INTRODUCTION
Atrial fibrillation (AF) is the most common arrhythmia with prevalence approaching up to 10% of people over the age of 65 years.Reference January, Wann and Alpert 1 AF is associated with an increased risk of stroke, heart failure, and all-cause mortality.Reference Stewart, Hart and Hole 2 Although AF is rarely life-threatening and not usually an emergent condition, presentation to the emergency department (ED) is common and accounts for one-third of hospitalizations for cardiac arrhythmias.Reference Verma, Cairns and Mitchell 3 , Reference Fuster, Ryden and Cannom 4 In Ontario (population approximately 12 million), there were 56,413 visits to the ED for a primary diagnosis of AF between January 2007 and December 2009.Reference Barrett, Vermeulen and Self 5 Hospital admissions for AF have increased by over 65% in the last 20 years and are expected to continue rising.Reference Friberg, Buch and Scharling 6 , Reference Wattigney, Mensah and Croft 7
The most recent updated Canadian Cardiovascular Society guidelines to make specific recommendations on the management of recent onset AF in the ED were published in 2014.Reference Verma, Cairns and Mitchell 3 The guidelines do suggest that there are “two competing strategies for ED management”: rate and rhythm control.Reference Verma, Cairns and Mitchell 3 To our knowledge, no randomized trials on the management of recent onset AF in the ED setting have been published.Reference Stiell, Healey and Cairns 8 Rate versus rhythm control has been explored in the general AF population in both the AFFIRM and AF congestive heart failure clinical trials. However, in those studies, it was found that rhythm control was not superior to rate control.Reference Wyse, Waldo and DiMarco 9 , Reference Roy, Talajic and Nattel 10 In the ED, it has been suggested that patients with recent onset AF should receive a trial of rhythm control and that this strategy could prevent hospital admissions and “bouncebacks.”Reference Michael, Stiell and Agarwal 11 , Reference Stiell, Clement and Perry 12 Studies have demonstrated, however, that a rhythm control strategy could lead to more ED return visits, as compared to a rate control strategy (52% v. 45%, respectively).Reference Scheuermeyer, Grafstein and Stenstrom 13 Stiell et al. examined this patient population in a Canadian cohort in 2011 and in 2017.Reference Stiell, Clement and Brison 14 , Reference Stiell, Clement and Rowe 15 Their results suggest that a rhythm control strategy is safe and that cardioversion rates in some institutions are high. Other data (from the RELY registry, which has not yet been published), however, suggest that worldwide cardioversion rates are lower, and we hypothesized that there was substantial interhospital variability within Canada as well.Reference Barrett, Vermeulen and Self 5
There are diverse trajectories possible in patients with AF, including spontaneous or treatment-induced reversion to sinus rhythm, rate slowing after treatment, and admission or discharge. The objective of this study was to describe current practices in the management of AF in the ED. We sought to characterize factors influencing the decision to proceed with a rhythm control strategy.
METHODS
Patients were identified using administrative data. The National Ambulatory Care Reporting System (NACRS) contains a record of every patient who presents to the ED in Ontario, including the primary reason for presentation as assessed by the ED physician. The International Classification of Diseases, 10th Revision (ICD-10), code for AF (I-480) has been previously validated in NACRS (positive predictive value of 93.0% [95% confidence interval, CI, 91.6% to 94.2%]; sensitivity, 96.6% [95% CI 94.1% to 98.2%]).Reference Atzema, Lam and Young 16 There were four academic hospitals, defined as hospitals with a direct affiliation with a university, and six community-based hospitals (three urban and three suburban) included in the study. From January 1 to December 31, 2010, across 10 Toronto hospital EDs, every patient with a primary diagnosis of AF or atrial flutter (AFL) was identified from the NACRS database. Patients were included if they were ≥18 years of age with a manually verified 12-lead electrocardiogram (ECG) confirming AF or AFL. From the list of eligible patients in each hospital, 50 patient charts were randomly selected from among the total, using a random selection program that was programmed by our statistician. For patients with more than one visit, only the first visit was selected for abstraction. Data abstraction was performed by a research assistant who was trained by the senior author of this manuscript.
