The Food Standards Agency (FSA) needs to be able to assess the adequacy of vitamin D status in the population as a whole, and in specific subgroups of the population, and to know the proportion of each group falling above and below cut-offs for adequate status. Status is assessed by measuring plasma 25-hydroxyvitamin D (25OHD) in samples from the National Diet and Nutrition Survey (NDNS). Concern about the wide variability of 25OHD measurements made using different methods and in different laboratories(Reference Binkley, Krueger and Cowgill1–Reference Hollis3) led the Scientific Advisory Committee on Nutrition to advise that ‘there is an urgent need to standardise laboratory methodologies’(4). FSA required a robust method for use in future NDNS and other national surveys, which would also allow comparisons of circulating concentrations of 25OHD reported in earlier NDNS and other UK population studies with those reported in other countries.
A workshop was convened in November 2009 to recommend the most appropriate and secure method for measuring vitamin D status in the NDNS, and to identify methodological issues which need serious consideration. Workshop participants (the Expert Panel) were invited on the basis of expertise in current 25OHD assays, or expertise in vitamin D nutrition and metabolism or detailed knowledge and experience in the NDNS. Background information which had been collated during FSA project N08029 was pre-circulated to participants. The workshop was structured to explore the relevant issues, allow detailed discussion of them and finally come to a consensus recommendation. A decision support matrix, which detailed the criteria by which different options could be scored and evaluated, was used to structure the discussion. The Expert Panel agreed upon the criteria, options and scoring methods.
The current methodology used in the National Diet and Nutrition Survey
Dr Alison Tedstone, FSA, described the rationale for commissioning the project, and Dr Christine Clewes, MRC-HNR Cambridge, described the current methodology used in NDNS. Assessment of vitamin D status has been included in the NDNS programme since the 1990s, and is planned for inclusion in the Diet and Nutrition Survey of Infants and Young Children. The NDNS currently uses the Diasorin Liaison Total assay for the measurement of 25OHD. There are 800 μl of serum available for 25OHD analysis. In 2008–9, 534 samples were analysed for 25OHD out of a study population of 1646 men and women, of whom 575 provided blood samples.
Current methods available for measuring 25-hydroxyvitamin D
Professor Mike Wallace, Glasgow Royal Infirmary, presented a literature review on the different methods currently available for measuring 25OHD. The literature review identified sixty-eight publications on the measurement of 25OHD since the year 2000, which were categorised as being either quantitative (thirty-five papers), if they included comparisons of the performance of two or more methods, or qualitative (thirty-three papers), if they reviewed or commented on the results of other publications(Reference Wallace, Gibson and de la Hunty5).
There are currently two main types of methods used routinely: competitive immunoassays and methods based on chromatographic separation followed by non-immunological direct detection (HPLC-UV and LC–MS/MS). HPLC-UV and LC–MS/MS methods are able to measure 25OHD2 and 25OHD3 independently with good recoveries. Most immunoassays rely on antisera that can detect both 25OHD2 and 25OHD3, but the proportion of 25OHD2 detected is variable(Reference Carter, Jones and Berry6). Little detail is available on how commercial immunoassays are standardised. For HPLC-UV and LC–MS/MS, there is a lack of consistency in the way these procedures are standardised. In most HPLC-UV and LC–MS/MS methods, extraction and procedural losses are corrected for by the inclusion of an internal standard. Most procedures have the required sensitivity to identify severe vitamin D deficiency (25OHD < 25 nmol/l). RIA and LC–MS/MS are the more sensitive. In general, the precision of immunoassays, HPLC-UV and LC–MS/MS is comparable, with room for improvement. The main assay weaknesses highlighted in scientific publications were poor specificity, matrix interferences and the lack of a common standard(Reference Hollis3, Reference Beastall and Rainbow7, Reference Carter and Jones8). The main strengths identified were the ability of HPLC-UV and LC–MS/MS to measure 25OHD2 and 25OHD3 separately, and the convenience and high throughput using immunoassays performed on automated platforms. A more detailed account of current methodology can be found in a recent review(Reference Wallace, Gibson and de la Hunty5).
