The “gut-mind axis” is experiencing a renaissance. The past decades have seen the publication of numerous studies of the dynamic relationship between digestive and psychological health, adding to an expanding body of research that shows little sign of slowing.Footnote 1 One of the most striking findings to have emerged from this research is that many of the body's most important neurotransmitters are produced and maintained by trillions of microbes residing in the gastrointestinal tract.Footnote 2 A study published in 2000 estimated that around 95 percent of the body's serotonin—the neurochemical targeted by the class of commonly prescribed antidepressant medications that includes Prozac, Zoloft, and Lexapro—resides in the small intestine, facilitating multidirectional communication between the digestive tract and the central nervous system.Footnote 3 Digestion, then, exercises a significant influence over cognitive processes and plays a vital role in regulating patterns of mood and behavior. Once considered metaphorical, the “gut feeling” is now a medical reality.
Historians, however, have been quick to point out that the idea of a gut-mind connection is far from new. Many older medical systems, as Ian Miller observes, “readily incorporated understandings of relations between gut, mind and emotions using the ascendant medical models of their time.”Footnote 4 In premodern Europe, the belly and the brain were understood to be engaged in constant and intimate commerce with one another, and emotional well-being was believed to be crucially dependent upon the health of the gut. As Gail Kern Paster and Michael Schoenfeldt have shown, the doctrine of the four humors—the dominant system of medical theory in in late medieval and early modern Europe dating back at least to Greek antiquity—gave the stomach and digestive organs a position of crucial importance in the governance and mediation of the passions.Footnote 5 David Hillman has argued that the “corporeal interior” was perceived as “the central locus of consciousness, emotion and transcendent meaning” in early modern English literary culture.Footnote 6 More recently, Jan Purnis, inspired by contemporary neurobiological accounts of the enteric nervous system, has suggested that the humoral notion of “a belly that is especially thoughtful, seemingly with the capacity to think and reason on its own,” offers an important corrective to linear narratives of scientific progress.Footnote 7
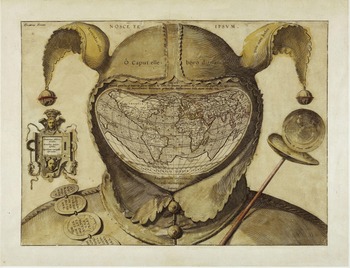
But while these studies have contributed much to our understanding of how the early modern gut-mind axis shaped the language of feeling in Renaissance literature, comparatively little attention has been paid to how this “embowelled” view of emotion shaped the way that diseases of the mind were understood, diagnosed, and treated in the domain of practical medicine.Footnote 8 To address this omission, this article presents a close study of hellebore, a violent purgative drug historically associated with mental illness. In early modern Europe, a medical prescription of hellebore carried immediate and powerful significance. Since ancient times, it was implicitly understood that to be given hellebore was to be declared mad and therefore beyond the power of most ordinary medicines. The Latin idiom “O caput elleboro dignum” (O head, worthy of hellebore) attained proverbial status in sixteenth- and seventeenth-century Europe, and the plant's near-miraculous virtues in cases of mental illness were documented by some of the most influential medical writers of the age.Footnote 9 A woodcut of hellebore appeared on the frontispiece of Robert Burton's Anatomy of Melancholy, which placed it among “The best medicines that e'er God made / For this malady, if well assay'd . . . a most renowned plant, and famous purger of melancholy.”Footnote 10 Even Paracelsus, a highly vocal and vitriolic critic of humoral medicine, was effusive in his praise of hellebore, writing, “There is more to be found in this one herb, then is to be found in all the writings of university doctors . . . That doctor who knows the right use . . . shall by this one herb have more infallible knowledge and skill in curing diseases, then all the empericks or doctors whosoever.”Footnote 11
Despite being extensively praised, prescribed, and purchased in its time, hellebore has received comparatively little attention in ours from historians of medicine.Footnote 12 With the decline of humoral medicine in the eighteenth and nineteenth centuries, the plant came to be seen by the medical establishment as less of a wonder drug than a professional embarrassment. In 1801, when Philippe Pinel reflected on the “helleborism” of the Greek medical tradition, he dismissed it as nothing more than “narrow-minded empiricism,” unworthy of the attention of modern doctors of the mind. Pinel poured scorn on his intellectual forebears, incredulous that such “popular prejudices or superstitious ideas . . . were [ever] subjects of serious discussion.”Footnote 13 The picture he painted of premodern medicine was damning: generations of physicians diligently laboring to make the remedies of the ancients actually work—or at the very least, to minimize their potential for harm—and, increasingly, to distance their practices from what was considered the primitive natural magic in which they were rooted. This tendency to view the medical past as a story of linear progress has contributed to the comparative historiographical neglect of discredited remedies like hellebore, which at best have been held up as colorful examples of what not to do. As the physician-turned-historian Guido Majno wrote in 1975, “Hellebore alone could claim a long chapter in the history of human error . . . One might as well shoot a gun blindly in order to enjoy the noise and the smell . . . The saving grace of hellebore was that it caused vomiting so fast that the patient stood a chance of getting rid of it before absorbing a lethal dose.”Footnote 14 Hellebore emerges from these accounts as just another toxic substance in a vast and largely arbitrary premodern pharmacopoeia. On the surface, it appears to confirm what we might think we already know: that medicine in the past could be incomprehensibly cruel, and that all-encompassing, overly simplistic theories were often carried to fatal extremes.
The past decade, however, has seen a noticeable increase in studies of the cultural significance of medicinal substances across the early modern world, as historians have begun to recognize that even discredited or “dangerous drugs” can offer valuable insights into the cultural milieux in which they were used.Footnote 15 He Bian, for instance, has drawn upon the bencao pharmacological tradition to offer a new perspective on processes of cultural change in early modern China, while Benjamin Breen has shown how the circulation and consumption of drugs in early modernity can be used to reveal “a larger fabric of social relations, cultural practices, and that deep reservoir of unstated beliefs about how the world functions.”Footnote 16 At the same time, there has been a concerted attempt to reclaim the study of plants and herbal medicine as a meaningful subject of historical, ethnographic, and phenomenological inquiry.Footnote 17 Ethnobotany has grown into an active, vibrant anthropological subdiscipline, while the new field of critical plant studies has brought together philosophers, literary scholars, and cultural critics to explore the interface of the human and vegetable worlds.Footnote 18 It is now widely recognized that the beliefs and practices that cluster around plants are always imbued with wider cultural significations, which in turn shape the ways in which they are perceived to act upon human bodies. Plant-based medicines, as Elisabeth Hsu observes, are “cultural artefacts that are produced and used in culture-specific ways,” warranting the same degree of critical analysis as other areas of social and material life.Footnote 19
Approaching dangerous drugs like hellebore seriously as a subject of historical inquiry is not the same as advocating for or defending their use in the present day. Hellebore contains the toxic compound protoanemonin, which if ingested by humans, causes “vomiting, inflammation of the mouth and throat, [and] abdominal pain that can be followed by severe ulcerations of the mouth and damage to the digestive and urinary systems,” and can even be fatal.Footnote 20 These effects alone are reason enough to be thankful that it has fallen out of use as a treatment for mental illness.Footnote 21 But in light of the current historical, anthropological, and philosophical interest in the relationship between mind and gut, it is worth considering what this centuries-old medical practice can tell us about past conceptions of embodied emotion and how seemingly nonmedical beliefs could find expression in the domain of practical therapeutics. I suggest that, far from illustrating little more than the ignorance and brutality of practitioners, the use of hellebore to treat mental illness offers graphic and visceral evidence of the interconnectedness of digestion and emotion that has been ascribed a “defining role in [the] emotional life” of early modern Europe.Footnote 22 Drawing on a wide range of sources, from physicians’ case histories and manuscript recipe books to works of medical and religious polemic, I show that the popular image of hellebore was shaped by accounts and descriptions that not only acknowledged the violence of its internal action within the body but portrayed these potentially life-threatening properties as crucial to its capacity to cure mental illness. I also show how the use of hellebore in exorcisms and other ritualistic hygienic practices suggests a deeper and more pervasive link to both spiritual and magical conceptions of emotion than has previously been recognized, a qualitative association that depended upon widespread awareness of the plant's violent expulsive properties.
