Background
Prevalence of depression among older people in the United Kingdom
Depression is the most common mental health problem among older people (Audit Commission, 2002), and the overall prevalence of depression warranting clinical intervention is 10% among people over the age of 60 years (Wilson et al., Reference Wilson, Mottram, Sivananthan and Nightingale2001). Clinically significant depression and milder forms of depression are disproportionately more common in people living in care homes than in similarly aged people living in primary care (Bruce et al., Reference Bruce, Brown, Raue, Miodzianowski, Meyers, Leon, Heo, Byers, Greenberg, Rinder and Nassisi2007).
Prevalence of depression among older people in care homes in the United Kingdom
Reports of the prevalence of depression vary, according to the assessment method used and the sample of residents assessed. The prevalence of depression among people aged ⩾65 years living in UK residential care in the 1990s was 27%, using a nurse-administered Geriatric Mental State Examination, compared with 9% in those living at home (McDougall et al., Reference McDougall, Matthews, Kvaal, Dewey and Brayne2007); and in 1997, 44% of residents were assessed as having case or sub-case-level depression (Lyne et al., Reference Lyne, Moxon, Sinclair, Young, Kirk and Ellinson2006). Among people newly admitted to care homes in the late 1990s, 38–45% were identified as being depressed by a staff assessment using a 15-item Geriatric Depression Scale (GDS; Godlove Mozley et al., Reference Godlove Mozley, Challis, Sutcliffe, Bagley, Burns, Huxley and Cordingley2000; Sutcliffe et al., Reference Sutcliffe, Burns, Challis, Godlove Mosley, Cordingley, Bagely and Huxley2007). In comparison, among older people who attended a local authority day centre, 42% were assessed as being depressed (Minardi and Blanchard, Reference Minardi and Blanchard2004).
Prevalence of depression among older people outside the United Kingdom
In the United States, 27% of older people not living in residential care present with psychological distress symptoms; and of these, 70% present with moderate psychological distress, and 30% with clinical depression (Preville et al., Reference Preville, Coté, Boyer and Hebert2004). Rates of depression range from 13.5% to 26.0% among older people receiving home health-care services (Bruce et al., Reference Bruce, McAvay, Raue, Brown, Meyers, Keohane, Jagoda and Weber2002). On the basis of psychiatric evaluation, the prevalence estimate was 14.4% for major depression in nursing homes and 16.8% for minor depression, whereas the prevalence of significant depressive symptomatology (including possible depression) was 44% (Teresi et al., Reference Teresi, Abrams, Holmes, Ramirez and Eimicke2001). Of the individuals living in nursing homes or long-term care facilities, 10% were clinically depressed (Preville et al., Reference Preville, Coté, Boyer and Hebert2004); and in care home residents in Southern California, 8.5% met criteria for probable major depression and 1.6% for mild depression.
In Botany, Australia, the estimated total prevalence of depressive disorders among older people was between 13.0% and 13.6% (4.6% major depression, 3.6% dementia with depression, 5.4% other depressive disorders; Snowdon and Lane, Reference Snowdon and Lane2001).
Depression and dementia
Depression is more common in those with dementia (McDougall et al., Reference McDougall, Matthews, Kvaal, Dewey and Brayne2007). About 40% of people with dementia will be depressed, but people with dementia, who have experienced a severely threatening life event in the preceding three months, are far more likely to be depressed (Waite et al., Reference Waite, Bebbington and Skelton-Robinson2004). The results showed that 62% of people with dementia who had experienced a severely threatening and independent life event in the preceding 3 months were depressed, compared with only 28% of those people with dementia without such events. Depressed people with dementia may present with behavioural problems, leading to a delayed or missed depression diagnosis, whereas older people with depression may present with memory problems, interpreted as cognitive impairment rather than depression (Curran and Shafiq, Reference Curran and Shafiq2006).
Factors associated with depression in care homes
In care home populations, service users often have several co-morbidities. Some people resident in care homes may feel that their lives have been enriched, whereas others may feel their life has been restricted (Cook and Stanley, Reference Cook and Stanley2009). Major depression in care home residents is significantly associated with medical morbidity, activities of daily living disability, reported pain and a past history of depression (Bruce et al., Reference Bruce, McAvay, Raue, Brown, Meyers, Keohane, Jagoda and Weber2002). Depression is significantly associated with younger age and high functional disability in those living in care homes; it is more common in those with dementia and co-morbid medical conditions (McDougall et al., Reference McDougall, Matthews, Kvaal, Dewey and Brayne2007).