A. d. l. H., Ashwell Associates, presented the findings of a survey of UK laboratories registered with the vitamin D External Quality Assessment Scheme (DEQAS) to determine users' opinions on the main strengths and weaknesses associated with the different 25OHD methods (A de la Hunty, AM Wallace, S Gibson, et al., unpublished results). This had a response rate of 52 %. Respondents scored seventeen different criteria on a scale of 1–4. Strengths were defined as criteria with an average score of 3 or more, while weaknesses were defined as criteria scoring < 2. The overall assessment for immunoassays using non-isotopic labels, HPLC-UV and LC–MS/MS, was similar, but LC–MS/MS had more strengths and fewer weaknesses identified by users compared with other methods. The inability to measure 25OHD2 and 25OHD3 separately was the main criterion distinguishing opinions on immunoassays from HPLC-UV and LC–MS/MS.
Current variability in 25-hydroxyvitamin D measurements
Julia Jones, DEQAS, reminded workshop participants that DEQAS has been assessing the performance of 25OHD assays internationally for 20 years. Five samples of human serum are distributed quarterly, and individual laboratory performance is determined by comparison of the results with an all laboratory trimmed mean (ALTM), the current target value. The performance of different methods is assessed by comparing the method mean with the ALTM.
The majority of participants in the DEQAS (85 %) use commercial non-chromatographic immunoassay kits, but the use of chromatographic methods, HPLC-UV and, in particular, LC–MS/MS, is slowly increasing (14 %). Since DEQAS was launched, there has been a gradual improvement in overall inter-laboratory agreement, from a mean annual inter-laboratory CV of over 25 % in the 1990s to 16·3 % in 2009.
Difference in bias between methods is one cause of poor agreement between methods. For samples distributed in 2008, bias from the ALTM ranged from − 9·0 % for the Diasorin Liaison method to +9·5 % for LC–MS/MS. Approximately one-third of the participants now use the Diasorin Liaison Total 25OHD assay, which with a negative bias could significantly affect the ALTM. Using the mean of the method means as a target value instead, to give equal weighting to each method, raised the target value and resulted in a shift to a more negative bias for all methods. In 2008, the bias had a range of − 9·0 to 9·5 % (ALTM) and a range of − 11·5 to 6·5 % (mean of the method means). No overall change in the spread of bias between methods was observed.
DEQAS has investigated whether the use of a common standard would reduce inter-laboratory imprecision of HPLC-UV and LC–MS/MS assays. There was little effect on the former, but agreement among LC–MS/MS users was significantly better when all participants used the same standard, with the mean inter-laboratory imprecision falling from 16·4 to 10·4 % for total 25OHD measurements.
The relative merits of different methods
The relative merits of four of the main methods were outlined by experts in their use. Dr Tom Hill, University of Cork, reported that the Immunodiagnostic Systems (IDS) enzyme-linked immunoassay (EIA) has shown a mixed performance within DEQAS. The highest mean percentage bias from the ALTM was reported in 2006, with 28·7 and 23 % bias being described for the automated and manual IDS EIA, respectively. This high overestimation of 25OHD subsequently resulted in a re-calibration of the standard curve to improve the comparability of the assay. Since 2006, the performance of the manual IDS EIA, in particular, within DEQAS, has been improving, with a mean annual percentage bias from the ALTM in 2009 (three distributions only) being − 2 %. The validity of re-calibrating an assay to agree with the ALTM or another assay is questionable.
The major strengths of non-isotopic immunoassays include the convenience and high throughput capabilities of the assay. Whether the IDS EIA is significantly susceptible to matrix effects is open to debate, but recent evidence points to a particular effect with the automated platform. Problems associated with operator bias and intermittent batch analysis have been identified with the EIA and warrant attention. A major weakness with all immunoassays is the inability to quantify 25OHD2 and 25OHD3 separately. This may or may not be important depending on what the analyst requires from the assay. In addition, immunoassays vary in the proportion of 25OHD2 detected. The two metabolites, 25OHD2 and 25OHD3, assess the intake of vitamin D2 and intake and production, in skin, of vitamin D3, respectively. The circulating 25OHD2 concentration is normally low or undetectable unless the subject is receiving high amounts in the diet or from supplements. The IDS EIA does not appear to underestimate the presence of 25OHD2 in DEQAS samples, although the IDS RIA does despite the same antibodies being used in both IDS kits.
