CLINICAL SCENARIO
A 23-year-old female presents with right lower quadrant pain that has been intermittent for the past several days. The pain suddenly worsened 1 hour ago. She denies vaginal bleeding or discharge, dysuria, fever, and back pain, but she has had several episodes of nausea with nonbloody, nonbilious vomiting. On examination, she is tender in the right lower quadrant, but her abdomen is not rigid.
KEY CLINICAL QUESTIONS
- 1.
Does ovarian torsion only occur in women of reproductive age?
Ovarian torsion predominantly affects reproductive-aged women, with a mean age of 30 years. The most common risk factor for ovarian torsion is an adnexal mass > 5 cm (80% of all patients),Reference Varras, Tsikini and Polyzos1–Reference White and Stella3 but the absence of an ovarian mass or cyst does not exclude torsion. Other risk factors include prior fertility therapies, history of ovarian torsion or tubal surgery, and polycystic ovarian syndrome.Reference Varras, Tsikini and Polyzos1–Reference White and Stella3 Close to 15% of all ovarian torsion cases occur in pediatric patients, and over half of these patients have normal ovaries.Reference Houry and Abbott2,Reference Karaman, Beger, Çetin, Melek and Karaman4 Postmenopausal patients account for 15% of cases, most commonly associated with an ovarian mass, and 10–25% of cases occur in pregnant women, typically in the first trimester.Reference Bouguizane, Bibi and Farhat5,Reference Chiou, Lev-Toaff and Masuda6
- 2.
Does ovarian torsion present with predictable symptoms?
The classic presentation of ovarian torsion is abrupt, severe, lower abdominal pain with nausea and vomiting, but the presentation is variable.Reference Houry and Abbott2,Reference White and Stella3,Reference Huchon, Panel and Kayem7 No one historical or physical examination finding should be used in isolation or in combination to rule in or out the diagnosis. Over 90% of patients have some form of abdominal pain, but abrupt pain occurs in less than 60% of patients.Reference Houry and Abbott2,Reference White and Stella3,Reference Huchon, Panel and Kayem7 Approximately 70% of patients experience nausea and vomiting, and fever may occur in 2–20%.Reference Houry and Abbott2,Reference White and Stella3,Reference Huchon, Panel and Kayem7 Pediatric patients may present with irritability and feeding intolerance.Reference Varras, Tsikini and Polyzos1,Reference White and Stella3 However, much of the literature evaluating these findings consists of small sample sizes from different settings and populations.
- 3.
How reliable is the abdominal and pelvic examination in the evaluation for suspected ovarian torsion?
Similar to the history, physical examination is not reliable for diagnosis. Most patients have abdominal pain and tenderness to palpation, but up to 30% of patients will not have tenderness on abdominal or pelvic examination.Reference Houry and Abbott2,Reference Huchon, Panel and Kayem7 While a significant risk factor for ovarian torsion is an ovarian cyst or mass, pelvic examination demonstrates poor sensitivity in detecting a mass, and obesity and age > 55 years further reduce the reliability of the examination.Reference Close, Sachs and Dyne8,Reference Ueland, DePriest and DeSimone9 While the pelvic examination should not be used to rule in or rule out the diagnosis, it may be useful when considering alternatives in the differential diagnosis.
- 4.
Can a pelvic ultrasound with normal arterial flow exclude the diagnosis of ovarian torsion?