In a survey of 244 UK care homes, staff indicated (with non-mutually exclusive categories) that 22% of residents’ mental state was normal; 64% were confused or forgetful; 20% showed challenging behaviour; and 19% were depressed or agitated (Bowman et al., Reference Bowman, Whistler and Ellerby2004). In all, 36% of residents had been admitted because of dementia and 7% because of depression (Bowman et al., Reference Bowman, Whistler and Ellerby2004).
Identification of depression in older people
Depression and anxiety disorders are frequently not identified among older adults. The presentation of depression in older people is slightly different from that in younger populations and is confounded by the complex interplay between physical illness and depression (Curran and Shafiq, Reference Curran and Shafiq2006). Depressed elderly people are less likely to report a dysphoric mood than young adults and are more likely to pay attention to their physical symptoms (Preville et al., Reference Preville, Coté, Boyer and Hebert2004). This tendency for older people not to complain about depression frequently results in the diagnosis being overlooked and memory problems may be mis-diagnosed as cognitive impairment or dementia (Curran and Shafiq, Reference Curran and Shafiq2006). The National Service Framework (NSF) for Older People reports that depression is under-diagnosed among people aged ⩾65 years and the problem is worse for care home residents (Department of Health, 2001). Many older people do not receive treatment because of the difficulties associated with recognising the condition (Wilson et al., Reference Wilson, Mottram and Vassilas2008). In a New York study in nursing homes, only 37–45% of residents diagnosed by psychiatrists were recognised as being depressed by staff (Teresi et al., Reference Teresi, Abrams, Holmes, Ramirez and Eimicke2001).
Assessment by care home staff
Care home staff generally have limited or no specific training in identifying depression, understanding its causes and the potential for effective treatment (Bagley et al., Reference Bagley, Cordingly, Burns, Mozley, Sutcliffe, Challis and Huxley2000), and hence usually do not identify depression (Bruce et al., Reference Bruce, Brown, Raue, Miodzianowski, Meyers, Leon, Heo, Byers, Greenberg, Rinder and Nassisi2007). Nurses may also be uncomfortable with assessing depression (Brown et al., Reference Brown, Meyers, Lee, Fyffe, Raue and Bruce2004b). Nurses using a structured diagnostic interview may only identify half of the people with depression (Dalton and Busch, Reference Dalton and Busch1995). However, training nurses to assess for depression can lead to appropriate referral and care for patients with depression (Bruce et al., Reference Bruce, Brown, Raue, Miodzianowski, Meyers, Leon, Heo, Byers, Greenberg, Rinder and Nassisi2007).
Management of depression among older people
The efficacy of antidepressants such as selective serotonin reuptake inhibitors and tricyclic antidepressants (TCAs) is similar for treating depression in older adults; however, classical TCAs are associated with a higher withdrawal rate due to side effects (Mottram et al., Reference Mottram, Wilson and Strobl2006), and thus they are not often used in practice (Curran and Shafiq, Reference Curran and Shafiq2006). There is little evidence to show the effectiveness of psychotherapy for depression in older people; however, Cognitive Behavioural Therapy may be of benefit (Bruce et al., Reference Bruce, Brown, Raue, Miodzianowski, Meyers, Leon, Heo, Byers, Greenberg, Rinder and Nassisi2007; Wilson et al., Reference Wilson, Mottram and Vassilas2008), although this is not widely available in the UK National Health Service (NHS).
Despite the availability of effective treatments, because care home residents may not be diagnosed as being depressed many may not receive adequate management for their depression; and 18% of those prescribed appropriate doses of antidepressants may not comply with their antidepressant treatment (Bruce et al., Reference Bruce, McAvay, Raue, Brown, Meyers, Keohane, Jagoda and Weber2002). One US study identified that 13.5% of residents had major depression, yet only about one-fifth (22%) of these depressed residents were prescribed antidepressant treatment, and none received psychotherapy. In addition, some were prescribed sub-therapeutic doses of antidepressants (Baldwin et al., Reference Baldwin, Chiu and Katona2002) or received a trial course of antidepressant for too limited a time period, and hence the optimum therapeutic effect was not achieved.