The Diasorin Liaison Total method, described by Professor Bruce Hollis, Medical University of Southern Carolina, provides readily accessible, uniform and standardised technology for high volume reference laboratories. The automated Diasorin Liaison Total assay is predicated on the Diasorin RIA, which was used to establish the reference ranges and cut-offs which have directed clinical practice for over 20 years. Under-recovery of 25OHD has, however, been observed in the National Institute of Standards and Technology (NIST) controls (SRM 972) to which 25OHD2 or 25OHD3 has been added. This problem was not observed in pools containing only endogenous 25OHD (discussed later).
The greatest advantage (and simultaneously one of the major disadvantages) of HPLC-UV, described by Dr Jacqueline Berry, University of Manchester, is that samples have to be extracted before being put onto HPLC-UV. This means that any potentially interfering substances such as proteins and lipids are removed, eliminating any related interference. The second advantage is the ability to measure 25OHD2 and 25OHD3 metabolites separately and accurately. Further advantages include its reliability, low batch-to-batch variation, its consistency between different operators and low limit of detection (5 nmol/l). These advantages are shared with LC–MS/MS, which has similar work-up procedures. The major disadvantage of HPLC-UV is the time-consuming and labour-intensive extraction procedure that limits the number of samples that can be processed per day. HPLC-UV methods can handle about fifty samples per day; however, several laboratories have now developed methods to automate the extraction process, so the low throughput may not be a problem in the future.
With the UV detection method, there are occasionally substances unrelated to vitamin D that will produce an interfering peak close to that of interest. For example, the C-3 epimer is known to be present at high concentrations in the circulation of some neonates (and also possibly in some adult samples). The C-3 epimer of 25OHD3 can be resolved using HPLC-UV by adaptation of a reverse-phase column and extending the run time. Different views were expressed by the workshop participants on the utility of quantifying the C-3 epimer, which, to date, has no known function. To gain more information on the C-3 epimer of 25OHD3, it will be quantified in National Health and Nutrition Examination Survey (NHANES).
Dr Sandra Rainbow, Northwick Park Hospital, described how LC–MS/MS has, over the past 5 years, become the method of choice for the quantitation of specific steroid-like molecules, including 25OHD, in biological fluids. The technique allows equivalent, or better, detection levels than an immunoassay and greater specificity, and is applicable through semi-automated processing to relatively large sample numbers analysed in batch mode. Several LC–MS/MS methods for the analysis of 250HD2 and 25OHD3 have been published in the last 5 years, which differ in either the sample preparation technique or selection of fragmentation pattern.
The strengths of the LC–MS/MS process include the ability to independently quantify 25OHD2 and 25OHD3 and, with suitable adaptation, other related metabolites of interest. Furthermore, sensitivity exceeds that of most immunoassays, and good inter-laboratory precision can be achieved if a common standard is used. Although the equipment is expensive, reagent costs are low and the use of radioisotopes is eliminated. Weaknesses of LC–MS/MS include the lack of a standardised method, the high cost of equipment, the possibility of interference with the C-3 epimer of 25OHD3, and the high level of expertise necessary to develop the method and run the equipment.
The US experience
Dr Mary-Frances Picciano, National Institutes of Health, and Dr Rosemary L. Schleicher, Centers for Disease Control and Prevention (CDC), explained why the US national survey, NHANES, starting with the NHANES 2007–2008, will use an LC-MS/MS method instead of using the Diasorin Liaison immunoassay to measure 25OHD. Dr Karen Phinney, NIST, described the development of the standard reference material (SRM 972) for 25OHD.
CDC discontinued using the Diasorin RIA for NHANES at the end of the NHANES 2005–6, and dedicated several years to the development of an LC–MS/MS method. CDC cited internal and published data(Reference Roth, Schmidt G and Weber9) demonstrating poor specificity of immunoassays compared with chromatographic methods. While HPLC-UV and LC–MS/MS showed outstanding comparability for 25OHD when directly compared(Reference Roth, Schmidt G and Weber9), isotope dilution tandem MS offers superior sensitivity, accuracy and precision. CDC had concluded that the Diasorin immunoassay lacked the precision necessary for NHANES, and that the changes made to the assay in the late 1990s had affected its performance. The reformulated Diasorin assay used during NHANES 2000–6 produced 12 % lower 25OHD results than the original assay used for NHANES 1988–94. Shifts in quality-control values, as a result of reagent lot variation, also complicated the interpretation of time trend data.
