Introduction
The epidemic of overweight and obesity in children observed in recent years calls for a better understanding of the associated risk factors( Reference Lobstein and Millstone 1 ). It is generally accepted that the main lifestyle factors related to the rising prevalence of obesity derive from an imbalance in energy homeostasis caused by increased energy intake and/or sedentary behaviour. Despite lifestyle-based campaigns and interventions in children, adolescents and their parents, the prevalence of obesity has not decreased( Reference Waters, de Silva-Sanigorski and Hall 2 ). Therefore, new approaches are needed for prevention and treatment.
The potential role of psychological and emotional distress in obesity development has been less extensively researched( Reference Hemmingsson 3 ), but a generally positive relationship was found between negative affect or stress in children and weight gain (see Table 1)( Reference Goodman and Whitaker 4 – Reference Wickrama, Wickrama and Lott 27 ). This is particularly relevant because mental disorders affect 10–20% of children and adolescents worldwide( Reference Kieling, Baker-Henningham and Belfer 28 ) and 47·7 % of the children in a European study presented psychosomatic or emotional symptoms( Reference Vanaelst, De Vriendt and Ahrens 29 ). Being more vulnerable to develop mental disorders or being more susceptible to stress could be followed by a poor emotion regulation (ER)( Reference Aldao and Nolen-Hoeksema 30 ). As it has been suggested in adult populations, a poor ER may entail the use of maladaptive strategies to manage with emotions for example, by using food( Reference Michopoulos, Powers and Moore 31 – Reference Taut, Renner and Baban 33 ). Since the manner how they deal with emotions might contribute to obesity, children should acquire efficient emotion management at an early age. Research into the relationship between ER and energy homeostasis could be extremely useful for designing preventive and treatment-based obesity programmes.
Table 1 Overview of studies about child and adolescent stress and negative affect as predictors of weight gain/overweight/obesity: prospective studies
CES-D, Center for Epidemiologic Studies Depression Scale; CBCL, Child Behaviour Checklist; PSS, Perceived Stress Scales; STAIC, State–Trait Anxiety Inventory for Children; CDI, Children’s Depression Inventory; SADS, Shedule for Affective Disorders and Schizophrenia, K-SADS-E, Kiddie-Schedule for Affective Disorders and Schizophrenia Epidemiologic version; K-SADS-P, Kiddie-Schedule for Affective Disorders and Schizophrenia Present Episode version; K-SADS-PL, Kiddie-Schedule for Affective Disorders and Schizophrenia Present and Lifetime version; DSM, Diagnostic and Statistical Manual of Mental Disorders; SCARED, Screen for Child Anxiety Related Emotional Disorders; MINI-KID, MINI-International Neuropsychiatric Interview for Children and Adolescents; MFQ, Mood and Feeling Questionnaire; SDQ, Strengths and Difficulties Questionnaire; RYM, Rotterdam Youth Monitor; CSI, Child Symptom Inventory; CAPA, Child and Adolescent Psychiatric Assessment; DISC, Diagnostic Interview Schedule for Children; SPIKE, Structured Psychopathological Interview and Rating of the Social Consequences for Epidemiology.
The present review discusses current literature on ER and obesity in childhood. Based on a non-systematic and narrative review, we present a novel conceptual framework for the role of ER in weight gain and obesity, discussing the potential underlying factors and their implications for prevention and treatment.
Emotion regulation
Definition of emotion regulation
ER is a growing field within psychology and holds a central role in all the psychological areas including health, development, clinical, social and personality as well as in a variety of other disciplines( Reference Gross 34 ). ER can be broadly defined as the set of strategies used to maintain a positive affective status or improve or suppress a negative affective status in stressful and non-stressful circumstances( Reference Compas, Jaser and Dunbar 35 , Reference Gross 36 ). Nevertheless, there is no single, unified approach of ER. One of the first definitions was given by Thompson( Reference Thompson 37 ), who defined ER as ‘the extrinsic and intrinsic process by which individuals are able to monitor, evaluate and modify their emotions to accomplish their goal’( Reference Thompson 37 ). This concept has been amplified to describe a process for modifying and maintaining feelings, behaviours and psychological features of emotions. In other words, ER refers to attempts to influence which emotions one has and how one experiences or expresses these emotions( Reference Gross 34 , Reference Gross 38 ). Also, the Adaptive Coping with Emotions (ACE) model has explained how emotion dysregulation can occur and provided tools to enhance effective ER( Reference Berking and Whitley 39 ). This new model is based on the acquisition of skills which help to maintain or restore mental health and to address aversive emotions. To summarise, ER is a common process that depends on certain skills and is frequently used in daily life to ensure personal well-being.