Summary
Research is needed to establish ways of improving the identification and management of depression in older adults in care homes (Brown et al., Reference Brown, Bruce, McAvay, Raue, Lachs and Nassisi2004a; Sherlock, Reference Sherlock2005).
Study aim and objectives
The aim of this feasibility study was to compare the level of depression among care home residents, as identified by senior care staff, with two different assessments of depression in the same environments by a psychiatrist. Both study psychiatrists were very experienced, Members of the Royal College of Psychiatrists, with more than two years of higher training as Specialist Registrars in Old Age Psychiatry. The senior care staff were defined as those having a registered nurse qualification or National Vocational Qualification level 2 or 3 in care.
The study objectives were:
• To determine the number and proportion of residents with mild, moderate and severe depression, according to senior care staff.
• To interview all residents providing informed consent, using the 30-item GDS and ICD-10 criteria (WHO, 2004).
• To record medicines and therapies received by residents in the week before the interview, based on the record of administration of prescribed medicines.
• To calculate the proportion of residents experiencing mild, moderate or severe depression, assessed by a psychiatrist using ICD-10 criteria and the 30-item GDS.
• To assess the level of undetected depression among residents by comparing levels of depression identified using ICD-10 criteria with the levels as assessed by senior care staff.
• To compare the levels of depression among residents as assessed by the GDS administered by a psychiatrist, with the levels assessed by a psychiatrist using ICD-10 criteria.
• To compare the levels of depression among residents as assessed by the GDS administered by a psychiatrist, with the levels assessed by senior care staff.
Study methods
Access to study population
The study was approved by the local NHS R&D Consortium, received ethical approval from the University Institutional ethics panel and was approved by the local District Council under the Research Governance Framework. The study took place from July 2009 to July 2010.
There were 51 potentially eligible care homes in the Metropolitan District (UK). The homes were placed in a randomly ordered list, and those at the top of the list were approached in sequence. Six homes were approached, and four of the six (66.7%) agreed to take part in the feasibility study. A letter was sent to the four homes to gain permission from the managers and senior care staff to conduct the study. In addition, a letter was sent to the attending general practitioners (GPs) responsible for residents in the four care homes explaining the study. The two study psychiatrists were required to gain the trust of staff and residents, and treat interviewees with dignity and respect and conduct the interviews. They were supervised by a consultant psychiatrist.
Inclusion criteria
All residents aged ⩾65 years in the participating care home were invited to take part in the study provided they were not experiencing any difficulty rendering them unable to give informed consent, or a consultee was able to represent the resident's wishes and consent on their behalf.
Exclusion criteria
Residents were not included in the study if they had a Mini Mental State Examination (MMSE; Folstein et al., Reference Folstein, Folstein and McHugh1975) score of <11 or were otherwise cognitively impaired. The MMSE is a set of questions that takes 5–10 min to administer, and tests cognitive domains including orientation to time and place, repetition, verbal recall, attention and calculation, language and visual construction. The total score ranges from 0 (impaired) to 30 (normal; Ridha and Rossor, Reference Ridha and Rossor2005).
The consent process
Once permission to access a care home was gained, each care home resident who met the inclusion criteria was approached with an invitation to participate. Residents were provided with written information in large print about the study, and had the opportunity to ask questions; and once agreement to participate was elicited, they were invited to give their written consent to take part. Each care home manager generated a comprehensive list of the names of all consenting residents who were assigned a study identification number. No names were recorded on data collection forms. The psychiatrists approached each resident sequentially to ensure that there was no selection bias.
As the study involved vulnerable adults, some with a mental illness such as dementia or cognitive impairment, the consent process adhered to the requirements of the Mental Capacity Act (OPSI, 2007). Capacity was assessed by a study psychiatrist who also administered the MMSE to determine the level of cognitive impairment and to make a judgement about capacity.
For any resident who lacked capacity, a suitable person was chosen who was willing and able to act as a personal consultee and advise the researcher on whether the resident would want to be involved in the study. Any resident lacking capacity, or showing any sign that they did not wish to be involved, was not included in the study.