Despite claims to the contrary by some contemporary medical writers, hellebore remained in widespread use in Britain throughout the seventeenth and early eighteenth centuries and was strongly associated with the treatment of mental illness throughout the period under discussion. Successive physiological theories continued to justify hellebore's use, and while many feared the violence of its operation, few argued that it was ineffective in treating sicknesses of the mind. Indeed, assumptions about the therapeutic potency of hellebore were inseparably tied to its reputation as a dangerous poison and the perceived violence of its laxative action. As my exploration of the metaphorical and symbolic use of hellebore in seventeenth-century polemic shows, its use as an insult harnessed the plant's reputation as a cure for madness whose operation was seen as both violent and grossly physical. Sensory descriptions of hellebore reinforced its association with the tactile qualities of the melancholy humor (black bile), which was accorded a central role in the pathology of emotional distress. Indeed, the clear parallels between medical accounts of successful hellebore cures and exorcistic rituals suggest that in both medical and demonological narratives, the moment of the “cure” was routinely signaled by the expulsion of large quantities of black matter from the belly and bowels. Drawing these strands together reveals a worldview in which morality, emotion, and digestion become practically indistinguishable. Far from being a trivial piece of herbal folklore, then, the story of hellebore offers a surprisingly vivid account of the emotional life of early modern Europe.
Purging the Passions
On 26 May in an unspecified year during the 1680s, the royal physician Edmund King attended a case of mental illness. His patient, Lady Betty Thomond, had “[fallen] into a violent passion” and was resisting treatment. Finding her “raving extremely” and “fearful that she would fall into a furor uterinus or mania,” King prescribed a course of vomits and purges, but this brought no relief. Over the next fortnight, Lady Thomond was subjected to a range of therapies, including warm baths, cordial waters, leeches, and enemas. But by 10 June, her condition was “worse and more raving than ever,” and King decided it was time to up his game. He took away his patient's feather bed and applied sheep's lungs to her head, to no effect. Lady Thomond's condition continued to deteriorate, and she showed only fleeting “sparks of sense.” Finally, despairing of any other cure, King prescribed a purge of black hellebore. Two weeks later, he found her in “good pulse and good temper.” By late July, after continuing her course of daily purges and vomits for a full month, she had “recovered very well.”Footnote 23
King was not alone in prescribing hellebore to the chronically low-spirited, and the account of Lady Betty Thomond, while unusually detailed, is just one of many similar examples recorded in early modern medical case histories.Footnote 24 For instance, when Leonard Kempson of Stratford-upon-Avon became “oppressed with melancholy” in the early seventeenth century, he sought medical advice from John Hall, a physician and the son-in-law of William Shakespeare. Hall administered an enema of black hellebore, which “brought away two Stools with a great deal of Wind.” After this treatment had been repeated several times, Hall reported, Kempson “became well, bidding farewell to Physick, and so was cured beyond all expectation, and lived for many years.”Footnote 25 When the astrological physician Richard Napier was called upon to treat the fifteen-year-old Eleanor Astone, who had become “lightheaded and very lunatic” and was suffering from fits of rage in which she would scream at and scratch her mother, his response was brisk and unequivocal: “Purge with blacke hellebor.”Footnote 26 Napier also prescribed hellebore to the forty-year-old Robert Day, who had fallen “mad out of his wits” due to unpaid debts; he also gave it gratis to the suicidal William Rogers, whom he judged to be “full of black melancholy.”Footnote 27 From 1597 to his death in 1634, Napier purged hundreds of his disturbed, distressed, and depressed patients with hiera logadii, a medicinal compound whose principal active ingredient was the root of black hellebore.Footnote 28
While case histories attest to how frequently hellebore was deployed by licensed physicians, domestic receipt books offer an eclectic array of practical advice on how to harness hellebore's mind-altering properties for oneself.Footnote 29 An early seventeenth-century collection of medical recipes attributed to one “Mrs Corlyon,” for instance, explained how to make “Good pils to purg Melancholy” from “roots of true black Helleborus,” while an anonymous medical miscellany from around 1634 offered guidance on how to administer the plant to those suffering from “Hystericks or Melancholy.”Footnote 30 The alchemical receipt book of Margaret Baker offered the following instructions for preparing a laxative medicine: “[Take] ye rootes of ellibur, slice them & putt them in an apple, and lett it stand all day . . . at night, rost it, then take the roots away & eate the apple & this will purge.”Footnote 31 This recipe was apparently widely known and well-regarded; in the early eighteenth century, the noted Edinburgh physician Archibald Pitcairne advised madhouse doctors to “let the Hellebore-Apple be used” in extreme cases; he recorded in his handwritten notes that the “root of the black hellebore, given cautiously, has vast effects in lunacy, epilepsy, madness &c.”Footnote 32
The potency of hellebore in cases of mental illness was thought to depend primarily upon its powerful laxative and emetic properties. Within the explanatory framework of early modern medicine, good health depended upon maintaining the body in a perpetual state of solubility, and serious illnesses of all kinds could arise from some form of obstruction or blockage of the body's humoral flow.Footnote 33 Many living in this time were thus haunted by a chronic anxiety about the state of their digestive interior, which Shigehisa Kuriyama has termed a “forgotten fear of excrement”; the result was an approach to practical therapeutics in which, as Barbara Duden puts it, “to purge oneself, to cleanse oneself, to loosen threatening stagnation by evacuation [was] paramount to both patient and physician.”Footnote 34 The practice of therapeutic purgation has a deep global history and continues to shape the ways in which people across the world perceive and act upon their bodies in the present day.Footnote 35 For many, however, it has become a largely figurative, disembodied process having little to do with actual bodily secretions and even less to do with digestion and the gut. Twenty-first-century English speakers deploy the “hydraulic model of emotions” on a regular basis, whether “letting off steam,” “bottling up their feelings,” or seeking the elusive state of “flow.”Footnote 36 The concept of catharsis—from the Greek katharsis, “to purify, purge”—continues to inform the practice of talking therapy by shaping the narrative within which the psychological breakthrough is constructed.Footnote 37 But any twenty-first-century psychiatrist who prescribed laxative medications as a primary treatment for mental illness would likely face professional ridicule and perhaps even suspension from practice.
In early modern Europe, by contrast, medical practitioners’ professional reputations could hinge upon their ability to provoke strong purges, the standard recourse for physicians confronted with debilitating passions in their patients.Footnote 38 Hellebore was the purgative remedy par excellence, scouring the body of corrupted matter and producing a blackened fecal discharge: tangible, noxious evidence of its therapeutic action.Footnote 39 Such was the power of its operation—its ability to reach into the hidden recesses of the body and draw out offensive matter—that it was thought to be an especially effective treatment for diseases whose origins were mysterious or remote: madness, migraines, convulsions, intestinal worms, and various internal or constitutional complaints.Footnote 40 A successful cure was evidenced by a forceful evacuation of the patient's stomach and bowels, after which their psychological symptoms were reported to have abated.