Psychological factors related to emotion regulation
ER is related to and interacts with other psychological factors. According to Gross( Reference Gross 34 ), ER along with coping and mood regulation concepts shape the affective regulation term. Coping is understood as responses to alleviate stress, whereas ER is conceptualised as an ongoing process that occurs under both stressful and non-stressful circumstances and is organised around specific emotions (i.e. sadness, fear, anger) and includes efforts to up- or down-regulate both positive and negative emotions( Reference Compas, Jaser and Dunbar 35 , Reference Gross 36 ). In contrast, mood refers to less specific and longer-lasting experiences and seems to be influenced by cognition more than by behaviour processes. Mood regulation may be distinguished from ER by its predominant focus on altering subjective feeling states( Reference Gross 34 ). Therefore, it is suggested that there is a considerable overlap among these regulatory processes( Reference Gross 34 ).
Other factors are executive functions, which are important in the management of cognitive and behavioural processes including working memory, reasoning, task flexibility, inhibition capacity and impulsivity, problem solving, planning and execution( Reference Royall, Lauterbach and Cummings 40 ). Some studies have reported a direct link between executive function abilities and specific ER capacities( Reference Gyurak, Goodkind and Kramer 41 ). Interestingly, impairments of executive function have been reported in overweight adults( Reference Fitzpatrick, Gilbert and Serpell 42 ) and also in children( Reference Schwartz, Leonard and Perron 43 , Reference Blanco-Gómez, Ferré and Luque 44 ) since it might contribute to eating styles( Reference Groppe and Elsner 45 ). Indeed, childhood disorders characterised by impaired executive function, such as attention-deficit/hyperactivity disorder, are associated with overeating and obesity( Reference Dempsey, Dyehouse and Schafer 46 , Reference Erhart, Herpertz-Dahlmann and Wille 47 ).
Self-regulation is a key factor related to ER and executive function that can be understood to include effortful control and impulsivity control. The concept of effortful control encompasses the abilities to inhibit or activate behaviours for the benefit of long-term goals; impulsivity is characterised by high reward sensitivity and a high deficit of response inhibition. These factors have a direct relationship with dietary restraint, in which efforts are made to suppress reward-based impulses to eat in pursuing long-term weight goals( Reference Johnson, Pratt and Wardle 48 ). Several studies in children have found that an increase in impulsivity, a decrease in inhibitory control and a higher reward sensitivity are associated with unhealthier food choices and overweight( Reference Batterink, Yokum and Stice 49 – Reference Pauli-Pott, Albayrak and Hebebrand 53 ).
Emotion regulation in children
Childhood and adolescence are two critical periods in the development of executive function, behaviour-regulation skills and consequently ER strategies. However, newborns and infants are capable of regulating their emotions. From the first days of life, using a neonatal self-regulation assessment, individual differences have been found in controlling negative emotions in a stressful environment( Reference Perez-Pereira, Fernandez and Gómez-Taibo 54 ). At preschool age, children acquire a large range of strategies to manage their own mood and this ability is established in adolescence( Reference Zeman, Cassano and Perry-Parrish 55 ).
Parental influence is essential in the process of ER development, where parents serve as role models and influence the family atmosphere( Reference Morris, Silk and Steinberg 56 ). Children learn ER skills early through interactions with their parents or caregivers, as well as through family factors like family expressivity or communication( Reference Gresham and Gullone 57 ). Also, a negative parental response to children’s emotions teaches children to avoid rather than understand emotions and has been linked to inappropriate ER strategies( Reference Jones, Eisenberg and Fabes 58 ). Parenting styles characterised by ‘high warmth and high control’ have an influence on children’s effective ER leading to greater self-efficacy, self-discipline and successful dealing with challenges( Reference Morris, Silk and Steinberg 56 , Reference Baumrind, Larzelere and Owens 59 ).
ER is essential to healthy psychological functioning. In children, it is an important predictor of risk behaviours( Reference Dickstein and Leibenluft 60 , Reference Wills, Pokhrel and Morehouse 61 ) and mental problems( Reference Dickstein and Leibenluft 60 ), particularly those related to emotional problems( Reference Braet, Theuwis and Van Durme 62 ). Children who do not develop adequate ER strategies will be less able to survive in new environments where they face conflicts. The use of maladaptive ER can generate a vicious circle, since it may increase negative emotions which are involved in developing maladaptive strategies( Reference Berking and Whitley 39 ).
Emotion regulation skills
According to the theory of adaptive coping cited above( Reference Berking and Whitley 39 ), adaptive ER is conceptualised as a situation-dependent interaction between ER skills. The regulatory skills in this model are: awareness of emotions (i.e. the ability to identify and label emotions), understanding emotions (i.e. the ability to identify the causes and maintaining factors of emotions); acceptance and tolerance (i.e. the ability to accept and tolerate negative emotions when necessary); self-support and self-compassion (i.e. the ability to provide effective self-support and self-compassion in distressing situations by self-soothing, self-encouragement and active self-coaching); modifying emotions (i.e. the ability to modify emotions in an adaptive way, which includes self-efficacy) and readiness to confront (i.e. the ability to address situations likely to cause negative emotions). Enhancing or acquiring these skills helps in maintaining or restoring mental health and in approaching aversive emotions( Reference Berking, Poppe and Luhmann 63 ).