Patient demographics, medical history, pre-presentation medication use, and details of ED treatment and outcome were recorded. Patient disposition (admitted or discharged) was recorded. Patients were classified according to the primary management strategy. The rhythm control group included any patient who received any antiarrhythmic drug (AAD) or electrical cardioversion, with or without rate control. AAD therapy was defined as the administration of any of procainamide, flecainide, propafenone, sotalol, amiodarone, and dronedarone by any route. Electrical cardioversion included patients with shocks delivered, with or without prior antiarrhythmic therapy. The rate control included any patient receiving a beta-blocker, calcium channel blocker, or digoxin in the ED, who did not receive any form of rhythm control.
STATISTICAL ANALYSIS
Continuous data are expressed in means + / - standard deviation and compared using the Student’s t-test. Categorical variables are expressed in frequencies and percentages and compared by the chi-square test or the Fisher exact test if expected cell counts were less than 5. A p value of <0.1 in a univariate model was considered for entry into the main model. We used hierarchical regression modelling where potential confounding variables, such as age and sex, were included in the model first followed by clinical variables. The model was assessed following the inclusion of all variables with general likelihood ratio testing because there were variables that were not statistically significant in the model. The removal of these variables, however, did not improve the model; thus, they remained in it. The Hosmer–Lemeshow test was used to assess the goodness of fit of the final specified multivariate model (p=0.818). Discriminability was measured using the area under the curve where the C-statistic was 0.836. Multivariate logistic regression was conducted using select demographic and ED factors to evaluate potential associations with a rhythm control strategy. These factors included age, sex, systolic and diastolic blood pressure, initial ventricular rate, symptoms of palpitations (≤48, >48 hours), symptoms of chest pain, dyspnea, syncope, fatigue, prior ED visit for AF, CHADS2 score (0, 1-2, >2), heart failure, prior warfarin therapy, history of valvular heart disease, prior valvular surgery, coronary artery disease, prior myocardial infarction, prior stroke, prior transient ischemic attack, implantable pacemaker, sleep apnea, smoking, dementia/cognitive deficit, prior coronary artery bypass grafting or percutaneous coronary intervention, chronic obstructive pulmonary disease/emphysema, prior major bleed, substance abuse, international normalized ratio (INR) > 2, elevated troponins, weekend or weekday visit, and time of day (0801 to 1600, 1601 to 2400, 2401 to 0800 hours). Discriminability was assessed by the receiver operator curve, and multicollinearity was evaluated using the variance inflation factor. Odds ratios (OR) with 95% CIs and p-values are reported where p<0.05 is considered statistically significant. All data were analysed using SPSS, version 22.0 (IBM Corp., Armonk, NY, USA).
RESULTS
In the random sample of 500 patients, 233 patients (47%) received rate control, 129 (26%) received rhythm control (with or without rate control), and 138 (28%) did not receive either therapy (Table 1). No patients were excluded from the 500 patients randomized to the study protocol. All of the 500 patients had a primary diagnosis of AF, and at least one 12 lead ECG with AF. Sixty-nine patients (14%) received an AAD alone, and 82 (16%) received electrical cardioversion. Of those receiving a rhythm control strategy, 64% had an electrical cardioversion (with or without an AAD), 47% had cardioversion only, and 36% received an AAD alone.
Table 1 Baseline characteristics
Data expressed in frequency (percent) or mean±standard deviation.
* Total patient count. The sum of the individual drugs does not equal this because some patients received multiple agents.
† This number is calculated from those whom an ECG was available (n=84 in rate control group, n=97 in rhythm control group, and n=57 in the no treatment group). Note: Not all patients had discharge ECGs available.