Purges of hellebore were a staple of ancient Greek medicine, and early modern Europeans acquired the practice from medieval Arabic sources, along with a vast and multifaceted corpus of medical knowledge.Footnote 41 The popular and much-reprinted Hippocratic Aphorisms instructed physicians to “purge melancholicke folke strongly by stoole,” and specifically appointed hellebore to be used for this purpose.Footnote 42 In a short treatise titled De Atra Bile (On Black Bile), written in the second century AD, the Greco-Roman physician Galen remarked that “this purge has been highly regarded, not just in the past two or three centuries, but also many more years back, and in the meantime everyone has used it as a drug.”Footnote 43 While Arabic physicians continued to make use of hellebore, their praise became somewhat more qualified, often evincing a preference for milder purgatives such as senna.Footnote 44 A highly influential medieval pharmacological work, purportedly authored in the ninth century by Yuḥannā ibn Māsawayh (Latinized as “Mesue”) recommended hellebore's use only in extreme cases, including “stubborn and persistent melancholy affections.”Footnote 45
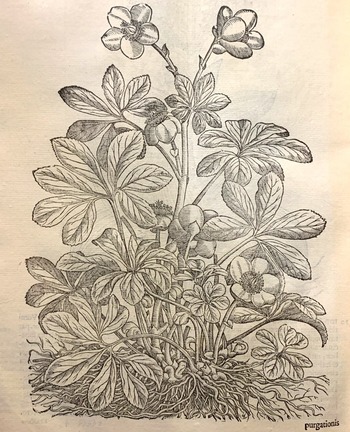
The revival of Greek learning in European medical faculties brought with it a renewed interest in remedies favored by the ancients. Over the course of the sixteenth century, the goal of providing more accurate translations of the Greek materia medica gave way to the even more ambitious project of refining and expanding upon an already sizable body of botanical knowledge.Footnote 46 As a result, from around the middle of the century, weighty and lavishly illustrated volumes of plant lore known as herbals—such as Pietro Andrea Mattioli's Commentaries on the Materia Medica of Pedanius Dioscorides (figure 1)—began to be printed in increasingly large numbers across continental Europe, providing detailed descriptions of the therapeutic virtues of plants within the framework of humoral physiology.Footnote 47 In the case of hellebore, these descriptions invariably emphasized both its psychosomatic properties and its powerful laxative or emetic action. “A purgation of Hellebor,” stated John Gerard's Herball, “is good for mad and furious men, for melancholy, dull, and heauy persons . . . [and] for all those that are troubled with blacke choler, and molested with melancholy.”Footnote 48 Humoral pharmacology classified hellebore as a “melanagogue”—a substance possessing a special affinity with melancholy (from the Greek μελαγχολία, literally “black bile”), a dark, viscous, and foul-smelling bodily fluid thought to be produced in the spleen.Footnote 49 Many pathological mental illnesses were believed to result from a disordered spleen producing an excess of black bile that flooded into the stomach, sending up fumes through the alimentary canal to “darken the mind, and over-cloud the brain.”Footnote 50 Hellebore's perceived ability to drive away sadness and sharpen the wits thus depended crucially upon its reputation for producing forcible evacuations of the stomach and intestines.

Figure 1 Woodcut of hellebore from Pietro Andrea Mattioli's Commentaries on the Materia Medica of Pedanius Dioscorides (Venice, 1565), Folger call no. 229–916f, 1p. 220. Photograph by Michael Walkden, reproduced by permission of the Folger Shakespeare Library.
From around the beginning of the seventeenth century, however, an influx of new medicines and competing systems of physiology began to pose fundamental challenges to the hegemony of humoral theory. Drawing on medieval occultism and the trade secrets of distillers, metallurgists, and folk healers, the “chemical” medicine spearheaded by Paracelsus in the sixteenth century introduced a host of new mineral and metallic substances into the physician's arsenal.Footnote 51 At the same time, new purgative plants from the Americas such as jalap, mechoacan, and tobacco—their operations somewhat gentler and more controllable than those of hellebore—were rapidly becoming mainstays in the treatment of mental illness, as both Richard Napier's and Edmund King's extensive practice notes reveal.Footnote 52 The second half of the seventeenth century, moreover, witnessed the emergence of a new physiology that emphasized the nerves and fibers of the body, marking a shift in the medical gaze “from attention to fluid somatic stirrings to ‘solidar pathology.’”Footnote 53 In light of these changes, we might reasonably expect to see a decline in the use of hellebore in the practical treatment of mental illness. And indeed, early in the seventeenth century, the German physician Daniel Sennert claimed that hellebore had been largely supplanted by chemical remedies such as mercury and antimony, while in 1685 the chemist Georg Wolfgang Wedel listed black hellebore in his catalogue of medicinal substances under the heading “Seldom Used” and white under “Never Used.”Footnote 54
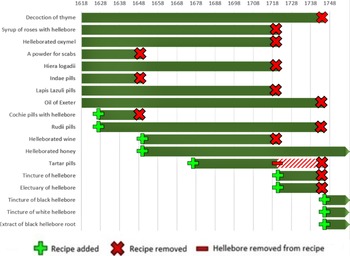
Yet the evidence from practice suggests that hellebore remained in active and widespread use in Britain until at least the middle of the eighteenth century. Rather than being displaced by mineral and metallic substances that were among the key practical innovations of chemical medicine, it was readily incorporated into new chemical compounds alongside these ingredients. The celebrated (and censured) Mathews’ Pills, for instance, combined both white and black hellebore with opium, saltpeter, and oil of amber.Footnote 55 An anonymous apothecary's cash book from the West Riding of Yorkshire recorded fourteen payments for hellebore and close to forty for Mathews’ Pills between 1703 and 1710, including prescriptions for patients suffering from dizziness, epileptic fits, and melancholy.Footnote 56 The Sussex apothecary Nicholas Gaynsford continued to draw up recipes containing hellebore in the 1710s, while the Londoner Thomas Corbyn was recording it in his inventories as late as 1773.Footnote 57 Recipes containing hellebore also continued to be listed in the College of Physicians’ published catalogue of medical compositions until around the middle of the eighteenth century, with a handful enduring longer still.Footnote 58 Although it is difficult to judge how often or how far these guidelines were followed in practice, they appear to suggest that the decline of hellebore in practical medicine did not begin until at least the eighteenth century; by 1745, the number of compounds in the Pharmacopoeia that included hellebore had fallen to just four—down from eight in the original 1618 edition, and as many as ten between 1627 and 1650 (figure 2).