A new model for the role of emotion regulation in obesity development
A discussion of findings in the field of ER and obesity is synthetised to provide evidence for the proposed model of the role of ER in obesity prevention and treatment. A schematic illustration of this model is given in Fig. 1.
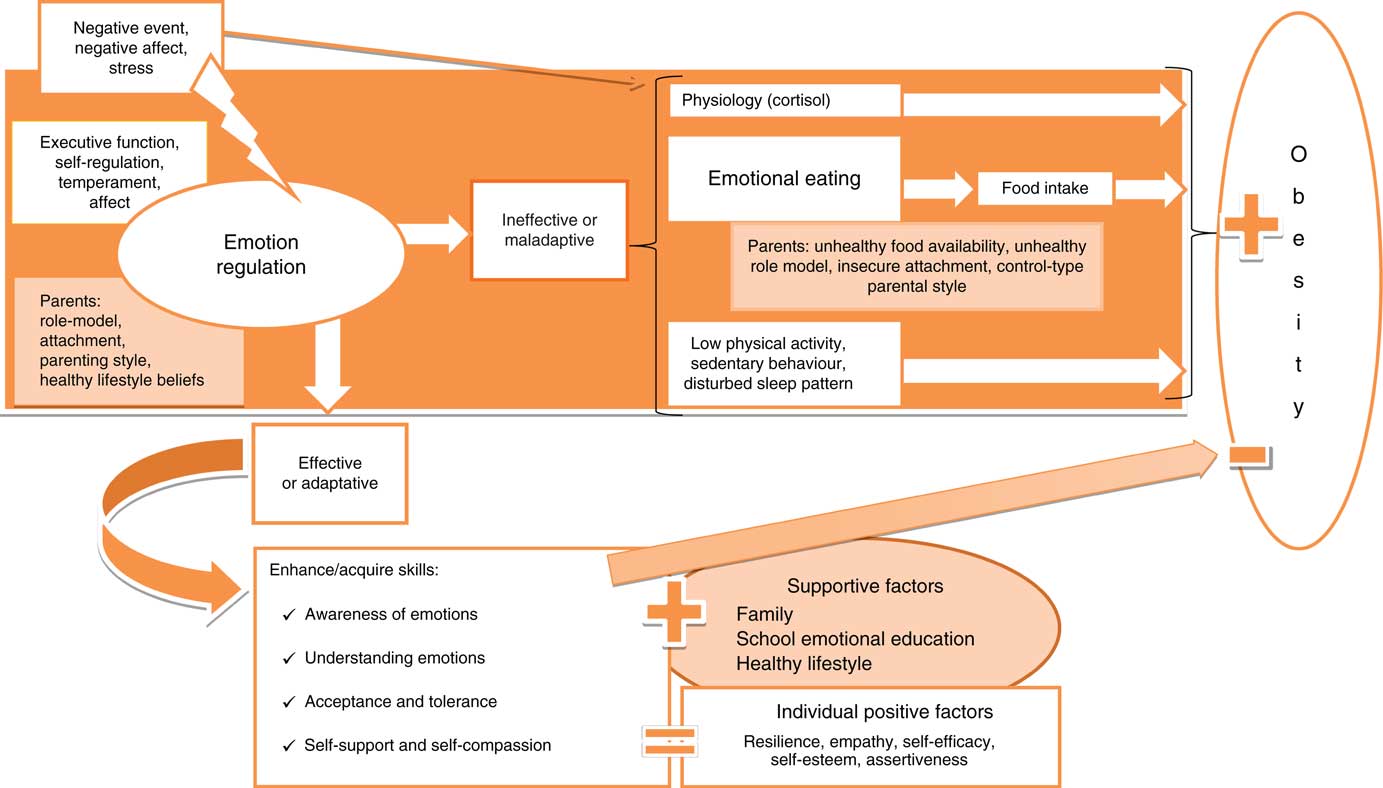
Fig. 1 Conceptual framework for the role of emotion regulation in the prevention and treatment of childhood obesity. For a colour figure, see the online version.
ER strategies have been classified as ineffective/maladaptive v. effective/adaptive, based on their immediate effects on affect, behaviour and cognition( Reference Aldao and Nolen-Hoeksema 30 , Reference Wedig and Nock 64 ). Presence of stress or negative life events could cause emotional dysregulation and therefore increase the vulnerability to develop maladaptive ER strategies in modulating the negative emotion. Thus, it is not only the fact that individuals experience negative emotions but also the way in which they cope with them that may determine the emotional impact on weight gain.
Only very few observational studies have assessed the relationship between ER and obesity in children. Therefore, related factors such as executive function and self-control, which include similar aspects of ER, have also been included in the overview shown in Table 2 ( Reference Graziano, Calkins and Keane 51 , Reference Graziano, Kelleher and Calkins 52 , Reference Isasi, Ostrovsky and Wills 65 – Reference Hughes, Power and O’Connor 71 ). Although the evidence is modest, better ER-related skills were associated with a healthier diet (more fruit/vegetables and less snack food, although not all studies reported significant findings), higher physical activity and, in some cases, a healthier weight status.