‡ This number is calculated from those whom HR was available (n=147 in rate control group, n=115 in rhythm control group, and n=73 in no treatment group). Note: Not all patients had posttreatment HRs available.
The most commonly used rate control therapy was with a calcium-channel blocker (60%) followed by beta-blocker therapy (55%). Eleven percent of patients received digoxin.
Patients receiving either rate control or no treatment were older than those receiving rhythm control (71±13 v. 60±15.4 years; p<0.001). The majority of patients not receiving rhythm control were female (62% rate control and 53% no treatment, respectively), whereas, in the rhythm control group, the majority were male (57%). Patients undergoing rhythm control were more likely to be symptomatic (88%) as compared to the rate control group or no treatment group (59% and 51%, respectively).
In the entire cohort, 67% were discharged home from the ED; the range of admission rates amongst the 10 hospitals was 14% to 50%. Discharged patients were more likely to have received rate control or no therapy than rhythm control (68% no rhythm control v. 32% rhythm control; p<0.0001; Figure 1).
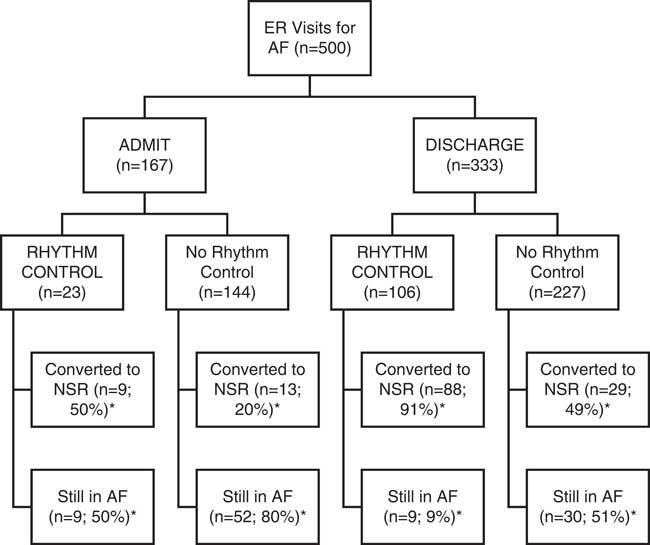
Figure 1 Treatment and disposition decisions.* Note: these values reflect the proportion of patients where ECGs were available at discharge.
Two hundred thirty-eight patients had an ECG available posttreatment prior to ED disposition. Of those discharged from the ED having received no rhythm control strategy, 141 had an ECG available and 51% of those converted to normal sinus rhythm prior to discharge, whereas 49% remained in AF (see Figure 1). Of those discharged using a rhythm control strategy, 97 had an ECG available and 91% were discharged in normal sinus rhythm (see Figure 1). The type of hospital (academic v. community) did not influence the treatment decision (rate v. rhythm) or admission rates (Table 2), although interhospital treatment differences were seen. These variabilities in admission rates and treatment decisions could not be explained by the type of hospital alone; further study would be required to elucidate the specific etiology amongst each individual hospital.
Table 2 Interhospital treatment variability
A multivariate regression model was used to evaluate demographic and clinically plausible predictors of a rhythm control strategy (Table 3). Of these factors, age in years (OR: 0.96; 95% CI: 0.94-0.98; p<0.0001), new onset palpitations ≤ 48 hours compared to asymptomatic (OR: 5.5; 95% CI: 2.8-10.7; p<0.0001), a CHADS2 score of 1-2 compared to a CHADS2 score of 0 (OR: 3.3; 95% CI: 1.3-8.8; p=0.015), and normal LV function compared to LV dysfunction (OR: 8.2; 95% CI: 1.8-36.8; p=0.006) significantly predicted treatment with a rhythm control strategy in an adjusted model.