Care staff assessment forms (CSAFs)
The senior member of care staff for each resident was asked to complete the CSAF for each consenting participant during the daytime, to indicate whether the resident had exhibited symptoms of depression in the past seven days, as well as the severity (mild, moderate, severe), if applicable. This form was not seen by the interviewing psychiatrists who were blinded to the CSAF outcome. The care home staff provided a list of medications administered over the previous week for each resident, indicating the route and frequency of the medications.
Interview by a psychiatrist
After the CSAF was completed, the psychiatrists performed the interview with the resident, privately, which took about one hour. The participant was first interviewed using the GDS to identify symptoms of depression, then by a comprehensive diagnostic clinical interview using ICD-10 criteria. The GDS is a sensitively worded, 30-item scale requiring yes or no responses. The instrument has a score range of 0–30 and is widely used with older people to assess feelings over the previous seven days. This GDS focuses on cognitive aspects of depression rather than the physical symptoms of depression (eg, tiredness) to identify depressive symptoms even among people with physical symptoms or illness. A score of 0–10 indicates no depression, 11–20 indicates mild depression and 21–30 indicates severe depression. At a cut-off score of 11, the sensitivity was 0.84 and specificity was 0.95 (Brink et al., Reference Brink, Yesavage and Lum1982); and in a systematic review, with pooled GDS-30 studies, sensitivity was 0.75 and specificity was 0.77 (Wancata et al., Reference Wancata, Alexandrowicz, Marquart, Weiss and Friedrich2006). The presence of mild to moderate dementia was found not to impair the accuracy of the GDS (O'Riordan et al., Reference O'Riordan, Hayes, O'Neill, Shelley, Walsh and Coakley1990).
In this way, the study generated an assessment of depression symptoms for each consenting resident, from the perspective of the senior member of care staff and a study psychiatrist. If during the interview the psychiatrist found that the resident had depression or another mental illness, the resident, the resident's GP and the senior member of care staff were informed of the outcome after the interview.
Data management and analysis
All the CSAFs and interview forms were returned to the principal investigator and were stored in a locked environment, and data were entered in a password-protected database.
Primary analysis
The primary analysis directly compared the numbers and proportions of residents identified as not depressed, mildly depressed, moderately depressed or severely depressed by the CSAF with those identified according to ICD-10 criteria, and then secondly with those identified according to the GDS outcome.
Sensitivity, specificity and positive predictive value
The sensitivity (the probability that a resident with depression would be identified as having depression), specificity (the probability that a resident without depression would be identified as not having depression) and positive predictive value (PPV; the probability that a resident identified as having depression would have depression) were calculated for the CSAF and GDS, against the ICD-10 as the ‘gold standard’.
The sensitivity, specificity and PPV analysis was performed using two thresholds for the GDS (10 and 11), and a dichotomised outcome (presence or absence of depression) was used for the CSAF, GDS and ICD-10 assessments. Cohen's weighted Kappa (κ) statistic (using quadratic weights) was used to assess the agreement between the CSAF and GDS outcomes.
Results
In all, six care homes were invited to take part, of which two care homes chose not to take part because they were ‘too busy’ and the other four homes agreed. All four homes had a proportion of nursing care and residential care places for elderly people, people aged over 65 years with dementia, people aged over 65 years with a mental disorder and people aged over 65 years with physical disability.
Residents consenting to take part
The number and proportion of all residents consenting to take part and any reason for ineligibility were documented, per location, as indicated in Table 1.
Table 1 Number of consenting participants per care home as a proportion of the total number of residents and reason for non-consent
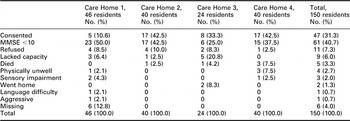
Note: Care Home 1: residents, with nursing, old age, dementia or mental disorder or physical disability over 65 years; Care Home 2: residents with old age, dementia or mental disorder over 65 years; Care Home 3: residents with old age, dementia or mental disorder over 65 years; Care Home 4: old age residents, with nursing.
Residents categorised as being depressed
The numbers and percentages of residents identified as being depressed according to each of the three assessment methods, is shown in Table 2.
Table 2 Number of participants identified as being depressed according to three assessment methods
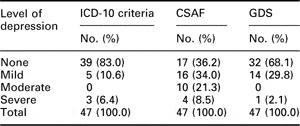
CSAF = care staff assessment form; GDS = Geriatric Depression Scale.