Table 2 Emotion regulation or related terms as predictors of childhood weight gain/overweight/obesity: observational studies
YAQ, Youth Adolescent Questionnaire; CBCL, Child Behavior Checklist; BRIEF-SR, Behavioural Rating Inventory of Executive Function−Self-Report Version; CEBQ, Child Eating Behaviour Questionnaire; CBQ, Children’s Behavior Questionnaire.
Physiological mechanisms leading to obesity
Studies have shown that stress can increase overweight and the related adverse metabolic consequences through neuroendocrine changes( Reference Pervanidou and Chrousos 72 ). Repeated activation of the hypothalamic–pituitary–adrenal (HPA) axis mediates stress responses and increases cortisol secretion. This chronic cortisol hypersecretion may cause fat to accumulate in the visceral adipose tissues( Reference Charmandari, Tsigos and Chrousos 73 ) through interaction with lipid homeostasis at several levels: lipolysis, adipogenesis, lipogenesis, and the regulation of circulating fatty acids( Reference Peckett, Wright and Riddell 74 ). However, intense acute or chronic stress might also lead to hypo-activation of the HPA axis, or hypocortisolism( Reference Pervanidou and Chrousos 72 ). The cortisol response to stress is complex, but both hypo- and hypercortisolism may be harmful. According to a meta-analysis, HPA activity depends on the personal response to stress, since cortisol output increases with distress and decreases in individuals with post-traumatic acute stress( Reference Miller, Chen and Zhou 75 ). Recent research in schoolchildren indicates that stress is associated with hypercortisolism( Reference Michels, Sioen and Braet 76 ). Additionally, other findings point out that maladaptive ER induces cortisol reactivity( Reference Cris, Opre and Miu 77 ).
Therefore, stress in combination with maladaptive coping strategies could lead to dysregulated cortisol secretion and obesity. Since cortisol is appetite-stimulating, it also increases appetite and the attraction to sweet and fatty foods, mainly by stimulating reward pathways or by influencing other hormones( Reference Michels, Sioen and Braet 76 , Reference Dallman, Pecoraro and Akana 78 ).
Emotional eating: a mediator between emotional dysregulation and obesity
Emotional eating and stress/emotions
In a stressful situation, some individuals will use maladaptive coping strategies such as eating mainly highly palatable and high-energy food to suppress negative emotions and stress( Reference Taut, Renner and Baban 33 ). According to the theory of emotional eating, the eating behaviour to deal with emotions is defined as emotional eating( Reference Bruch 79 ). A poor emotional regulation leads to emotional eating in adults( Reference Michopoulos, Powers and Moore 31 , Reference Evers, Marijn Stok and de Ridder 32 , Reference Spoor, Bekker and Van Strien 80 ). Studies consistently report that emotional eating is often followed by negative emotions, also in children( Reference Goossens, Braet and Van Vlierberghe 81 – Reference Braet and van Strien 85 ). Consequently, emotional eating is the result of self-inability to regulate emotions, and this maladaptive strategy might underlie the relationship between emotional dysregulation and obesity by modifying dietary intake( Reference Francis and Susman 50 , Reference Graziano, Calkins and Keane 51 , Reference Isasi, Ostrovsky and Wills 65 ). Studies in children and adolescents have revealed an association between maladaptive ER strategies and emotional eating( Reference Czaja, Rief and Hilbert 83 , Reference Harrist, Hubbs-Tait and Topham 86 – Reference Kubiak, Vögele and Siering 88 ). However, different maladaptive strategies of ER have been assessed in these studies and this may lead to bias in the results. Harrist et al. ( Reference Harrist, Hubbs-Tait and Topham 86 ) conducted a longitudinal study in 782 children and found that reactivity to anger and worry was consistently related to emotional eating. In this vein, maladaptive ER such as ruminative thinking increased the desire to eat in adolescents( Reference Kubiak, Vögele and Siering 88 ).
Emotional eating and food intake
Emotional eating leads to an unhealthier diet since it is suggested that food with high energy density can ameliorate negative affect or stress( Reference Gibson 89 ). As a result, emotional eating increases the intake of sweet and fatty foods, or ‘comfort food’( Reference Konttinen, Männistö and Sarlio-Lähteenkorva 90 – Reference Péneau, Ménard and Méjean 92 ). In experimental studies, emotional eaters have been found to consume more sweet and fatty foods( Reference Oliver, Wardle and Gibson 93 – Reference Wallis and Hetherington 95 ) in response to stress. Although there are fewer studies of child populations, the conclusions are often similar: emotional eating was associated with high intake of sweet and/or fatty food in both observational( Reference Braet and van Strien 85 , Reference Elfhag, Tholin and Rasmussen 96 – Reference Ouwens, Cebolla and van Strien 98 ) and laboratory studies( Reference Wallis and Hetherington 95 , Reference Moens and Braet 99 – Reference Goldschmidt, Tanofsky-Kraff and Wilfley 101 ). Although these observational studies were cross-sectional, several were conducted on large samples and showed strong association( Reference Elfhag, Tholin and Rasmussen 96 – Reference Moens and Braet 99 ). Moreover, sex appeared to play a role in the effect of emotional eating on food choices since females often tend to eat more sweet and fatty food. However, the possible interaction of sex and age remains unclear.