Table 3 Predictors of rhythm control strategy: multivariate logistic regression
The regression model suggests that a recent onset of symptoms (< 48 hours) is a predictor of rhythm control in patients who are candidates for cardioversion. However, these patients were more likely to receive rate control or no therapy than rhythm control (59% v. 41%, p<0.0001; Table 4). Similarly, patients who were anticoagulated with an oral anticoagulant at the time of presentation were more likely to receive rate control or no therapy (82% v. 18%, p<0.0001; Table 4).
Table 4 Patients eligible for a rhythm control strategy
DISCUSSION
Our data suggest that there are a wide range of practices between sites within the same geographic region treating patients presenting to the ED with AF. In urban, suburban, and academic teaching hospitals in a large Canadian city, the minority of patients presenting to the ED with AF receive rhythm control management, even amongst those already anticoagulated (who can safely be cardioverted regardless of AF duration) or those with recent onset of symptoms.
There have been conflicting reports previously published as to the most common practice with respect to management of recent onset of AF in the ED. Prior observational studies in selected EDs in Canada have suggested that rhythm control is the most commonly used management strategy for recent onset of AF.Reference Stiell, Healey and Cairns 8 Rhythm control, usually with intravenous procainamide and/or electrical cardioversion, had a reported use in 66% of patients with recent onset of AF.Reference Rogenstein, Kelly and Mason 17 Rhythm control is undertaken to rapidly improve symptoms, shorten ED length of stay, with the expectation that patients can then be discharged home safely once they are in a normal sinus rhythm.Reference Stiell, Healey and Cairns 8 Other published observational studies found that cardioversion in Canada was less common, which is similar to our findings.Reference Barrett, Vermeulen and Self 5 , Reference Atzema, Dorian and Ivers 18 Barrett et al. found that only 10% of patients in the ED received cardioversion in Canada compared to 5% in the United States.Reference Barrett, Vermeulen and Self 5 In another retrospective study evaluating the practice in Ontario, Atzema et al. found that only 7% (of 12,772) of all patients with AF in the ED underwent cardioversion.Reference Atzema, Dorian and Ivers 18 In contrast, a retrospective review of an observational cohort of Canadian practice regarding a recent onset of AF, Stiell et al. found that rhythm control was the predominant strategy with 60% of ED physicians attempting rhythm control, either pharmacologic or electrical.Reference Stiell, Clement and Brison 14 Furthermore, their group found that 83% of patients presenting with recent-onset AF were discharged home.Reference Stiell, Clement and Brison 14
The reason for these different observations is not clear. Scheuermeyer et al. described a cohort of patients from two urban EDs from 2006 to 2010, and Stiell et al. described a cohort of patients from eight different EDs across Canada in 2008.Reference Scheuermeyer, Grafstein and Stenstrom 13 , Reference Stiell, Clement and Brison 14 Scheuermeyer’s cohort had a median age of 65 years with 63% male patients, and the majority had documented a previous AF.Reference Scheuermeyer, Grafstein and Stenstrom 13 Similarly, Stiell’s cohort had a median age of 65 years with 57% male patients and again the majority had a previous AF.Reference Stiell, Clement and Brison 14 Scheuermeyer et al. found that patients who underwent electrocardioversion or chemical cardioversion appeared to be younger, had shorter preceding arrhythmia duration, had fewer cardiovascular risk factors, and had lower CHADS2 scores than those who did not undergo rhythm control.Reference Scheuermeyer, Grafstein and Stenstrom 13 Stiell et al. found geographic differences in the use of rhythm and rate controls. Other predictors in his cohort of rhythm control included age, previous cardioversion, and associated heart failure.Reference Stiell, Clement and Brison 14 These data together with our data suggest that there is a substantial difference in practice in different settings.
Our data showed that young, low risk patients (CHADS2 1-2) with no LV dysfunction and new onset symptoms (palpitations<48 hours) were the patients who were most likely to receive a rhythm control strategy. This is not surprising based on the risk profile of AAD therapy. Elderly patients who have multiple comorbid conditions are more likely to have complications from AAD therapy, and hence this population is expected to be more likely to receive a conservative approach. Patients with new onset symptoms are more likely to be successfully treated with rhythm control. Furthermore, they are more likely to remain in sinus rhythm than patients who have had long-standing AF.