The CDC nutrition laboratory has now developed and validated an automated LC–MS/MS method for monitoring 25OHD2 and 25OHD3 in NHANES. A refinement that will allow the separation and measurement of the C-3 epimer of 25OHD3 is under development. Reconciliation of the values obtained in NHANES in previous years using the Diasorin RIA method with those obtained using the new LC–MS/MS method will involve re-measuring approximately 100 samples from each of seven previous years with the new LC–MS/MS method and calculating regression equations for each year.
NIST has recently developed a SRM for vitamin D metabolites (SRM 972), which consists of four pools of fresh frozen serum(Reference Phinney10) and these will be used to standardise the calibration of the LC–MS/MS method for NHANES. Each pool has a different concentration of 25OHD2, 25OHD3 or both. One pool also contains a C-3 epimer (3-epi-25OHD3), a metabolite that may be present at significant concentrations in infant serum. As part of the value assignment of SRM 972, NIST developed an isotope-dilution LC–MS/MS methodology capable of resolving C-3 epimers. This method is being submitted for approval by the Joint Committee for Traceability in Laboratory Medicine as a reference measurement procedure (RMP).
As indicated earlier, measurement of the recovery of exogenously spiked samples appears not to be suitable for testing the ability of an immunoassay to measure endogenous 25OHD. The use of spiked SRM 972 pools should probably be restricted to assess the accuracy of HPLC-UV and LC–MS/MS methods only. Furthermore, the SRM 972 pool diluted with horse serum may not be suitable for the assessment of immunoassays due to matrix-related interferences in this type of assay. The endogenous human serum, however, does appear to provide comparable results in all assay procedures. A formal commutability study is needed to assess which levels of SRM 972 are appropriate to use with individual assays.
Lessons from elsewhere
Professor Linda Thienpont, University of Ghent, described the determination of the ideal specifications for a reference measurement system for 25OHD, which includes both routine and reference measurements(Reference Stöckl, Sluss and Thienpont11). The specification goals for a RMP should be related to those for routine measurements; the imprecision (CV) of an RMP should be half of that of the goal for routine measurements, while the bias should be one-third of the bias goal for routine measurements. Achievable goals for routine measurements could be based on those determined by biological variation and reference intervals. Thus ideally, routine testing of 25OHD, such as that carried out in the NDNS, should have a precision (CV) ≤ 10 % and bias ≤ 5 %. These values should be incorporated into the final specification of the method chosen for the NDNS.
Professor Mike Wallace, Glasgow Royal Infirmary, discussed lessons which could be learnt from the measurement of other hard-to-measure hormones. Recent standardisation issues for the measurement of growth hormone have been resolved by the use of a common international standard, achieved by detailed guidelines and recommendations formulated by the Society for Endocrinology(Reference Wieringa and Trainer12). Testosterone, like 25OHD, is a steroid that circulates in nmol/l concentrations bound to a high-affinity specific binding protein. In response to concerns about the validity of some testosterone assays, the Endocrine Society in the United States recently published a position statement, which concluded that direct immunoassays perform poorly at low testosterone concentrations and should be avoided(Reference Rosner, Auchus and Azziz13). They recommended that extraction and chromatography, followed by MS or immunoassay, were likely to furnish more reliable testosterone results. Similar recommendations for harmonising 25OHD measurements would be helpful.
The requirement for a RMP for 25OHD was highlighted by Graham Carter from DEQAS. There is an urgent need for a definitive method for 25OHD which is accepted to give the ‘true’ 25OHD concentration in serum samples(Reference Carter and Jones8). Historically, GC–MS has been used as the RMP for steroid assays, but several LC–MS/MS methods have been recently promoted as candidate RMP for 25OHD. If an LC–MS/MS method is chosen as an RMP, its status would be greatly enhanced if results were confirmed by GC–MS. DEQAS has commissioned the development of a GC–MS method, which will be used to check the validity of the ALTM as a surrogate for the true value and/or for assigning target values to DEQAS samples. Early results are promising.