Emotional eating and obesity
Since emotional eating is related to less healthy dietary intake, it has been longitudinally linked to weight gain and obesity, especially in females( Reference van Strien, Herman and Verheijden 102 , Reference Koenders and van Strien 103 ). Although no significant relationship was observed in a small number of studies( Reference Snoek, van Strien and Janssens 104 ), other studies identified a significant percentage of emotional eating in overweight children( Reference Goossens, Braet and Van Vlierberghe 81 , Reference Braet and van Strien 85 , Reference Braet, Claus and Goossens 105 , Reference Eddy, Tanofsky-Kraff and Thompson-Brenner 106 ). Braet et al. ( Reference Braet, Claus and Goossens 105 ) showed that in a large sample of children and adolescents 10·5 % of overweight children reported high scores of emotional eating. Especially in adolescence, the relationship becomes stronger in overweight females( Reference Braet, Claus and Goossens 105 ) with loss of control( Reference Goossens, Braet and Van Vlierberghe 81 , Reference Eddy, Tanofsky-Kraff and Thompson-Brenner 106 ). Interestingly, obese individuals are also more vulnerable to emotional eating since, according to psychosomatic theory, they are unable to distinguish between hunger and negative emotions as a cause of their desire for food( Reference Kaplan and Kaplan 107 ). In addition, the cognitive load of coping with a negative emotion may overcome the self-regulation process so that obese individuals no longer maintain their self-control. Therefore, emotional eating may have an important role in the development and maintaining of overweight and obesity.
Emotional eating and parental influence
Parents and family members influence children’s food choices not only through food availability, eating patterns at home, and role modelling( Reference Skeer and Ballard 108 ), but also through other processes. Parental feeding practices could lead to unhealthy eating behaviours and childhood obesity( Reference Wehrly, Bonilla and Perez 109 , Reference Rodgers, Paxton and Massey 110 ), since parents can pressure children to eat or restrict their diet or can use sweets as rewards or to change their temperament. Children also learn from their parents’ behaviour, for example by using food to calm negative emotion. A laboratory study conducted on twenty-five preschool children and their mothers showed that children of mothers who use food for ER consume more sweet palatable foods in the absence of hunger( Reference Blissett, Haycraft and Farrow 111 ). Similarly, a cross-sectional study in 497 children and mothers found that maternal feeding behaviours affect emotional eating in children( Reference Bost, Wiley and Fiese 112 ). These practices may have a negative impact on the development of self-regulation of eating, since children learn to use food as a strategy to cope with emotions and are likely to use the same maladaptive emotional eating later in their lives( Reference Blissett, Haycraft and Farrow 111 , Reference Kröller, Jahnke and Warschburger 113 ). Finally, it is strongly supported that certain parenting styles, such as the authority and permissive parenting style, increase the risk of overweight( Reference Baumrind, Larzelere and Owens 59 , Reference Latzer and Stein 114 ), especially those children who fail to delay gratification or have poor self-regulation( Reference Connell and Francis 115 ). Indeed, it has been suggested that ER mediates the relationship of parental attachment with emotional eating or unhealthy food consumption and sedentary activities in children( Reference Vandewalle, Moens and Braet 87 , Reference Bost, Wiley and Fiese 112 ).
Lifestyle: a mediator between emotional dysregulation and obesity
Stress and negative affect are linked to other aspects of obesity-related lifestyle like sedentary behaviour and low physical activity. Children and adolescents with stress or negative affect may perform less physical activity due to decreased motivation and are likely to spend more time on sedentary activities like video games, Internet and television( Reference Ouwens, Cebolla and van Strien 98 , Reference Anton, Newton and Sothern 116 , Reference Reeves, Postolache and Snitker 117 ). A recent review suggests that cognitive abilities and self-regulation may enhance active or inactive physical activity behaviours( Reference Buckley, Cohen and Kramer 118 ). Indeed, a failure in ER or self-regulation might predispose to sedentary behaviour whereas successful self-regulation has been associated with more physical activity( Reference Isasi, Ostrovsky and Wills 65 , Reference Isasi and Wills 66 ). Simultaneously, an individual could perform physical activity to deal with stressful states or negative emotions. In a representative Canadian sample (aged 15 years or over), 40 % reported using exercise for stress coping and these individuals were more likely to use positive coping strategies and less likely to use alcohol or drugs for coping( Reference Cairney, Kwan and Veldhuizen 119 ). Physical activity could play a role as an adaptive coping strategy and also increase well-being and efficient ER skills in adults( Reference Hegberg and Tone 120 ) and adolescents( Reference Ho, Louie and Chow 121 ). This effect could be possible through neuro-hormonal mechanisms but also psychological and sociological aspects( Reference Monshouwer, ten Have and van Poppel 122 , Reference Rees and Sabia 123 ).