Sensitivity, specificity and positive predictive value results
The sensitivity, specificity, PPV and likelihood ratios calculated using the CSAF and the GDS are summarised in Table 3 along with the posterior probabilities, which incorporate prior estimates of the prevalence of depression.
Table 3 Sensitivity, specificity and PPV of CSAF and GDS, according to ICD-10 criteria
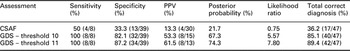
CSAF = care staff assessment form; GDS = Geriatric Depression Scale; PPV = positive predictive value.
CSAF results
Compared with the ICD-10 criteria, the sensitivity using the CSAF was 50.0% (see Table 3), the specificity was 33.3% and the PPV was 13.3%. In total, 36.2% received a correct diagnosis (presence or absence of depression) using the CSAF. The low likelihood ratio obtained for the CSAF (0.75) suggests that this method of assessment did not provide useful information for diagnosing depression. The calculated PPV of 13.3% may be compared with the corresponding posterior probability of 21.7% incorporating the estimated 27% prevalence of depression among older people aged ⩾65 years living in UK care homes (McDougall et al., Reference McDougall, Matthews, Kvaal, Dewey and Brayne2007).
GDS at a threshold of 10 and 11
For the GDS, results are also presented in Table 3 for a threshold of 10 (ie, scores of 9 and under indicating no depression) and 11 (ie, scores of 10 and under indicating no depression). This reflects reported variations in the use and interpretation of the threshold score (Wancata et al., Reference Wancata, Alexandrowicz, Marquart, Weiss and Friedrich2006). Compared with the ICD-10 criteria, the sensitivity using the GDS at a threshold of both 10 and 11 was 100% (see Table 3). The calculated PPVs may be compared with the corresponding posterior probabilities of 67.3% and 74.3% incorporating the estimated 27% prevalence value. In total, 85.1% received a correct diagnosis (either presence or absence of depression) using the GDS at a threshold of 10 and 89.4% using a threshold of 11.
High values of the likelihood ratio obtained for the GDS (5.57 for threshold 10 and 7.80 for threshold 11) indicated that this test provided some useful information, in that a diagnosis of depression was more likely to be made for a resident with depression than for a resident who was not depressed, using the GDS.
Receiver operator characteristic (ROC) curve
The optimum combination of the sensitivity of 1.00 and specificity of 0.87 was associated with the GDS threshold score of 11, as indicated by the top left-hand point in Figure 1. For a threshold of 10, the sensitivity was 1.00 and the specificity was 0.82. For a threshold of 12, the sensitivity was 0.88 and the specificity was 0.82.
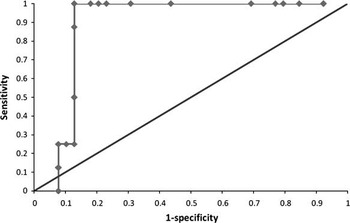
Figure 1 Area under the receiver operator characteristic (ROC) curve for the 30-item Geriatric Depression Scale to identify depression, according to a diagnostic assessment using ICD-10 criteria
Results for prescription of antidepressants
A wide range of medications was reported to have been administered to participants in the week before the interview, indicating a range of physical health problems, as indicated in Table 4. Almost all (93.5%) of the residents (43/46) were prescribed at least one drug for cardiovascular problems (antiplatelets, cardiac drugs, diuretics, antihypertensives, lipid regulation and omega-3 fatty acids) and 56.5% (26/46) were prescribed an analgesic. Of the 47 participants, 22 (46.8%) were prescribed an antidepressant, and three of all participants (6.4%) were prescribed two different antidepressants.
Table 4 Most frequently documented medications taken by residents in the previous week
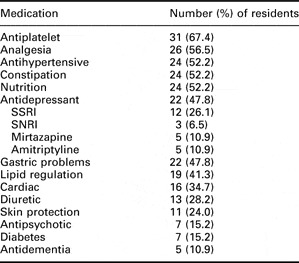
SSRI = selective serotonin reuptake inhibitor; SNRIs = serotonin and norepinephrine reuptake inhibitors.
In all, 39.1% (18/46) of participating residents were prescribed an antidepressant and were no longer depressed and 8.7% (4/46) of residents were prescribed an antidepressant and remained depressed. In this study, there were 6.5% (3/46) residents the study (ICD-10) identified as being depressed who were not prescribed an antidepressant. There were 45.6% (21/46) residents who were not depressed and were not prescribed an antidepressant. That is, 54% (25/46) residents either had been, or were currently depressed.