The first-line imaging modality for evaluation of suspected ovarian torsion is ultrasound, either transabdominal in pediatric or virginal patients or transvaginal in other populations. Ultrasound can be used to rule in the disease, but it should not be used to rule out ovarian torsion, as the sensitivity ranges from 35% to 85%.Reference Varras, Tsikini and Polyzos1,Reference Swenson, Lourenco and Beaudoin10,Reference Wilkinson and Sanderson11 However, studies evaluating ultrasound for diagnosis of ovarian torsion suffer from several limitations, including poor sample sizes, different gold standards for diagnosis, and heterogenous imaging findings. The most common finding on ultrasound with gray-scale imaging is an enlarged, edematous ovary. The whirlpool sign, consisting of a hyperechoic structure with multiple inner hypoechoic rings wrapped around a central axis, is pathognomonic for torsion.Reference Wilkinson and Sanderson11 Other findings on ultrasound suggestive of torsion include displacement of the affected ovary toward the midline, peripherally displaced follicles with an afollicular stroma, and a hypoechoic ovary.Reference Varras, Tsikini and Polyzos1,Reference Swenson, Lourenco and Beaudoin10,Reference Wilkinson and Sanderson11 Doppler may demonstrate reduced or absent venous flow, and in later stages of torsion, absent arterial flow may be found.Reference Swenson, Lourenco and Beaudoin10–Reference Chiou, Lev-Toaff and Masuda13 However, arterial flow is normal in 25% of cases and will be present in over 50% of ultrasound examinations.Reference Nizar, Deutsch and Filmer12,Reference Chiou, Lev-Toaff and Masuda13 The combination of an enlarged ovary, any abnormal Doppler flow, and free pelvic fluid is associated with high specificity and positive predictive value for the diagnosis of ovarian torsion.Reference Swenson, Lourenco and Beaudoin10,Reference Wilkinson and Sanderson11
- 5.
What findings on CT suggest ovarian torsion?
While ultrasound is the recommended first-line imaging test for suspected torsion, CT with intravenous (IV) contrast may demonstrate findings consistent with ovarian torsion, particularly a twisted vascular pedicle, thickened Fallopian tube, abnormal ovarian enhancement, and an ovary with afollicular stroma with peripherally displaced follicles.Reference Swenson, Lourenco and Beaudoin10,Reference Wilkinson and Sanderson11,Reference Chiou, Lev-Toaff and Masuda13 One small case-control study comparing ultrasound and CT found similar diagnostic performance for diagnosis of ovarian torsion, although it is limited by its retrospective nature and small sample size.Reference Swenson, Lourenco and Beaudoin10 Other findings that demonstrate high sensitivity for the diagnosis of ovarian torsion but are not specific include an adnexal mass or enlarged ovary, free pelvic fluid, uterine deviation toward the affected ovary, ovarian displacement toward the uterus, and inflammatory stranding surrounding the affected ovary.Reference Swenson, Lourenco and Beaudoin10,Reference Wilkinson and Sanderson11,Reference Chiou, Lev-Toaff and Masuda13 If one of these less specific findings is present on CT, specialty consultation is recommended.
- 6.
Is there a definitive critical time of ischemia for the ovary?
Ovarian torsion is a time critical diagnosis, and suspicion of ovarian torsion based on history and examination warrants consultation with a gynecologist or surgeon, even if imaging is negative for torsion. Lymphatic and venous obstruction occur before arterial obstruction, and the ovaries possess dual vascular supply.Reference Houry and Abbott2,Reference Ghandehari, Kahn, Tomlinson and Glanc14 Thus, patients may experience symptoms of torsion, but arterial flow may not yet be compromised. Literature evaluating ovarian viability in the setting of torsion suggests patients may have a median of 3 days with symptoms (with a range of 0–60 days) and retain ovarian viability.Reference Houry and Abbott2 While ovarian torsion remains a time critical diagnosis, ovarian viability varies. The critical ischemia time for human ovaries is unknown, and the duration of symptoms should not determine whether the ovary is salvageable.
SUMMARY/CONCLUSIONS
Ovarian torsion occurs with twisting of the vascular pedicle, resulting in ovarian ischemia and potentially necrosis. It may affect women of all ages and has a variable presentation. History and physical examination should not be used to exclude the diagnosis. Ultrasound is the first-line imaging modality, but if obtained, CT of the abdomen/pelvis may reveal several findings suggestive of ovarian torsion. Gynecology or surgery should be consulted if ovarian torsion is suspected.
CASE RESOLUTION
The emergency clinician provides antiemetics and analgesics to the patient. An ultrasound is obtained, which reveals an enlarged ovary, peripherally displaced follicles, and abnormal venous flow but normal arterial flow. The emergency clinician speaks with the gynecologist, who evaluates the patient and takes her to the operating room based on the history, examination, and ultrasound.