Concurrently, stress and disturbed affective states may influence sleep patterns, causing difficulties in falling asleep or sleep disruption( Reference Morin, Rodrigue and Ivers 124 , Reference Vandekerckhove, Weiss and Schotte 125 ). Indeed, a comprehensive review described the bidirectional relationship between stress and sleep problems and their underlying pathways( Reference Kahn, Sheppes and Sadeh 126 ). Ineffective ER strategies appear to be related to sleep disturbances, which reduce sleep quantity and quality. Since sleep problems may be associated with diminished self-regulation of appetite, they can increase the risk of overeating and obesity( Reference Kahn, Sheppes and Sadeh 126 , Reference Burt, Dube and Thibault 127 ). In the other direction, sleep also plays a role in regulating cognitive and emotional processes. Poor sleep may negatively affect the ability of perception, processing and understanding emotional stimuli( Reference Kahn, Sheppes and Sadeh 126 , Reference Alfarra, Fins and Chayo 128 ). A recent laboratory study showed that sleep loss affects adequate attention resources during an emotional task( Reference Alfarra, Fins and Chayo 128 ). As a consequence, adequate sleep patterns could ameliorate negative emotions and be helpful in ER.
Enhancing emotion-regulation skills for prevention and treatment of obesity
Interventions in adults
Several intervention studies and randomised controlled trials have recently been conducted in adults to test the effectiveness of ER strategies in regulating obesity and food intake( Reference O’Reilly, Cook and Spruijt-Metz 129 ). The most frequent strategies are based on the regulatory skills and correspond to new approaches within the cognitive–behavioural psychological therapies. So, mindfulness therapy, acceptance and commitment therapy, self-compassion therapy (loving-kindness therapy), emotionally focused therapy and dialectical behaviour therapy lead to less psychological distress( Reference Compare, Calugi and Marchesini 130 – Reference Mantzios and Wilson 134 ), fewer binge eating episodes( Reference Compare, Calugi and Marchesini 130 , Reference Dalen, Smith and Shelley 131 , Reference Wiser and Telch 135 ), less emotional eating( Reference Alberts, Thewissen and Raes 136 ), fewer food cravings( Reference Alberts, Thewissen and Raes 136 – Reference Forman, Hoffman and Juarascio 138 ), healthier eating patterns( Reference Dalen, Smith and Shelley 131 , Reference Miller, Kristeller and Headings 139 ), weight loss( Reference Dalen, Smith and Shelley 131 , Reference Forman, Butryn and Hoffman 132 , Reference Mantzios and Wilson 134 , Reference Forman, Hoffman and Juarascio 138 ), fewer personal barriers to physical activity( Reference Tapper, Shaw and Ilsley 140 ), and improved self-efficacy to weight loss( Reference Kidd, Graor and Murrock 141 ). Despite a few non-significant findings( Reference Kearney, Milton and Malte 142 ), these strategies are a promising approach for obesity treatment and prevention.
Mechanisms of intervention
Mindfulness therapy encourages individuals to be non-judgmentally aware of and to understand their emotions so that they can avoid maladaptive ER such as emotional eating( Reference Alberts, Mulkens and Smeets 137 ). Acceptance therapy could reduce frustration and food preoccupation because it increases the ability to tolerate aversive internal experiences (i.e. anger or sadness)( Reference Forman, Butryn and Hoffman 132 ). Similarly to these therapies, dialectical behaviour therapy and emotionally focused therapy enhance identification, enabling individuals to accept and modify emotions adaptively. Self-compassion therapy is related to self-support and can help to reduce the sense of threat and stimulate a self-soothing system( Reference Gilbert and Procter 143 ).
The skills used in the several types of therapies are interrelated, and other individual positive factors should be encouraged simultaneously, such as self-empathy, self-esteem, assertiveness, self-efficacy and resilience. For example, self-compassion and mindfulness are related to lower self-criticism since they enhance self-kindness, self-acceptance, self-empathy and self-esteem( Reference Berking and Whitley 39 ). Through self-empathy, we develop a concern for our well-being, learn to be sensitive and tolerant of our distress, and develop a deep understanding of its roots and causes. Self-empathy is negatively associated with negative affect and stress and could help us to deal with weight and food stress in a non-judgemental/critical way and to develop self-warmth( Reference Gilbert and Procter 143 ). Self-esteem also could be a mediator between emotional disorders and obesity( Reference Cortese, Falissard and Angriman 144 ), since low self-esteem in childhood predicts weight gain( Reference Ternouth, Collier and Maughan 24 ). So, good self-esteem could help to enhance self-encouragement and self-coaching, which enables individuals to modify their emotions and to confront negative situations. Along with these skills, assertiveness could be developed and be useful as a strategy of social relation, self-confidence and coping. The ability to analyse and actively modify emotions improves emotional self-efficacy, which reduces stress and avoidance of aversive events. In addition, resilience, which is the capacity to deal successfully with disturbances, is related to awareness, acceptance and tolerance; it decreases vulnerability to negative emotion and boosts self-regulation abilities (i.e. impulse control). This emotional resilience and self-efficacy facilitates a disposition to experience emotionally challenging situations with additional opportunities to strengthen ER skills( Reference Berking and Whitley 39 ). Later, Forman & Butyn( Reference Forman and Butryn 145 ) considered the acceptance-based intervention efficacious for weight control in individuals who are more susceptible to eating in response to internal and external cues (for instance, availability of unhealthy food). These skills included an ability to tolerate uncomfortable internal responses and a reduction of pleasure, behavioural commitment to clearly defined values, and conscience of decision-making process( Reference Forman and Butryn 145 ).