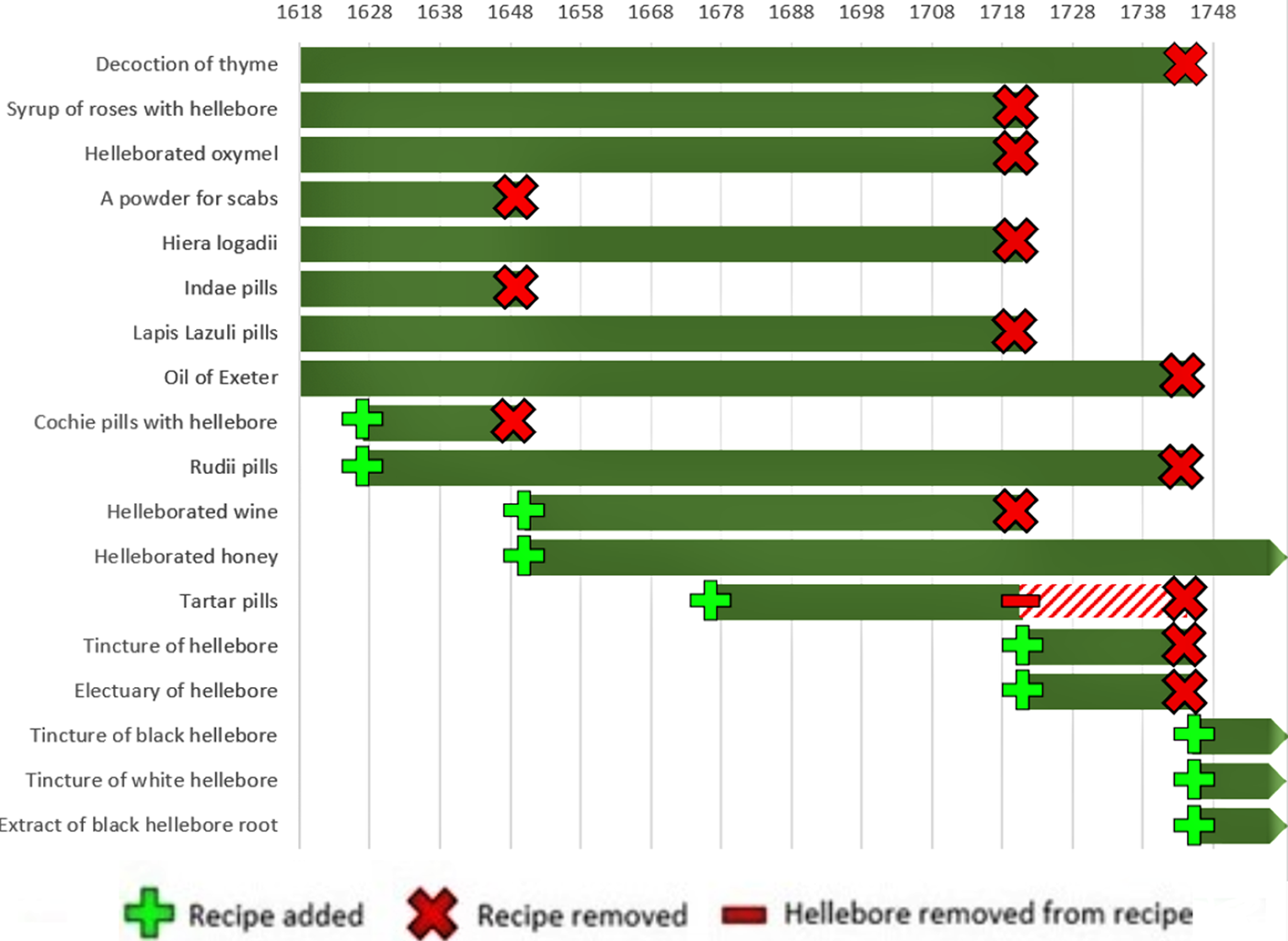
Figure 2 Timeline showing recipes containing hellebore in successive editions of the London College of Physicians’ London Pharmacopoeia, 1618–1745.
Purgative medicine, it seems, took on a life of its own in the seventeenth and eighteenth centuries, no longer dependent upon the humoral framework. Even as the foundations of humoral medicine came under increasing attack, most practitioners saw little reason to reject specific therapies that were obviously effective.Footnote 59 In 1667, the physician George Castle published The Chymical Galenist in an explicit attempt to reconcile humoral medicine with more recent developments in chemistry, anatomy, and physiology.Footnote 60 However, rather than attempting to retrofit purgative medicine into a chemical framework, Castle instead pointed out (correctly) that purging, as a medical practice, long predated even Hippocrates.Footnote 61 He singled out hellebore as an example of a substance whose effectiveness in treating melancholy disorders was held to be self-evident, claiming that “purging was not founded upon the notion of the four humors, but upon long observation, that when distempers discovered themselves by such and such signs, the body was to be emptied, and, by frequent trials, one purger (as especially hellebore in melancholy) was found more effectual than another.”Footnote 62 Castle clearly felt that the belief in the efficacy of hellebore transcended the dispute between humoralists and chemists; rather than being rooted in blind obeisance to ancient teachings, it was the product of centuries or even millennia of careful and sustained observation. For Castle—a committed Galenist but also a member of the Oxford Experimental Philosophy Club, which promoted chemical and mechanical investigations—there was no reason why new theories should invalidate established practices.Footnote 63
Even those who advocated a more radical split with humoral medicine were often reluctant to abandon hellebore, preferring instead to reframe its operation to accord with their own competing theories. One of the most fundamental challenges to humoral orthodoxy came from the Flemish physician and alchemist Jan Baptist van Helmont, whose ideas gained a significant following in mid-seventeenth-century England.Footnote 64 Van Helmont rejected the humoral pathology that had attributed emotional disturbance to vapors arising to the head from the spleen and stomach, instead putting forward a quasi-mystical physiology in which mental illness was caused by “Diseasie Seeds” and “excremental Ideas” conceived in the digestive organs.Footnote 65 The idea that the stomach, as opposed to the head, played the principal role in the genesis of pathological emotional states was central to Helmontian medicine, and to illustrate this point, Van Helmont drew upon reflections from his own experiences as a medical practitioner: “A greater authority of the stomach over the head is beheld, than of the head over the stomach, which I have above already demonstrated by many arguments: For truly, drowsiness, sleep, watching, doatages, and whatsoever symptoms are wont to be attributed to the head, are abolished by Stomatical remedies, but are not mitigated by Cephalical ones, or head-remedies: For hence is the Proverb, Oh head, that art worthy of Hellebor: For although manifold vomitive medicines are not wanting, yet a peculiar virtue is attributed to Hellebor for a mad brain.”Footnote 66 According to Van Helmont, however, hellebore's ability to cure madness depended less upon any affinity with the brain or head than upon its special sympathy with the lower parts: “Black Hellebor,” he wrote, “easeth madnesses before other vomitive medicines commonly known, because it unloads the antient fevers of the midriffs.”Footnote 67
The continued defense of hellebore even among those who rejected humoral theory suggests that the plant's persistence in practical medicine, despite the challenges posed by new ideas and new substances, was about far more than a lingering attachment to ancient theories and practices. For early modern Europeans, the relationship between digestive and emotional health was an integral part of lived reality, and while the precise nature of hellebore's therapeutic operation was a matter of dispute, few doubted its potency as a treatment for madness. Far more often, as I discuss below, criticisms of hellebore centered on the perceived dangers of a remedy that could kill as easily as it could cure.
Panacea or Poison?