The need for the separate measurement of 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3
Professor Christel Lamberg-Allardt, University of Helsinki, discussed whether the separate measurement of 25OHD2 and 25OHD3 was necessary for population monitoring of 25OHD status (C Lamberg-Allardt, unpublished results). There are differences in the biological activity and the toxicity of vitamins D2 and D3. The intestinal absorption of vitamin D2 is lower than that of vitamin D3. The clearance of 25OHD2 from circulation is faster than that of 25OHD3, which could be due to the lower affinity of 25OHD2 to vitamin D-binding protein. Furthermore, there are some differences in the metabolism between these two forms of vitamin D. Thus, the serum concentration of 25OHD2 may not be equipotent to that of 25OHD3.
There are few sources of vitamin D2 in the diet: it is mainly found in wild mushrooms. Some studies have shown that irradiation of cultivated mushrooms increases their vitamin D2 content. Vitamin D3 is the form mostly used in supplements and fortified foods. Hence, vitamin D3 is the predominant form, arising from cutaneous synthesis, from food, and from fortified foods and supplements.
There are few population studies showing detectable circulating concentrations of 25OHD2. Unpublished results from the OPTIFORD study show that the proportion of the population with detectable levels of 25OHD2 is low (about 5 %). Nevertheless, at least in Finland, the vitamin supplements given as drops to infants contain vitamin D2, and their serum will mainly contain 25OHD2. In a recent report from West London in the UK, in which a high proportion of subjects were Asian, about 16 % of the patients had detectable serum 25OHD2 concentrations(Reference Costelloe, Woolman and Rainbow14). In conclusion, the need for measuring 25OHD2 and 25OHD3 separately depends on the future use of vitamin D2 in food fortification and as supplements, as the natural food sources are of marginal importance. The measurement of 25OHD2 could be important at the individual level.
Using the decision support matrix to reach consensus on methodology
Criteria
The purpose of the decision support matrix is to structure discussion and aid the evaluation and comparison of the different 25OHD methods for the NDNS. The Expert Panel was asked to consider which criteria should be used and which methods should be evaluated. After a plenary discussion, the Expert Panel voted by a substantial majority to use eleven criteria for the evaluation procedure (see Table 1). They did not think it was necessary to weight the criteria because this would over-complicate the matrix. It was, however, made clear that this decision did not mean that all criteria had equal importance.
Table 1 The eleven criteria used to evaluate suitability for measuring 25-hydroxyvitamin D (25OHD) in the National Diet and Nutrition Survey (NDNS)
ALTM, all laboratory trimmed mean; MOMM, mean of method means; NIST, National Institute of Standards and Technology; DEQAS, vitamin D External Quality Assessment Scheme; VIM, Vocabulaire International de Métrologie.
* The Expert Panel agreed that the ability to discriminate the C-3 epimer should be included as a criterion since the method would also be used in the forthcoming Diet and Nutrition Survey of Infants and Young Children.
† The Expert Panel agreed that a limit of quantitation in the region of < 10 nmol/l ( ± 5 %) was sufficient for the purposes of the NDNS.
‡ As there is no ‘gold standard’ for 25OHD methods, the Expert Panel agreed that accuracy or ‘trueness’ could not be assessed against one. It was agreed that assessment of accuracy against the NIST standard reference materials and the NIST candidate reference method procedure was the best currently available approach.
§ Subsequent to the workshop, it was suggested that it would have been better if an internationally accepted definition of trueness had been used. This is trueness: closeness of agreement between the average of an infinite number of replicate measured quantity values and a reference quantity value (VIM). In practice, this means a small percentage bias from the ‘truth’ as we know it now(15, 16).
∥ It was agreed that the ability of a method to be adjusted to the NIST standard (SRM 972 Level 1) should be a criterion.
¶ It was agreed that operator skills and laboratory facilities should be considered as part of the feasibility of setting up the method in the UK.
Methods for measuring 25-hydroxyvitamin D
The Expert Panel considered eight potential methods on which they felt there was adequate published information to evaluate (see Table 2). They decided to exclude three methods for the following reasons:
1 The Roche assay as it only measures 25OHD3.
2 The two RIA methods as the NDNS had already moved away from using an RIA method. Current UK Health and Safety policies restrict their use, and it is likely they will be phased out in future.