Interventions in children
Systematic reviews of interventions show that successful childhood obesity interventions should be multidimensional, combining traditional strategies with behavioural and psychological approaches( Reference Waters, de Silva-Sanigorski and Hall 2 ). Nevertheless, few interventional studies have focused on emotional factors. One recent review of behavioural interventions reported that only a small number of intervention studies focused on stress management and emotional control training but that these studies were generally effective( Reference Martin, Chater and Lorencatto 146 ). The latter-mentioned ER techniques have been applied in children and adolescents in the field of mental disorders but not in child obesity. Nevertheless, we have highlighted some intervention studies which could use methods with similar features of ER techniques such as calm down and awareness about feelings and deal with emotion in a healthy way.
In the field of childhood obesity prevention focusing on ER, to our knowledge there is only one pilot study and two on-going studies( Reference Riggs, Sakuma and Pentz 147 – Reference Melnyk, Kelly and Jacobson 149 ). A school-based pilot intervention translated specific components of a violence and substance abuse programme into a lifestyle intervention. This pilot programme included seven lessons focusing on teaching tools for controlling impulsiveness, recognising and adaptively dealing with stress, and analysing the effectiveness of possible solutions( Reference Riggs, Sakuma and Pentz 147 ). Although it was a short-term and non-randomised controlled study, the result was a significant change in positive attitudes toward self-regulation of appetite and positive changes in food and lifestyle( Reference Riggs, Sakuma and Pentz 147 ). A randomised clinical trial and prospective study conducted in 779 adolescents and their parents applied a cognitive–behavioural skills intervention combined with nutrition education and physical activity. The programme included four of fifteen sessions on cognitive reappraisal, emotional and behavioural regulation, stress, coping, goal-setting and overcoming barriers to a healthy lifestyle( Reference Melnyk, Kelly and Jacobson 149 ). This intervention indicated a positive impact on physical activity, BMI and psychological outcomes and also after 6 months, the participants had lower BMI( Reference Melnyk, Jacobson and Kelly 150 ). Another school-based intervention study is currently being carried out in toddlers, combining a traditional obesity prevention programme with a programme to enhance self-regulation. The study teaches children tools for behavioural self-regulation and includes a parental intervention( Reference Miller, Horodynski and Herb 148 ).
In childhood obesity treatment, successful intervention studies have applied cognitive–behavioural therapy to encourage the development of effective ER( Reference Boutelle, Kuckertz and Carlson 151 – Reference Moore, Borawski and Cuttler 157 ). One pilot interventional study applied a cognitive–behavioural skills-building programme in primary care services. The programme was carried out through seven telephone and clinical sessions, which included evaluation of emotional responses and behaviour. Although their results did not show an effect on BMI, they observed an increase in physical activity, healthy lifestyle behaviours and nutrition knowledge. Long-term results were mainly attained in children with supportive families( Reference Jacobson and Melnyk 153 , Reference Jacobson and Melnyk 154 ). Another interventional study conducted in thirty-one children aged 6–12 years and their parents showed positive persistent results since anthropometric parameters and energy intake were reduced and family habits and emotional and social problems were improved at 5 years follow-up( Reference Vignolo, Rossi and Bardazza 152 ). Although these studies did not include a control group, their results are promising. Indeed, Sacher et al. ( Reference Sacher, Kolotourou and Chadwick 156 ) developed a randomised controlled trial through a multicomponent community-based childhood obesity intervention based on nutritional and behavioural change in 160 obese children and their parents. The intervention showed a reduction in waist circumference and BMI at 6 and 12 months post-intervention. Therefore, both clinical and community settings now support the development of childhood obesity programmes using ER-related skills.
Implications for prevention and treatment
Our model highlighted the role of ineffective ER in weight gain. Effective ER skills development could reduce vulnerability during emotional problems and distress, and avoid developing maladaptive ER strategies such as unhealthy eating behaviour related to obesity (i.e. emotional eating, sedentary behaviour). Therefore, future studies should urgently explore the impact of ER on obesity prevention and treatment by applying interdisciplinary interventions.