Hellebore had an ambivalent reputation within the early modern materia medica. On the one hand, it drew high praise, and those who could attest firsthand to hellebore's healing powers were more than willing to tout them to friends and acquaintances. In a letter to the natural philosopher Anne Conway, Henry More recommended hellebore based on personal experience, calling it “a marvellous good medicine if it be given in its due doses.”Footnote 68 It was praised for its potency and the strength of its action in moving the belly; the Swiss physician Felix Platter described this effect as “so great that it will cure almost the desperate.”Footnote 69 When the York physician Martin Lister related a case of rabies to the Royal Society in 1683, he expressed bafflement that neither “bleeding, or the most famed antidotes, or even hellebore could in the least save [him].”Footnote 70 The extreme potency of hellebore was considered especially vital in cases of severe mental illness, which were believed to resist all but the most powerful remedies. In a work on nervous disorders published in 1729, Nicholas Robinson—a proponent of the new physiology and governor of the infamous Bedlam madhouse—reported, “Purging medicines of black hellebore, are mightily extoll'd” in cases of “raving madness,” which demanded “the most violent vomits, [and] the strongest purging medicines.”Footnote 71
However, the strength of hellebore was perceived by many to be excessive, especially when it was handled or administered inexpertly. Robert Boyle recalled an instance in which an acquaintance of his, during a medical demonstration, “[caused] a large quantity of black hellebore-root to be long pounded in a mortar . . . most of those who were in the room, and, especially, the person who powdered it, were thereby purged, and some of them strongly.”Footnote 72 Besides causing potentially embarrassing situations like this one, it was well known that an overly generous dose of hellebore could kill. The Hippocratic Aphorisms warned of the dangers of administering hellebore recklessly, and physicians generally recommended against prescribing it “to children, women with child, or weak persons”;Footnote 73 it was to be given only “warily, and to strong bodies.”Footnote 74 One French physician observed darkly, “it does not always benefit the sick; but it always harms those that are well.”Footnote 75 Numerous seventeenth-century accounts attest to hellebore's potential to do more harm than good. The Scottish clergyman Alexander Ross claimed, “I never knew what the cramp was, till I was let blood and purged with hellebore by an unskilful physician.”Footnote 76 The apothecary William Drage, meanwhile, reported, “When I was a youth, I took white hellebore for my quartan ague, and I had a convulsion of my gullet; so that it seemed to cleave together to my apprehension, and to rise as if somewhat was in my throat.”Footnote 77 In a characteristically cruel experiment conducted in the 1670s, the natural philosopher William Courten gave hellebore to a dog; the medicine “very much disordered him, and caused wretchings, suffocations, vomiting, and voiding of excrements.”Footnote 78 Even more dramatically, in 1602, a Middlesex gardener named John Pemmer was indicted before a jury for administering a fatal dose of hellebore to his neighbor, one Anne Fisher. The unfortunate Fisher, “ignorant of the effect of so great a quantity of White Elebore” and “being persuaded by John Pemmer it would be a remedy for her sickness,” died five days later.Footnote 79
In light of all this, it is hardly surprising that many regarded hellebore as a dangerous poison. One of its principal uses, besides curing mental illness, was to kill vermin. It was listed as rat poison in a number of sixteenth- and seventeenth-century herbals, and one commentator described it as “good only to choke daws withal;” Robert Burton acknowledged that many attributed “no other virtue to it, than to kill mice and rats, flies and mouldwarps.”Footnote 80 Drawing on the Natural History of Pliny the Elder, Burton presented a whole range of examples in which hellebore had been used as a fatal poison. It had supposedly been employed by the Greek statesman Solon to poison the spring of a besieged city, killing or weakening the inhabitants to procure his victory.Footnote 81 The French were said to have used it to poison their arrows for the hunt, “that the venison which they take will eat the tenderer; but then they cut away the flesh round about the wound made by the foresaid arrows.”Footnote 82 Its deadly potency evoked both gushing praise and harsh condemnation. As Shadi Bartsch has noted, hellebore embodied the ancient Greek medico-philosophical concept of pharmakon: “a medicine-poison that exemplifies the curious paradox of potentially being its own cure.”Footnote 83
This ambivalent status of hellebore, straddling the boundary between panacea and poison, made it a frequent focal point of medical controversy. A particularly public dispute over its dangers occurred around the middle of the seventeenth century, when the herbalist and astrologer Nicholas Culpeper took it upon himself to produce an unauthorized English translation of the Pharmacopoeia of the London College of Physicians.Footnote 84 From 1618, it became a legal requirement for apothecaries to arrange their medicinal compositions according to the guidelines of the College of Physicians as laid out in the Pharmacopoeia. This was ostensibly to ensure that drugs were made and distributed safely and effectively, but in practice it also enabled the college to impose restrictions on a potentially rival trade.Footnote 85 Culpeper, a republican and radical, saw the collapse of censorship in the 1640s as an opportunity to attack the college's attempted monopoly over medical practice.Footnote 86 In translating the Pharmacopoeia, he took the liberty of adding his own scathing commentaries to many of their compositions, especially those that contained hellebore. For instance, under “Syrup of Roses Solutive with Hellebore,” Culpeper wrote, “I wish the ignorant to let it alone, for fear it be too hard for them, and use them as coarsely as the College hath done.” He did, however, add grudgingly that the syrup “rightly used, purgeth melancholly, resisteth madness.”Footnote 87 In the case of “Honey Helleborated,” his criticisms were harsher still: “What a monstrum horrendum, horrible terrible receipt have we got here? . . . what should this medicine do? Purge melancholy say they, but from whom? From men or beasts? For the medicine would be so strong the Devil would not take it unless it were poured down his throat with a horn.”Footnote 88 Nearly every recipe containing hellebore received similar treatment from Culpeper, emphasizing the dangerous violence of the college's compositions and ridiculing their professional incompetence. He warned that hiera logadii—the compound favored by Richard Napier—“may well take away diseases by the roots, if it take away life and all.”Footnote 89 Under the purgative “Decoction of Epithimum,” he noted ominously, “Here is half a drachm of black hellebore added, and I like the receipt never the better for that.Footnote 90
In 1661, a new English edition of the Pharmacopoeia was published, this time approved and amended by members of the College of Physicians.Footnote 91 This edition removed Culpeper's more seditious rants and inserted an additional commentary for each medicine under the heading “Virtues newly added.” Sometimes these new additions explicitly contradicted or ridiculed Culpeper's earlier remarks, turning what was ostensibly a pharmacological manual into a cantankerous war of words. In response to Culpeper's attack on their “Decoction of Epithimum,” for instance, the college-friendly translation retorted, “Why the addition of half a drachm of black hellebore to this medicament by the College (as it seems) should be blamed by Culpeper, I see not . . . This medicament deserves the commendations given it.”Footnote 92 And in the case of “Syrup of Roses with Hellebore,” the college declared that “Culpeper might possibly have his considering cap on, but certainly his wits were on wool-gathering, when he censured this medicament.”Footnote 93 While acknowledging the perils of hellebore, the college physicians also took the opportunity to remind readers of the occasional need for a powerful cure. Under “Wine Helleborated,” for instance, they noted that “hellebore being a most violent and dangerous medicament, it is good to be very wary of the use hereof. Yet as Hippocrates says, strong diseases require strong medicaments.”Footnote 94 And concerning “Honey Helleborated,” even the college was forced to admit, “This is indeed a violent medicament not to be used but with great caution, in strong bodies and at the last cast when gentler medicaments will do no good.”Footnote 95