Agreement between assessment methods
The agreement between the CSAF and GDS outcomes was 0.22 using Cohen's weighted κ statistic (Armitage et al., Reference Armitage, Berry and Matthews2005), using quadratic weights. This level of agreement is normally assessed as ‘fair’.
Discussion
Participants
In this study, the proportion of residents consenting ranged from 10% to 43% between the care homes and the proportion of residents excluded because of a lack of capacity ranged from 38% to 57% between the care homes. In contrast, 16% of the nursing home residents in the New York sample could not be assessed because of refusal, physical illness, advanced dementia and/or impaired communication (Teresi et al., Reference Teresi, Abrams, Holmes, Ramirez and Eimicke2001).
Prevalence of depression among participants
The proportion of residents (17%) identified as having depression using the ICD-10 criteria was lower than the 27% reported in other studies of depression among elderly people aged ⩾65 years living in UK care homes and higher than the 9% reported in those living at home (McDougall et al., Reference McDougall, Matthews, Kvaal, Dewey and Brayne2007). There are a number of possible explanations for this; the possibility of selection bias due to self-selection among care home managers who chose to take part and the possibility of some self-selection among the residents themselves, with those less likely to be depressed consenting to take part.
A more plausible explanation might be that the management of depression within these homes (47.8% residents had been prescribed an antidepressant) had reduced the overall prevalence of depression. It was assumed that 54% (25/46) of residents either had been suffering from depression (as indicated by their antidepressant prescription) or were currently depressed (as indicated by the diagnostic interview). It was assumed that the antidepressant prescription was effective in treating depression in 39.1% (18/46) of residents who were prescribed an antidepressant and were no longer depressed. However, 8.7% (4/46) of residents who were prescribed an antidepressant remained depressed; the antidepressant may have been newly prescribed, at too low a dose, or the resident may not have taken the antidepressant.
As there were 6.5% (3/46) residents who were identified as being depressed, who were not prescribed an antidepressant, it was assumed that the level of undiagnosed depression was 6.5%.
It is likely that the prevalence of depression would have been higher had the study included residents who had advanced dementia and incapacity problems. However, it was not possible to undertake a full psychiatric history, the full range of clinical and physical assessments, brain scans and further investigations that would have been required to exclude treatable causes of dementia.
CSAFs results
The proportion of residents assessed as being depressed by care staff (64%) was higher than the 17% identified by the diagnostic clinical interview, indicating that the care staff had rated non-depressed residents as depressed, as was found in an earlier study (Eisses et al., Reference Eisses, Kluiter, Jongenelis, Pot, Beekman and Ormel2005). It was not possible for the assessment outcome to have changed between assessments, as the CSAF was completed in the same week as the GDS and the ICD-10 diagnostic criteria were applied, during the same interview. That is, it was unlikely that some residents’ depression had improved during this interval and that the CSAF was indicating true depression.
It is possible that there was a research effect, whereby the care home staff were motivated to identify depression as they were taking part in a study. Another explanation might be that care home staff were sensitive to some of the symptoms of depression; however, a lack of specific training meant that they saw some residents as being unhappy, having some symptoms of depression and interpreted this as depression. However, depression is indicated by a combination of symptoms, in addition to low mood, such as loss of appetite and sleep-related problems, loss of interest and lack of energy. These symptoms of depression are more common than a clinical diagnosis of depression. About a quarter of elderly people living in nursing homes or long-term care facilities present a high level of psychological distress symptoms that do not meet the criteria for major depression diagnosis (Blazer, Reference Blazer1993).
A further explanation might be that the staff were aware of the antidepressant prescription and regarded 82% (18/22) of these residents as being depressed and 18% as not depressed, even though following the antidepressant prescription 82% (18/22) were no longer diagnosed as being depressed.
Care home staff are very busy and have much paperwork to complete for each resident, in addition to addressing the residents’ care needs. As part of the admission process for new residents, staff need to assess whether an individual is depressed, without knowing the person's usual presentation. Care staff voiced their uncertainty about how to identify whether a service user who was grieving for a spouse who had recently died was becoming depressed. Help to improve the efficiency of their assessment, such as externally provided training, might be valuable for the staff and the residents. Care staff expressed great interest in the possibility of training to help them to better understand depression.