Implications for prevention
Given that the acquisition of healthy ER and dietary habits starts in infancy, prevention strategies should be implemented early in life and target the promotion of mental health, effective ER techniques and healthy lifestyle habits such as eating behaviour. Learning effective ER skills from an early age (i.e. as awareness and understanding emotions, acceptance of emotional distress and to learn to have a tolerance under frustration and negative feelings) could avoid children acquiring and developing maladaptive ER such as emotional eating when they feel overwhelmed by intense emotions or stressful events. These intervention approaches should be applied along with nutritional interventions through family-based community programmes, in primary care or in schools. Since parenting style and parental modelling influence children’s ER and lifestyle, community obesity prevention programmes should provide support to parents for teaching conflict and negative emotion management techniques and also seek to actively involve parents and family members in changing their own behaviour. To integrate this approach into the school setting, teachers can act as health agents and ER, along with healthy eating habits and lifestyle, can be incorporated into the school curriculum. This type of curricular programme should focus on learning and encouraging awareness and understanding of feelings, identifying internal strengths and learning effective ER skills. Of course, ER programmes should be adapted to the children’s age and should include working groups for parents, to reinforce the concepts and techniques that children learn in class and to help the parents face difficult situations they may encounter with their children. One such novel ER approach has been proposed for a school-based obesity prevention programme( Reference Sakuma, Riggs and Pentz 158 , Reference Pentz 159 ).
Implications for treatment
In obesity treatment, public health agents and paediatricians are encouraged to consider traditional weight-loss methods and nutritional recommendations along with ER intervention. Through ER-based intervention, barriers in the treatment progress such as shame and preoccupation with food can be targeted by fostering greater self-soothing, self-esteem, resilience and body acceptance. Additionally, families need to be aware of the emotional distress that overweight children suffer from. Consequently, the family should also be involved in the intervention to learn effective ER and how to resolve potential conflicts with the child.
Limitations in the interpretation of the model
Since the model presented in this study is intended to illustrate the potential role of ER in the development of obesity, other risk factors in the stress–obesity pathway have not been mentioned. First, it has been assumed that the associations between stress and obesity share genetic factors like polymorphism on the serotonin 5-HT2C receptor gene, monoamine oxidase A, serotonin transporter gene or the fat mass and obesity associated gene (FTO gene)( Reference Fuemmeler, Agurs-Collins and McClernon 160 – Reference Velders, De Wit and Jansen 162 ). In addition, a recent review suggested that socio-economic disadvantages and family disharmony are a common starting point for weight gain and psychological distress in children( Reference Hemmingsson 3 ). At the same time, several prenatal, perinatal and postnatal factors (for example, toxics exposure, maternal nutrition, maternal stress, maternal psychopathology and negative events during early life) have been identified as obesity and/or neurodevelopmental risk factors( Reference Wermter, Laucht and Schimmelmann 161 , Reference Provençal and Binder 163 , Reference Entringer, Buss and Swanson 164 ).
Additionally, due to the multifaceted nature of the concept, ER has been discussed in the literature under other terms such as self-regulation, self-efficacy, effortful control, impulsivity and emotional eating. This lack of consistent terminology has hindered the literature search strategy and interpretation of studies.
Conclusion
Stress and negative emotions during childhood pose a major threat to public health, since they have been related not only to psychological disease but also to physiological disturbances such as obesity. Our model posits that ER – the process used to cope with negative emotions – is a fundamental link between childhood stress and obesity. The present review enhances knowledge of the mechanistic pathways between ER and eating behaviour and obesity by condensing existing studies to a visual research framework. Stress, combined with ineffective ER, could already be present in childhood and could cause abnormal cortisol patterns, emotional eating, decreased physical activity, increased sedentary behaviour and the onset of sleep problems. A healthy lifestyle, such as physical activity and adequate sleep, could show benefits on ER and in developing adaptive ER strategies. Parents also influence the development of ER and obesity in children, as role models and through their parenting style and parental feeding practice. Effective ER skills could decrease obesity-related unhealthy behaviour and enhance protective factors, which boost mental and physical health. As a result, effective ER could contribute to the prevention and treatment of childhood obesity. Although the literature is limited in child populations, some observational studies but few interventional studies on this relationship have been published whose findings are modest but promising. We proposed that psycho-educative intervention in ER training could increase the efficacy of prevention and treatment programmes of obesity. Therefore, encouraging adaptive ER could be an effective new approach, along with nutritional and physical activity intervention, in the fight against and the treatment of childhood obesity. Also, developing an effective ER could have effects on other health issues such as better well-being and preventing psychological problems in children. Based on the literature addressing the adult population, possible successful therapies include mindfulness-based stress reduction therapy, acceptance and commitment therapy or self-compassion therapy. Furthermore, protective factors could be stimulated, such as resilience, assertiveness, empathy, self-efficacy and self-esteem. Future ER interventions are needed to confirm the validity of this model in children. Scientists in the nutritional area should be encouraged to conduct more interdisciplinary studies on this nutrition- and obesity-related topic.
Acknowledgements
There is no relevant funding or sponsorship disclosures from any of the authors.
The authors’ contributions to the manuscript were as follows: N. M. initiated the research question and approach; E. A. performed the literature searching and wrote the drafted manuscript; N. M., J. C., V. A. and S. D. H. provided supervision and critical revision of the manuscript. All authors read and approved the final version of the manuscript.
All authors declare no conflicts of interest.





