale (Hamilton, Reference Hamilton1959), and Child Behaviour Checklist-Parent Version (Achenbach and Edelbrock, Reference Achenbach and Edelbrock1991; Alfano et al., Reference Alfano, Ginsburg and Kingery2007).
Our findings of significant differences for weekday and weekend sleep are consistent with the limited literature investigating weekday and weekend sleep. For example, Hudson et al. (Reference Hudson, Gradisar, Gamble, Schniering and Rebelo2009) also found that children and adolescents with anxiety disorders reported going to bed significantly later, more frequent night-time awakenings, and reduced total sleep time on weekday than weekend nights. The finding of differences, particularly in relation to total sleep time, are unsurprising given societal demands for early waking and morning activity on weekdays (Crabtree and Williams, Reference Crabtree and Williams2009). Greater night-time awakening seen on weekday nights may also reflect worries, many of which may relate to the school environment, such as academic work and social interactions (Owczarek et al., Reference Owczarek, McAnee, McAteer and Shevlin2020). Given the high levels of generalised anxiety disorder and social anxiety disorder in this study, school is perhaps especially triggering and therefore particularly affects weekday sleep.
Following treatment for anxiety disorders, in line with previous research combining children and adolescents with anxiety symptoms (Caporino et al., Reference Caporino, Read, Shiffrin, Settipani, Kendall, Compton and Keeton2017; Peterman et al., Reference Peterman, Carper, Elkins, Comer, Pincus and Kendall2016), weekday sleep showed significant improvements; specifically sleep onset latency and total sleep time. Nevertheless, it is worth noting that the average amount of sleep was less than 7 hours and therefore remained below the recommended guidance of 8–10 hours (Paruthi et al., Reference Paruthi, Brooks, D’Ambrosio, Hall, Kotagal, Lloyd and Rosen2016). Given that our participants were all adolescents, there may be specific developmental factors that make it challenging to reach recommended amounts, such as school wake up times, and academic, social, and extracurricular activities occurring in the evening. Biological processes, such as phase delayed circadian rhythms and changes in adolescent brain structure and organisation associated with larger declines in slow wave sleep and slow wave activity are also likely to play a role (Colrain and Baker, Reference Colrain and Baker2011). Consequently, further intervention around sleep may be beneficial, potentially taking place in community settings, such as schools.
Improvements in sleep over the course of treatment for anxiety provides further support for the bi-directional relationship between sleep and anxiety, with evidence here suggesting that changing anxiety can alter sleep. However, it is not possible to determine from the present data if psychological techniques improve sleep and anxiety directly, or if improvement in sleep is a by-product of improvements in anxiety. Further research understanding the mechanisms of change is warranted.
The lack of significant improvements in sleep pattern variables over weekend nights may have resulted from adolescents typically having increased freedom with weekend sleep patterns (Crabtree and Williams, Reference Crabtree and Williams2009). Furthermore, sleep averages were around the recommended amounts on the weekend, resulting in less room for improvement. Insomnia symptoms also revealed that adolescents’ perceptions of difficulty falling asleep or staying asleep did not significantly improve from pre- to post-treatment, despite significant change in sleep patterns. This may have resulted from the relatively low scores at baseline. Additionally, as outlined earlier, it is also possible that some of the sleep difficulties could be driven by school-related worries, and therefore has less of an impact on weekends.
This study benefited from several methodological strengths. All adolescents received a gold standard diagnostic assessment prior to treatment. The heterogeneous sample, in terms of diagnoses, contributes to the generalisability of findings. For instance, the sample included those with primary anxiety and co-morbid depression diagnoses, reflecting ‘real-world’ adolescents. In addition, by including only adolescents this prevents the data from being skewed by differences in sleep patterns in children. Furthermore, sensitivity analyses including adolescents with anxiety disorders indicated that co-morbid depression had little impact on the overall results. External validity was also strengthened by the various treatments and formats provided.