A study in the Netherlands (Eisses et al., Reference Eisses, Kluiter, Jongenelis, Pot, Beekman and Ormel2005) found beneficial effects of a programme of staff training in improving detection, treatment and the course of depression in normal practice. The study found that the care staff appreciated the training and received valuable tools to deal with vulnerable residents. A routine screening tool for depression can be used with minimal in-house training to improve the detection of depression among older adults with significant physical and functional impairment.
Performance of the GDS
The GDS, with a sensitivity of 100%, a specificity of 87.2% and a PPV of 61.5%, at a threshold of 11 performed more efficiently as a method of diagnosing depression than the CSAF with a sensitivity of 50% and specificity of 33.3%. These results are consistent with findings in a systematic review, with pooled GDS-30 studies, where the sensitivity was 0.75 and specificity was 0.77 (Wancata et al., Reference Wancata, Alexandrowicz, Marquart, Weiss and Friedrich2006). As an instrument that does not require a medically trained person for its administration, there is the potential to use the GDS in a care home setting, following staff training, either for self-administration by residents, or staff administration.
Reliability of the clinical assessment by the psychiatrists
Rather than one assessor consistently undertaking the assessment, two psychiatrists performed the interviews, but they did not both assess the same patients. It is possible that there was a variation among the outcomes of the assessors, although this was unlikely.
Medication
The prescribed medications indicated a range of morbidity among the participants and that 47.8% were taking at least one antidepressant. A relatively high proportion of residents had been prescribed amitriptyline, a TCA, which is regarded as poorly tolerated because of their side-effect profile that includes memory impairment and delirium at high doses (Curran and Shafiq, Reference Curran and Shafiq2006), as well as cardiovascular effects (NCCMH, 2009). As paroxetine may be associated with fewer adverse effects (NCCMH, 2009), this finding warrants further review.
Although four participants had been prescribed an antidepressant with no apparent benefit, NICE Guidance (2009) suggests that most improvement will begin in the first week an antidepressant is taken and emphasises the importance of monitoring. Of greater concern was the 6.5% (3/46) of residents with unidentified depression, as indicated by the lack of an antidepressant prescription.
Strengths and limitations of the study
The study, with a small sample of four care homes and 47 consenting residents, demonstrated that a clinical assessment for depression and an assessment by care home staff could be undertaken in a care home setting. It was possible to compare the results gained from a gold standard clinical assessment with those gained from the GDS and an assessment by care home staff. This study is among the first to explore the level of undetected depression in care homes.
At the time of recruitment, the participating care homes faced additional difficulties such as the swine flu scare, a new manager in post and an infectious outbreak. It is a credit to the homes that they agreed to undertake the study burden of the additional time to assess the participants and document prescription data in detail.
The main limitation of the study is that it is a cross-sectional study of a sample of four care homes, representing less than 8% of homes in the area, and thus the representativeness for all care homes in the area cannot be established. There is potentially some bias in the sample of care homes recruited and in the sample of participants consenting to take part. Therefore, the results from the study must be treated with caution. A larger sample of randomly selected care homes and a random selection of participants may have enhanced the generalisability of the findings.
A further limitation is that the study excluded residents with a poor MMSE score because of the difficulty in administering the GDS with these people, although it is likely that around 40% of these people with dementia may have been depressed (Waite et al., Reference Waite, Bebbington and Skelton-Robinson2004; Thompsell, Reference Thompsell2006).
Summary and conclusion
This was a small feasibility study that tested the process of consenting older people in a care home setting and undertaking a clinical interview to identify depressive symptoms. The care home staff were very supportive of the study and took the time to undertake the assessments, as well as provide a detailed list of the residents’ medication. The CSAF was inadequate for accurately identifying depression among residents, indicating a training need among care home staff to improve the identification and management of depression in older adults in care homes. The GDS performed well in this group of participants. The results should be treated with caution, as this was a small study. However, they indicated that 47.8% residents were being treated for depression in the care homes; most depression was managed successfully with an antidepressant prescription and 6.5% residents had unidentified depression. Further research is warranted to examine the cost-effectiveness of training care home staff in ways to improve the identification and management of depression in older adults in care homes.