At no point in this dispute was the power of hellebore—either to cure or to kill—drawn into question. What Culpeper was disputing was the ability of the college to harness this life-threatening power effectively and humanely. Strong purgative drugs drew the particular attentions of medical reformers because the consequences of mishandling them could be catastrophic.Footnote 96 But with the proper knowledge and expertise, even hellebore could be administered safely and effectively. One of Culpeper's recurrent gripes against the College of Physicians concerned the boiling of hellebore, which he felt would either totally diminish its efficacy or leave it still potent enough to cause internal damage to the patient who took it: “Either the virtue of the hellebore will fly away in such a martyrdom, or else it will remain in the decoction. If it evaporate away, then is the medicine like themselves good for nothing. If it remain in, it is enough to spoil the strongest man breathing.”Footnote 97 Culpeper's comments were not dissimilar to those of other medical commentators, who felt that the art of giving hellebore lay in knowing the correct dose.Footnote 98 “Whatsoeuer others may feare or write,” insisted the English herbalist John Parkinson, both white and black hellebore “may be without danger applied, so [long] as care and skill, and not temerary rashnesse doe order and dispose of them.”Footnote 99
The ability to harness the curative powers of deadly purges like hellebore was one of the most frequent ways in which early modern physicians sought to consolidate professional power and demonstrate their unique mastery over disease.Footnote 100 “Tamed poisons,” the thinking ran, “become the most precious medicines”; only those who possessed the requisite skill and expertise, however, could be trusted to do the taming.Footnote 101 As illustrated by the case of Culpeper and the College of Physicians, seemingly minor quibbles over the inclusion or exclusion of hellebore in medicinal compounds could therefore function as shorthand for more fundamental disputes about professional competence. Similar concerns over hellebore's safety can be seen in the debate surrounding Mathews’ Pills, an evacuative and narcotic medicine that gained popularity from around the middle of the seventeenth century. The composition of the pills varied, but hellebore and opium were two of its core ingredients. According to their purported inventor, the alchemist Richard Mathews, the “venomous quality” of the hellebore was held to be “corrected” and thus rendered harmless by the inclusion of salt of tartar (potassium carbonate).Footnote 102 The pills became famous in Britain and the North American colonies, but the inclusion of hellebore drew condemnation from some quarters. The medical compiler William Salmon noted, “Some (in making this pill) leave out the white hellebore, and put in only the black; and some (very profitably in my judgement) leave them both out.”Footnote 103 John Quincy, a prominent English apothecary, agreed: “How much soever it may be imagined to stand corrected here, it is much safer left out.”Footnote 104 The College of Physicians in Edinburgh followed their example: “Some dislike the black hellebore; Quincy leaves out the white; and our college rejects both.”Footnote 105
One of the most influential English medical authorities to denounce the use of hellebore in Mathews’ Pills was the Oxford physician and anatomist Thomas Willis.Footnote 106 Hellebore, Willis claimed, had been used so frequently by the ancients only because few other remedies were then known; mental illnesses could be more safely and effectively treated with remedies targeting the head. “There is need of Physick for these,” he wrote, “tho not of Hellebore, but of Cephalick Remedies for corroborating the Brain.”Footnote 107 However, as noted above, the censure that surrounded hellebore rarely translated directly into practice, and Willis himself was not above recommending hellebore in extreme cases. In his London Practice of Physick, we find the following inclusion under cures for melancholy: “In Bodyes hard to be wrought on, let there be added to these, fibres of black Hellebore”; elsewhere he described it as “useful, yea very necessary in physick.”Footnote 108 Well into the eighteenth century, Mathews’ Pills containing hellebore were still being sold in both England and the Low Countries; the Dutch chemist Hermann Boerhaave noted, though with apparent skepticism, their tendency to provoke vomiting.Footnote 109
The ambivalent nature of many of these accounts leaves us with an untidy picture of hellebore's popular perception. One thing that can be said with some certainty is that hellebore sharply divided opinion, as the fierce dispute between Culpeper and the College of Physicians makes clear. Some believed that it was a magic bullet in laxative form, able to cure the most desperate emotional disorders even when other medicines and treatments fell short. Others assigned it the status of a deadly poison and issued stark warnings against its use. Ultimately, these seemingly polarized views of hellebore may have been just two sides of the same coin. The tone of many commentators suggests that hellebore's toxic reputation only reinforced the perception of its effectiveness. As a substance that exercised a harsh or even punitive action upon the body, hellebore produced a dramatic and tangible effect; physicians’ anxieties centered not so much on the risk of it not working as of it working too well. Using hellebore to treat mental illness was, then, a carefully judged balancing act. The severity of the condition had to be weighed against the danger of the cure, and the skillful physician knew how to administer just the right amount of toxin to drive out the greater poison already present within the sufferer.
Symbol and Substance
As a potentially deadly substance that could destroy a physician's reputation if given incorrectly, hellebore became a focal point for controversy in medical circles. Such was the vitriol with which Culpeper expressed his loathing of the College of Physicians that it prompted college physician William Johnson to quip of him, “You profess yourself student in physick, but want some physick yourself to purge away the malignant humor possesseth you, against the honourable Society of the College of Physicians . . . A little hellebore would do well to purge your brains with.”Footnote 110
Such insults played a key role in the intellectual and emotional life of early modern England. Physicians, theologians, politicians, and natural philosophers made their differences known through scathing battles of words, and professionals engaged in pamphlet wars to protect their reputations against libel (and, of course, to denounce and slander their enemies).Footnote 111 Within this world of backbiting, mockery, and colorful invective, hellebore reared its head with remarkable frequency. The precise language used in these disputes is often revealing. For instance, when William Barlow accused Mark Ridley of plagiarizing his unpublished work on magnetism, he publicly mocked his opponent's “unreasonable and senseless opinions, which have more need of helleborus to purge them out of his head, than arguments to confute them in his book.”Footnote 112 By evoking the image of hellebore, Barlow was able to cast his opponent as a fool governed entirely by his bodily fluids, unworthy of attention from the higher faculties of reason and judgment.
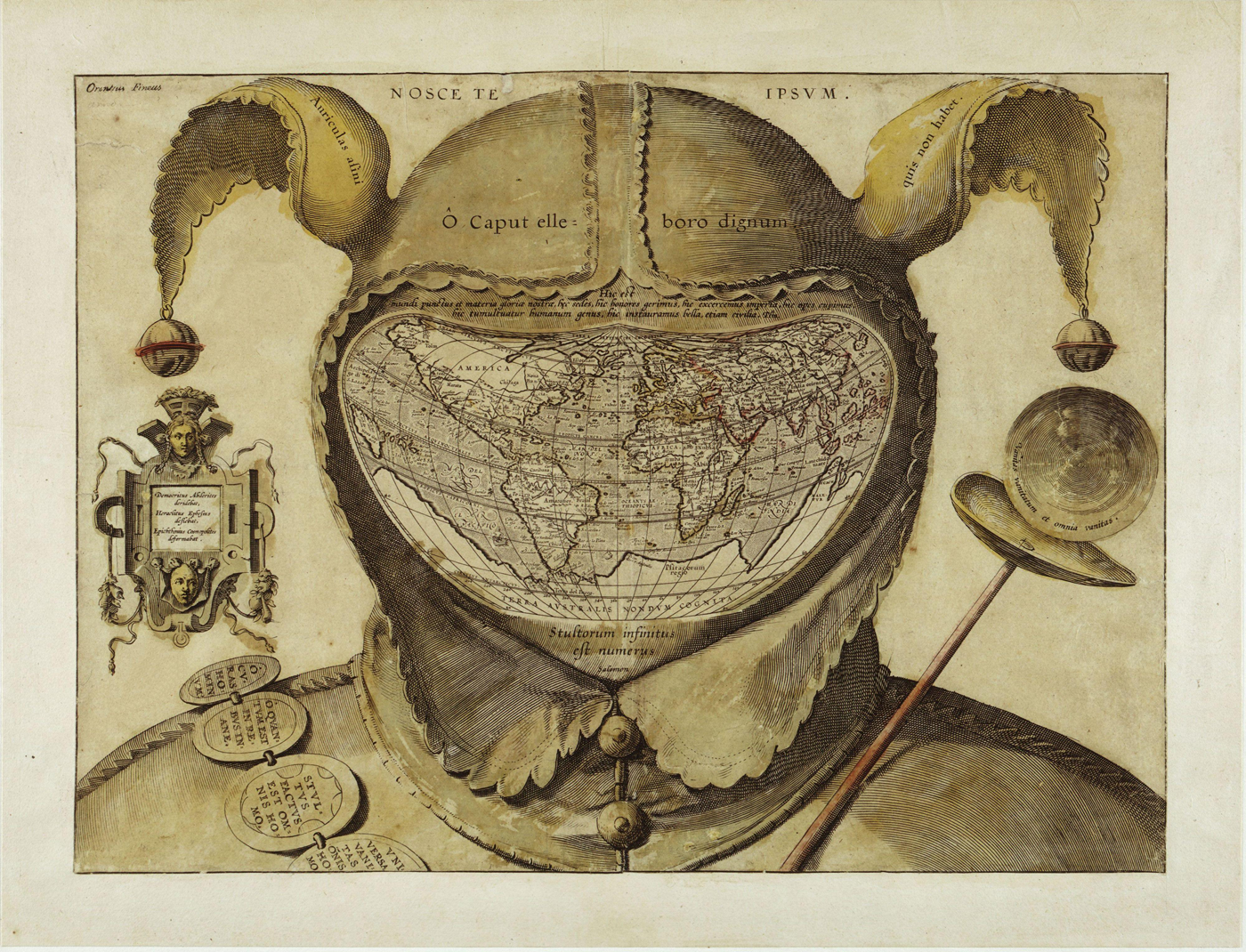
Figure 3 Fool's Cap Map of the World, artist unknown. The map appears to be based on Abraham Ortelius's third Typus Orbis Terrarum (1587). The inscription across the cap's brow reads “O caput elleboro dignum” (O head, worthy of hellebore).