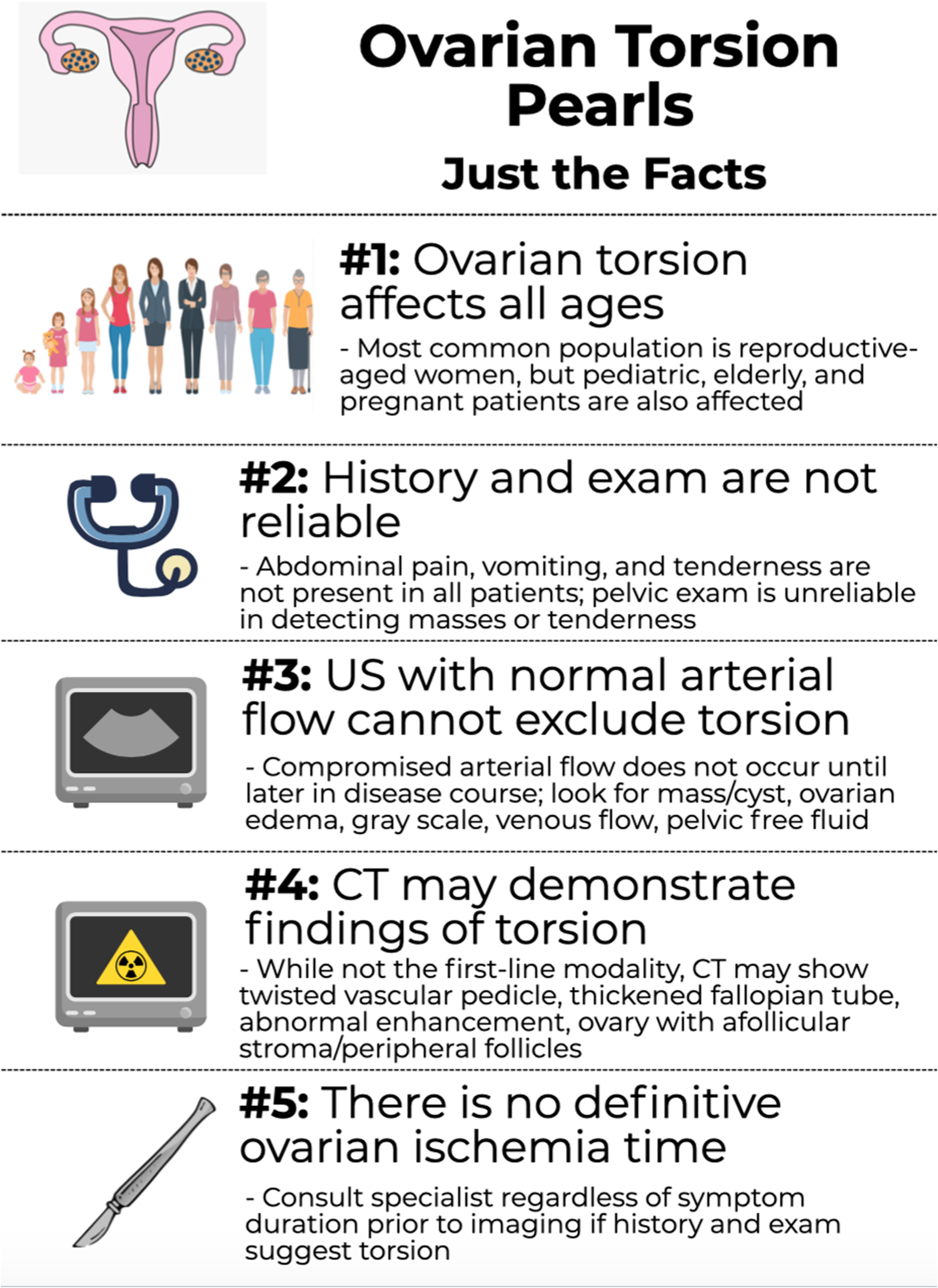
Infographic. Ovarian torsion pearls.
Competing interests
None.
Acknowledgements
B.L., E.T., and A.K. conceived the idea for this manuscript, obtained permission for submission from Dr. Paul Atkinson, and contributed substantially to the writing and editing of the review. This clinical review has not been published, it is not under consideration for publication elsewhere, its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out, and that, if accepted, it will not be published elsewhere in the same form, in English or in any other language, including electronically without the written consent of the copyright-holder. This review does not reflect the views or opinions of the U.S. government, Department of Defense, U.S. Army, U.S. Air Force, or SAUSHEC EM Residency Program.
Financial support
This manuscript did not use any grants or funding, and it has not been presented in abstract form.