Table 2 The eight potential methods considered and the five methods (in italics) chosen to evaluate in the decision support matrix
IDS, Immunodiagnostic Systems; EIA, enzyme-linked immunoassay.
The Expert Panel agreed to evaluate five methods (Diasorin Liaison, IDS EIA automated, IDS EIA manual, HPLC-UV and LC–MS/MS) against the eleven agreed criteria.
Evaluating the different methodologies according to the decision support matrix
The participants in the Expert Panel were divided into three breakout groups, chosen to ensure a range of expertise in each group. The breakout groups were asked to score each of the five methods from 1 to 4 against the eleven agreed criteria (1, not good; 2, acceptable; 3, good; 4, very good). Groups were encouraged to give a consensus score and to record their comments or any conditions for each score; the scores from each breakout group were then pooled. Breakout groups were given the option of changing their score if the plenary discussion revealed that they had interpreted the criteria in a slightly different way. The final criteria, and agreed definitions against which the different methods were evaluated, are those listed in Table 1.
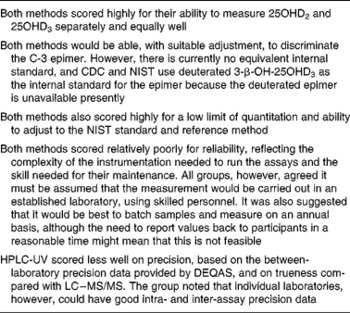
The scores for the individual groups were very similar. All three groups scored LC–MS/MS and HPLC-UV similarly highly, while the scores given by all groups for the immunoassays were lower. The total ‘plenary’ score for each method (as listed in Table 3) therefore reflected these differences. It was agreed that the scores for each method reflected the discussions about the strengths and weaknesses of the different methods, in relation to the particular requirements of the NDNS. The majority view was that only two methods (HPLC-UV and LC–MS/MS) should go on for further discussion. There was little to discriminate between the scores of the three immunoassays, and of the three methods, the Diasorin Liaison Total method scored the highest. Discussion thereafter focussed on LC–MS/MS and HPLC-UV. Table 4 summarises their strengths and weaknesses.
Table 3 Pooled scores* from all three breakout groups evaluating five methods against eleven criteria
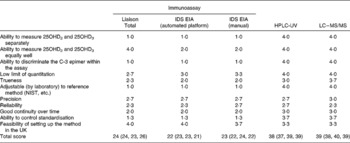
IDS, Immunodiagnostic Systems; EIA, enzyme-linked immunoassay; 25OHD, 25-hydroxyvitamin D; NIST, National Institute of Standards and Technology.
* Scoring: 1, not good; 2, acceptable; 3, good; 4, very good.
Table 4 Strengths and weaknesses of HPLC-UV and LC–MS/MS
25OHD, 25-hydroxyvitamin D; CDC, Centers for Disease Control and Prevention; NIST, National Institute of Standards and Technology; DEQAS, vitamin D External Quality Assessment Scheme.
Recommendations for 25-hydroxyvitamin D methodology for use in National Diet and Nutrition Survey
Both HPLC-UV and LC–MS/MS scored similarly highly, and there was little to discriminate between them according to the criteria against which they had been evaluated. It was agreed, however, that LC–MS/MS should be recommended as the preferred method for the NDNS as this would facilitate future comparisons on 25OHD status with NHANES. The fact that NHANES has recently made the change to LC–MS/MS from immunoassay and has already put reconciliation measures in place strongly influenced the Expert Panel to recommend this methodology to FSA for use in NDNS. If FSA accepts this recommendation, the Expert Panel suggested the following considerations:
1 The particular characteristics the specific method needs to achieve in terms of sensitivity, precision and accuracy should be specified at the outset.
2 The specification should be drawn up in close liaison with US CDC to ensure that the method used for NDNS is similar to that used for NHANES. A visit to the CDC Micronutrient laboratory in Atlanta by the successful contractor is recommended.
3 There is a potential problem with the blood collection tubes used in the NDNS (Sarstedt Monovette™ tubes) as they could introduce ion suppression effects in LC–MS/MS. The method can be adapted to prevent the problem from occurring.