The metaphor of hellebore was also used to evoke a more damning form of moral censure. Those who sinned, who coveted, who doubted God's word or accepted false idols, might all be called upon to take hellebore. In the spiritual turmoil of post-Reformation Britain, such insults were flung from all sides. One writer, in a 1616 diatribe against the “spirituall diseases” of Catholics, declared, “all the Helleborus in the world is not sufficient to purge them, that they may vomit out their follie.” Nonetheless, the author continued, “I have propounded in this discourse a strong potion compounded of ingredients; which if they bee not past cure, may purge and cleanse them of their disease, and reduce them to the sanity of Christian Religion.”Footnote 113 The Anglican clergyman Thomas Gataker, meanwhile, writing during the interregnum, used the metaphor of hellebore to mount a sarcastic attack on Calvinists and other religious sectarians, stating, “I wish you together well in your wits, and your pates with Ellebore throughlie purged.”Footnote 114 Conversely, the Calvinist bishop Joseph Hall used the plant to both cast doubt on his detractors and to instil the fear of God into his followers. As a prolific writer dealing frequently and extensively with religious controversy, Hall was particularly fond of the hellebore metaphor as a corrective both for foolishness and moral transgression, and returned to it at least eight separate times in his vast array of published works.Footnote 115 On the one hand, we can observe in Hall's writing the familiar satirical flourishes in which hellebore denoted ignorance or stupidity: his opponents’ arguments were, he declared, “worthy of a large dose of hellebore,” or “more fit for hellebore, than theological conviction.”Footnote 116 However, Hall's writings also demonstrated a profound spiritual hostility toward hellebore and its takers. Writing of the pathologically insane, he declared, “only dark rooms, and cords, and hellebore are meet receipts for these mental distempers.”Footnote 117 Hall used almost the exact same language—but this time, we assume, figuratively—in a diatribe against the Scottish Covenanter movement: “Our charity bids us hope . . . that you hate the frenzies of our wild country-men abroad, for whom no answer is indeed fit, but dark lodgings, and hellebore.”Footnote 118 The strength of feeling behind this statement is striking. Besides diagnosing the Covenanters as mad and recommending they be subjected to confinement and purgation, Hall also explicitly encouraged his readers to despise them.
The medical and moral discourses surrounding hellebore were suffused with a language of violence and fear. “Who hath not horror of the torments which both the hellebores bring to the body?” asked Timothie Bright in 1615.Footnote 119 George Kendall, in a passage from 1664 that was intended to provide a defense of Mathews’ Pills, expressed concern that a knowledge of the remedy's ingredients would “so affright weak and timorous persons, that they shall not dare to make use of it.”Footnote 120 It would be difficult to overstate the naked fear that hellebore, much like madness itself, was able to evoke. This emotive character was reflected in sensory descriptions that consistently emphasized its negative or hurtful aspects. Francis Bacon described it as “loathsome and of horrible taste” in his qualitative categorizations of purgative remedies, and John Floyer noted, “The smell of the root is very offensive,” adding that “it caused a pain in my tongue to the throat; the same it may cause in the stomach.”Footnote 121 When Martin Lister experimented on hellebore roots in 1695, he found them to be “of a very fiery and stinging nature” and reported that “the tops of my fingers, which were wetted with [hellebore] juice, did boaken and ache . . . that pain continued in them for several days; and at length the skin of my fingers end peeled off.”Footnote 122 To the touch, hellebore was “black, rough, [and] hairy,” tactile qualities that earned it the nickname “Bear's Foot.”Footnote 123 Descriptions of hellebore continually returned to these themes of violence, darkness, corruption, and filth, making it an appropriate vegetal analogue for the melancholy humor that was held to be the physiological cause of most mental perturbations.Footnote 124
The implications of hellebore's ambivalent status as poison/medicine went beyond the purely practical or physiological. The fact that humans could ingest hellebore without (necessarily) suffering fatal consequences was infused with moral significance, as it placed them in the gastronomic company of the goat, “a beast filthie, stinking, and vncleane.”Footnote 125 The most frequently cited Greek origin myth for hellebore as a treatment for madness was the story of Melampus the goatherd, who, observing that his goats regularly and intentionally purged themselves with the plant, gave it to the daughters of King Proetus, who believed themselves transformed into cows. After being chased through the fields and bathing in the fountains of Arcadia, the two princesses were cured of their bovine delusions when Melampus gave them hellebore infused in the milk of goats that had grazed upon it.Footnote 126
The symbolic association of goats with evil had deep cultural and theological roots. Goats, thought to be possessed of insatiable appetites and willing to consume (or copulate with) just about anything, were potent symbols of iniquity and debauchery. According to humoral dietary advice literature, goat meat was thought to breed “rank and filthy substance” and to predispose the body to melancholy diseases.Footnote 127 Moreover, the raw animality of goats was likened to the loss of rational self-control experienced in episodes of madness. Edward Topsell, in his work on four-footed animals, wrote, “There is no beast that is more prone and given to lust than is a goat . . . that which is most strange and horrible among other beasts is ordinary and common among these.”Footnote 128 The implication was that goats fed upon hellebore through an animal instinct toward self-purgation, as a natural counter-balance to their inherently sinful nature. For humans, the practice of purging with hellebore fulfilled a similar function, providing a physiologized ritual of atonement for inborn sin.
Still more revealing is the way in which the symbolism of opposing qualities was employed to place hellebore at the dark end of the moral spectrum. It seems likely that affective responses to the name black hellebore would have been largely negative in a religious culture in which blackness connoted evil and in which Hell was considered by many to be terrifyingly real.Footnote 129 In the Faerie Queene, Edmund Spenser listed hellebore among those plants that grew in the necropolitan Garden of Persephone, “direfull deadly blacke both leafe and bloom, / Fit to adorne the dead, and decke the drery toombe.”Footnote 130 The descriptive language of the early modern Christian world made frequent use of the light/dark opposition to convey positive and negative emotional states. As the alchemist George Starkey put it, “Verily there is nothing comfortable, but by reason of its participation of light, darkness being on the contrary a principle of dread and horror.”Footnote 131 Whiteness, by contrast, was seen as “the emblem of joy . . . where the emblem of whiteness is once had; the motto of joy and gladness will not long be behind.”Footnote 132 Stuart Clark has suggested that this sort of dichotomous thinking had such a great hold over early modern European culture that it can be described as “one of the distinctive mental and cultural traits of the age.”Footnote 133 In an example of what structural anthropologists term dual symbolic classification—the organization of seemingly disparate domains of cultural life into an overarching system of binary oppositions—early modern medicine credited the white variant of hellebore with the power to purge upward (by vomit) and the black downward (by stool).Footnote 134 In contemporary Christian cosmology, blackness and downward motion were firmly associated with corruption, the earth, and evil; conversely, whiteness and upward motion belonged to the realm of purity and the divine. As the Czech theologian Johann Comenius put it in 1633, “Blacknesse represents the earth in density; whitenesse the heaven in rarity.”Footnote 135 Hellebore, with its dark, excremental materiality, was clearly aligned with the former; and yet it also provided a means of moving oneself qualitatively closer to the latter.