Rate control may have been more common in this cohort due to its ease of use and limited risk. Moreover, the administration of an AAD must be monitored more closely than rate control and has the potential for more serious adverse effects. Finally, there is a lack of evidence to suggest that one strategy leads to improved morbidity or better quality of life, although it seems reasonable to suppose that prompt restoration of sinus rhythm would lead to better short-term symptom relief than a rate control strategy.
There are limited data that have evaluated long-term outcomes (readmissions, stroke rates, or quality of life) in patients discharged in a normal sinus rhythm as compared to those discharged with AF. In the FinCV (Finnish CardoVersion) Trial, 7,660 cardioversions were performed in acute AF, and the short-term risk (<30 days) of thromboembolic complications was low (<1%).Reference Airaksinen, Gronberg and Nuotio 19 More recently, in a Canadian cohort, Stiell et al. showed that there were few serious complications in the short-term (< 30 days) following cardioversion for recent-onset AF and AFL.Reference Stiell, Clement and Rowe 15 There was 1 stroke in their cohort (0.1%) of 1,091 patientsReference Stiell, Clement and Rowe 15 ; 15% of patients returned to the ED for AF or AFL within 30 days with 6.5% requiring a subsequent cardioversion and 3.3% requiring hospitalization.Reference Stiell, Clement and Rowe 15 Although not a randomized comparison, these data suggest that a rhythm control strategy is safe. In a follow-up study of patients treated in the ED with a strategy of rate or rhythm control, 52% of those who underwent electrical cardioversion, 50% of those who received pharmacologic cardioversion, and 45% of those who underwent rate control had a repeat ED visit within the subsequent year,Reference Scheuermeyer, Grafstein and Stenstrom 13 suggesting that an aggressive rhythm control strategy may be associated with frequent recurrences requiring acute medical care. There may be a trade-off between accepting a higher risk of ED readmission and a likely superior relief of AF symptoms. The knowledge that most patients with symptomatic AF convert spontaneously may encourage both the physician and the patient to undertake a conservative strategy with discharge, regardless of their rhythm at discharge.Reference Cotter, Blatt and Kaluski 20 It is possible that patients treated with a rate control strategy may be more likely to follow up with their physicians and use a long-term management plan, because they may be less likely to be under a false belief that they have been “cured.” Higher rates of discharge in sinus rhythm are associated with increased rates of recurrent AF, resulting in subsequent ED visits.Reference Scheuermeyer, Grafstein and Stenstrom 13 This knowledge, with the ease of administration and a long-standing safety profile, likely drives the use of rate-control as the predominant strategy.
Limitations of this study include that it was a retrospective analysis. It is unclear what, if any, other biases may have contributed to the pathways that were undertaken. Both patient wishes and physician biases were not accounted for in our analysis. The random sample of 50 patients was not weighted by hospital size. We opted to group the patients based on their initial treatment strategy as opposed to their outcome, because we wanted to examine the decision process and predictors in management. Many patients who were treated with any strategy (including no treatment or rate control) converted to sinus rhythm. Some patients may have been intended to be treated with a rhythm control strategy but converted to sinus rhythm before the treatment could be instituted. The percentage of patients who converted to sinus rhythm was obtained from less than half of the original sample because only 48% of patients had ECGs available posttreatment.
CONCLUSIONS
Our data suggest a substantial practice variation in treating patients presenting to the ED with AF. The minority of patients received rhythm control. Young patients with normal LV function and new onset of symptoms were the patients who were most likely to receive a rhythm control strategy. Randomized studies are required to elucidate the optimal strategy in the management of this patient population.
Competing interests: This study was supported by an unrestricted educational grant from Sanofi, Inc.; and PD received research support and honoraria from Bayer, BI, BMS, Pfizer, Sanofi.