Several important limitations are, however, worth acknowledging. The study relied on subjective sleep measurement. Self-reported improvement in post-treatment sleep may reflect improvements in anxiety and depression symptoms, and thus perceptions of sleep, rather than changes in objective sleep quality (Reynolds et al., Reference Reynolds, Orchard, Midgley, Kelvin and Goodyer2020). Similarly, negative perceptual biases are common in adolescents with anxiety, thus perceived sleep quality may be a misrepresentation of actual sleep quality, with adolescents over-estimating their sleep difficulties (Reynolds et al., Reference Reynolds, Orchard, Midgley, Kelvin and Goodyer2020). Such discrepancies have been reported to exist between subjective and objective measurement (Alfano et al., Reference Alfano, Patriquin and De Los Reyes2015). It is noteworthy that items from the Sleep Habits Survey identified greater improvements in sleep compared with items from the Insomnia Severity Index. It is possible that this is due to the ISI focusing on more of a subjective experience of insomnia and thus based on subjective adolescent perspectives. However, given the common difficulties experienced by adolescents in getting sufficient sleep (Dawson, Reference Dawson2005), it is surprising that the ISI revealed mild difficulties at baseline. This potential difference in reporting patterns would be useful to explore in future work to confirm if this difference exists. The use of objective measures of sleep (e.g. actigraphy or polysomnography) would also help to elucidate these results. In addition, the service collected data using items from the sleep measures rather than the full scales to reduce burden on patients, and therefore clinical cut-offs could not be used. This may have had a detrimental effect on the reliability and validity of the measures.
Furthermore, the sleep questionnaire was administered to adolescents over different seasons (e.g. during term-time and school holidays), as they were administered in a routine clinical service. Sleep habits are likely to be different in school holiday periods in comparison with term-time, where sleep could be exacerbated by various factors including school stress and early wake times. To better understand the presentation of sleep patterns and insomnia symptoms in adolescents with an anxiety disorder, it would be helpful to be able to compare them with other groups, including community populations and those with sleep disorders. Conclusions concerning effectiveness of treatment are also limited by a lack of a waitlist control group, as sleep may spontaneously improve over time. Finally, missing post-treatment data were relatively high (45%). Missing data were present as some participants had not started treatment, whilst others had not completed post-treatment questionnaires.
In conclusion, the results show that prior to treatment, adolescents with anxiety disorders experience significant difficulties with sleep onset latency, frequency of night-time awakening, wake after sleep onset, and total sleep time. CBT for anxiety disorders shows improvements in some of these areas (i.e. total sleep time, sleep onset latency), and may indicate a return to a more ‘common’ level of sleep disruption. Further research is needed to understand discrepancies between subjective and objective sleep, and to explore avenues for the delivery of support for sleep problems.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1352465824000195
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, P.W. The data are not publicly available due to their containing information that could compromise the privacy of research participants. Research materials can be accessed by contacting P.W.
Acknowledgements
The authors thank the adolescents who took part in this study, as well as clinicians and staff from the Anxiety and Depression in Young People (AnDY) Clinic, Poppy Elvin for help with data entry, and the Berkshire Healthcare NHS Foundation Trust for supporting this research.
Author contributions
Olivia Sukiennik: Conceptualization (equal), Data curation (lead), Formal analysis (lead), Investigation (equal), Methodology (equal), Project administration (lead), Resources (equal), Software (equal), Writing – original draft (lead), Writing – review & editing (lead); Polly Waite: Conceptualization (equal), Data curation (supporting), Formal analysis (equal), Investigation (supporting), Methodology (equal), Project administration (supporting), Resources (equal), Software (equal), Writing – original draft (supporting), Writing – review & editing (equal); Faith Orchard: Conceptualization (equal), Data curation (supporting), Formal analysis (equal), Investigation (equal), Methodology (equal), Project administration (supporting), Resources (equal), Software (equal), Writing – original draft (supporting), Writing – review & editing (equal); Ray Percy: Project administration (supporting), Resources (supporting), Software (supporting), Writing – review & editing (supporting)
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Competing interests
P.W. (Postdoctoral Research Fellowship; PDF-2016-09-092) is funded by the National Institute for Health Research (NIHR). The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care. Olivia Sukiennik undertook this paper as part of a Master’s degree when at the University of Reading.
Ethical standards
Authors have abided by the Ethical Principles of Psychologists and Code of Conduct as set out by the BABCP and BPS. Permission to use routine clinical information for research purposes was provided by the Clinical Audit Department of the Berkshire Healthcare NHS Foundation Trust. This study was classified as a service evaluation because it (i) evaluated current treatments being delivered within routine services, (ii) measured current service without reference to a standard, (iii) did not involve randomisation to treatment, and (iv) involved the analysis of existing data (Health Research Authority, 2016).






Comments
No Comments have been published for this article.