The moral obsession with cleansing rituals and the necessity of maintaining an impossibly pure spiritual and physical interior therefore became central to the treatment of psychological distress in sixteenth- and seventeenth-century Europe. As Kuriyama has shown, while humoral medicine was theoretically concerned with the maintenance of balance, equilibrium, and the healthy flow of vital fluids, early modern practitioners were overwhelmingly preoccupied with the cleansing or scouring away of excremental matter.Footnote 136 This blurring of boundaries between morality and medicine was at its most pronounced in accounts of demonic possession. For the sufferer, possession, like madness, could be an intensely visceral process.Footnote 137 The afflicted person was often observed to evacuate all manner of strange objects: “Some diseased persons,” wrote John Cotta in 1616, “haue beene seene to vomit crooked iron, coales, brimstone, nailes, needles, pinnes, lumps of lead, waxe, hayre, strawe, and the like.”Footnote 138 Another common occurrence was the casting out of black liquid either by vomit or stool. In 1625, Joan Drake, a Buckinghamshire noblewoman and later “Puritan exemplar,” consumed forty oranges during a fit of despair brought on by demonic possession. According to her biographer, the fruit “proved excellent medicines unto her, purging away abundance of black ugly filthy matter, which made her to look much better.”Footnote 139
Many believed that the melancholy humor itself had a special affinity with devils and demons, a quality signified by its blackness, viscosity, and foul odor; “evil spirits,” warned Robert Burton, “take all opportunities of humours decayed . . . to pervert the soule of a man.”Footnote 140 In this view, melancholy could furnish the Devil with a physical seat or “bath” from which he could exercise his malicious designs upon body and soul.Footnote 141 The following extract, from a 1652 work on medicinal substances, can be viewed as an attempt to reconcile the materiality of melancholy with the divine and demonic realms: “Although the Devil cannot be cast out by human art or physical means, yet by taking black hellebore, the melancholy humour is drawn away (which is Balneum & sedes Diaboli, the bath and seat of the Devil) and so the Devil is more easily cast out, from whence it may rightly (say some) be called, fuga Daemonum.”Footnote 142 Despite its initial disclaimer, this account suggests a functional and substantive relationship between body and soul in cases of demonic possession. The Devil lodged himself wherever there was an accumulation of black bile—the head, spleen, stomach, and bowels—and was at least partially dependent upon this corporeal matter to retain his corrupting power over the individual's soul. A purgation of hellebore could thus provide both physical and spiritual deliverance, and to say so was not heretical so long as it was expressed in clearly analogous terms.
Thus while in theory the possessed person could only be truly healed through the “powerful exorcism of piety and prayer,”Footnote 143 in practice, as Piero Camporesi notes, “the techniques of evacuation and the art of the exorcist were so interlocked as to seem almost indistinguishable.”Footnote 144 The cure in cases of possession and madness commonly followed the same basic structure, with the deliverance of the sufferer depending upon dramatic and visceral expulsion.Footnote 145 Robert Burton, citing the Italian physician Antonio Musa Brasavola, described the case of a madman at the court of Ferrara—one “Melatasta”—who was believed to have been possessed by the Devil. After taking a purge of black hellebore, he reported that “his excrements were like ink: he perfectly healed at once.”Footnote 146 The Dutch surgeon Nicolaes Tulp treated a boy suffering from “most violent Fits of the Falling-sickness [epilepsy], which came upon him onely by pressing the region of the Spleen with ones finger.” Tulp gave an infusion of black hellebore in chalybeate water, after which the patient “voided so much black choler, that at last he came to himself.”Footnote 147 William Salmon recalled a young man so troubled with nightmares that he was afraid of going to sleep and had become fully convinced that he was cursed by some “unconquerable and uncontrollable power.” Following a purge of hellebore, “a great quantity of filthy matter, almost as black as ink came away, and he confessed himself very much relieved.”Footnote 148
In each of these accounts, the voiding of copious quantities of black liquid from the bowels was followed immediately by the report of recovery. While the violent expulsive properties of hellebore were called in to counteract the corrupting power of melancholy, both substances shared the same deeply negative symbolic load; the only way to cure the befouled body in cases like these was to voluntarily self-contaminate. This practice calls to mind the ritual behavior that anthropologists have termed respect pollution, in which deliverance from suffering is achieved through “a voluntary embrace of the symbols of death.”Footnote 149 A key feature of respect pollution is that deliverance can be achieved only through voluntary self-defilement, which serves as an acknowledgment of the sufferer's subordinate status in the natural order of things. “By doing that which under other circumstances would be defiling,” writes Edward Harper, “an individual expresses his inferior position.”Footnote 150 Descriptions of hellebore as a filthy, excremental substance reinforce this perception: taking it into the body was, in a sense, little better than consuming fecal matter itself—the ultimate act of moral depravity.
Viewed in this light, a prescription of hellebore becomes about much more than just the removal of corrupted physical matter. The black substance voided from the bowels was the embodiment of the evil cast out, with the site of spiritual transformation being neither the soul nor the mind but the gut. Taking hellebore presented many of the same dangers as the condition it purported to cure: loss of control, internal corruption, and the very real possibility of death. By forcibly confronting sufferers with their own embodiment, it offered a temporary reprieve from the existential anguish of madness and melancholy. In doing so, it confirmed what many godly individuals already believed: that their bodies were vile and filthy vessels and that their best hope for deliverance lay in abasement before God.
Conclusion
A close examination of the discourses around specific substances like hellebore can provide a revealing window onto the affective life of the past. Hellebore's status as a cure for mental illness was highly ambivalent and fraught with contradictions. The risks of taking hellebore were plain for all to see, and yet the perception of its danger seems only to have strengthened the widespread belief in its therapeutic efficacy. The example of hellebore encourages us to interrogate the dividing line between medicine and poison and to question what it means for a cure to be simultaneously punitive and palliative. Moreover, the ways in which early modern writers deployed the metaphor of hellebore reveal a great deal about the social and spiritual status of the mentally ill in early modern England. Whether it was used to ridicule one's professional rivals or to strike fear into the heart of the sinner, the rhetorical power of hellebore lay in its ability to evoke the sense of excremental abjection that was embodied in the figure of the mad person. The metaphor of hellebore—a dark, toxic, and generally reviled substance—formed part of a powerful “faecal imagery and rhetorics of abuse” that permeated public discourse in early modern England.Footnote 151
Above all, the example of hellebore presents a compelling case for viewing seventeenth-century diseases of the mind as inseparably tied up with the digestive tract. Even if we assume that hellebore offered little more than a placebo effect, its successful operation required both physicians and patients to believe in a functional and dynamic interplay between gut and mind, and to view their mental and moral states as essentially dependent upon the health and hygiene of their bowels. The black and stinking excrements of melancholy lurking in the folds of the viscera provided a suitably disturbing material analogue for the depraved spiritual condition of insanity. Appalled by the image of their own “glutted, unvented bodies,”Footnote 152 many early modern Europeans turned to hellebore for deliverance, reaching into the deepest parts of themselves and literally purging out the “dark inner violence” that lay within.Footnote 153 In this paradoxically therapeutic act of self-contamination, traditional binary oppositions—sacred and profane, divine and temporal, mental and physical—were effectively collapsed, and the excremental bowels became the site of a powerful ritual of spiritual purification.