4 The use of the NIST standards (SRM 972) or secondary standards calibrated against NIST standards is recommended.
5 A reconciliation procedure is needed to be able to compare the results measured previously using Diasorin Liaison Total method with those obtained using the suggested LC–MS/MS method. It will be necessary to run the two methods together for a while to perform a cross-over study. This will enable a correction factor or derived equation (or factors for low/medium/high concentrations) to be determined for values previously measured with the Diasorin Liaison method.
6 Ideally, there should be a limited range of methods being used by FSA contractors measuring 25OHD. The results obtained by other FSA-funded projects should be comparable with the values obtained from the NDNS. As each research contract is put out to tender, the FSA should reserve the option to decide to specify a single laboratory for the measurement of 25OHD for all its research projects.
7 While LC–MS/MS is capable of quantitating 25OHD2 and 25OHD3 separately, the FSA should seek advice on whether it needs to report both separately, as will be done in NHANES. The Expert Panel advised that, when reporting values back to participants, only total 25OHD (25OHD3+25OHD2) should be reported, in keeping with usual UK clinical practice.
8 The LC–MS/MS method chosen will need to be adjusted to ensure that it is able to discriminate the C-3 epimer of 25OHD3, especially in the Diet and Nutrition Survey of Infants and Young Children. The Expert Panel thought that until it was known whether the C-3 epimer was functional, there was probably no need to quantify it.
Conclusions and recommendations
The Expert Panel recommended that an LC–MS/MS method should be the preferred method for the NDNS. A detailed specification for the method will be required to ensure comparability between NDNS and NHANES in the US facilitating future comparisons. The Expert Panel also recommended that the method should be carried out in a laboratory with appropriate expertise, competency and history of records of good performance. The method should be standardised against NIST SRM 972. If the recommended LC–MS/MS is adopted, the Expert Panel indicated that the method should be able to discriminate the C-3 epimer of 25OHD3, especially if used to measure 25OHD in young infants in the forthcoming Diet and Nutrition Survey of Infants and Young Children, who are known to have high circulating concentrations of the C-3 epimer.
List of participants (Food Standards Agency Workshop NO8029)
Expert Panel: Dr Jackie Berry, Manchester Royal Infirmary, Manchester; Graham Carter, DEQAS, London; Dr Christine Clewes (was at), MRC Human Nutrition Research, Cambridge; Professor David Fraser, University of Sydney, Australia; Dr Dominic Harrington, St Thomas' Hospital, London; Dr Tom Hill, University College, Cork, Ireland; Professor Bruce Hollis, Medical University of South Carolina, USA; Julia Jones, DEQAS, London; Dr Susan Knox, Glasgow Royal Infirmary, Glasgow; Dr Susan Lanham-New, University of Surrey, Guildford; Dr Helen Macdonald, University of Aberdeen, Aberdeen; Professor Hugh Makin, St Bartholomew's and the Royal London School of Medicine and Dentistry, London; Dr Karen Phinney, NIST, USA; Dr Mary-Frances Picciano, Office National Institutes of Health, USA; Dr Sandra Rainbow, Northwick Park Hospital, Harrow; Dr Rosemary L. Schleicher, CDC, USA; Dr Inez Schoenmakers, MRC Human Nutrition Research, Cambridge; Dr Martin Shearer, Guy's and St Thomas' NHS Foundation Trust, London; Dr Dietmar Stockl, Ghent University, Belgium; Professor Linda Thienpont, Ghent University, Belgium; FSA: Dr Fiona Comrie (FSA Scotland); Dr Alison Tedstone; Heiko Stolte; Dr Elaine Stone; Gillian Swan; Ashwell Associates consortium: Dr Margaret Ashwell; A. d. l. H.; S. G.; Professor Christel Lamberg-Allardt and H. V., University of Helsinki, Finland; Professor Mike Wallace, Glasgow Royal Infirmary, Glasgow.
Acknowledgements
No author has any conflicts of interest. A. d. l. H., M. A., S. G., A. M. W., C. L-.A. and H. V. were contracted by the FSA to organise and be rapporteurs of the Workshop. A. d. l. H. produced the first and subsequent versions of the manuscript, to which all other authors contributed substantially, in terms of drafting, critical reviewing and editing.






