Mental disorders are set to become the major causes of disability worldwide Reference Mathers and Lopez1 and are the leading cause of invalidity benefit in the UK. Reference Henderson, Glozier and Holland2 Individual placement and support (IPS) is a form of vocational rehabilitation based on eight principles (Box 1) including individualised job finding and rapid, direct placement without prolonged and structured preparatory rehabilitation. Reference Bond and Kukla3,Reference Bond and Kukla4 It has consistently demonstrated greater success than stepwise rehabilitation, roughly doubling open employment rates over an 18-month follow-up. Reference Bond, Drake and Becker5 Consequently, it is recommended as the evidence-based intervention in a number of countries Reference Latimer, Lecomte, Becker, Drake, Duclos and Piat6–Reference Hoffmann, Jäckel, Glauser and Kupper8 and several US states and it is government policy in the UK. 9 Despite these policy recommendations implementation is patchy. This is in part because IPS's fixed caseloads (25 clients per IPS worker) and no-discharge policy restrict access and increase service costs although Latimer and colleagues Reference Latimer, Bush, Becker, Drake and Bond10 have reported a flexible interpretation of this policy in US services with considerable variation in turnover and discharge. In the EQOLISE Reference Burns, Catty, Becker, Drake, Fioritti and Knapp11 study of IPS in Europe, first employment was noted to be predominantly achieved during the first 9 months of intervention with many fewer in the subsequent nine. A similar early clustering has been reported in the ENDEAVOUR trial (in press BJPsych). We therefore decided to test a shortened form of IPS in which job-seeking support was limited to 9 months and support to those who acquired employment to 4 months. Those failing to obtain employment were referred back to their mental health team with an open invitation for re-referral. A similar offer of re-referral was made to those employed. Our hypothesis was that time-limited IPS (IPS-LITE) would be marginally less effective than IPS but that the increased throughput would result in more patients overall obtaining employment with the same staff input. It would therefore become more cost-effective.
Key principles of IPS are:
-
(a) focus on competitive employment;
-
(b) no exclusion criteria;
-
(c) rapid job search;
-
(d) integration with mental health team;
-
(e) attention to client's job preferences;
-
(f) time-unlimited support;
-
(g) benefits counselling; and
-
(h) active job development.
Method
Design and setting
The trial was an individual-level unblinded randomised controlled trial of IPS-LITE versus standard IPS. The setting was a non-statutory mental health service in Oxford (RESTORE) funded by local commissioners and which offers a range of programmes for individuals with mental health problems (www.restore.org.uk). RESTORE had been operating a limited IPS service for 2 years and received a contract for an expansion to four full-time IPS workers to accept referrals from Oxfordshire Community Mental Health Teams (CMHTs). Enrolment of accepted patients into the IPS-LITE trial and its evaluation was a condition of the contract. The four IPS workers received internal training and supervision, and each was allocated to regular liaison meetings with either one or two CMHTs from whom they received their referrals. The trial was approved by the National Research Ethics Service Isle of Wight, Portsmouth and South East Hampshire Research Ethics Committee Ref. no. 09/H0501/53. Trial registration: ISRCTN28876952.
Participants
Eligible patients were (a) in contact with their CMHT for a minimum of 6 months and expected to remain in outpatient follow-up, (b) aged 18–65 years, (c) unemployed for a minimum of 6 months and (d) seeking employment in the open market.
Recruitment and randomisation
The four IPS workers met regularly with their allocated CMHTs to raise awareness of the service and relied on CMHT staff to refer potential patients. Referred patients were assessed by the IPS worker for their motivation for obtaining employment before being offered the service. Those found not to be motivated for open employment were often redirected to alternative supports or referred back to the CMHT. If offered IPS they had the difference between IPS and IPS-LITE explained by the IPS worker and if they consented to the trial then their details were forwarded to an independent statistician who conducted the randomisation. A non-deterministic minimisation algorithm Reference Pocock12 was used to produce treatment groups balanced for five factors: age <38 yrs v. ≥38 yrs (EQOLISE median age), gender, diagnosis (psychosis versus non-psychosis), duration of illness (<5 yrs v. ≥5 yrs) and previous employment (previously employed versus never employed). The first 2 patients were allocated using simple randomisation to avoid predictability. Subsequently, the minimisation algorithm was applied with an allocation ratio that is not fully deterministic: there was an 80% bias in favour of allocations that minimise the imbalance. If the marginal totals for the groups were the same at a given point, simple randomisation was then used.
IPS workers started their treatment without waiting for either randomisation or the baseline research interview, as there was no difference in initial practice. Blinding was not possible for the patient, the IPS worker or the independent researcher.
Outcome measures
Primary outcome measure
Employment in the open market for at least 1 day during the 18 months follow-up period. This is the internationally used measure in IPS outcome studies.
Secondary outcome measures
Vocational outcomes. Employment in the open market for at least 13 weeks. This is the outcome used for employment statistics by the UK National Audit Office. 9
-
(a) Time to first employment.
-
(b) Number of days worked.
-
(c) Duration of longest employment (job tenure).
Clinical and social outcomes
-
(a) Psychiatric hospitalisation (Yes/No).
-
(b) The Hospital Anxiety and Depression Scale is a self-reported scale which assesses adverse anxiety and depression states by 14 items, each with range from 0 (no symptom) to 21 (severe symptoms). Reference Zigmond and Snaith13
-
(c) The Brief Psychiatric Rating Scale is a researcher-rated scale of symptom severity on 24 domains (ranging from 24 (not present) to 168 (severe symptoms)). Reference Lukoff, Nuechterlein and Ventura14
-
(d) The Manchester Short Assessment of Quality of Life (MANSA) assesses self-reported quality of life on 16 items with total score for 12 ‘subjective’ items ratings ranging from 12 (could not be worse) to 84 (could not be better). Reference Priebe, Huxley, Knight and Evans15
-
(e) Euro-QoL is a self-reported, standardised measure of health-related quality of life on five dimensions. Reference Brooks16
-
(f) Camberwell Assessment of Needs, Short Appraisal Schedule, research version assesses clinical and social needs with 22 items (ranging from 0 (no problem) to 22 (serious problem/unmet needs)). Reference Phelan, Slade, Thornicroft, Dunn, Holloway and Wykes17
-
(g) Social Outcomes Index summarises objective indicators of social outcomes in one overall score (range 0–6). Reference Priebe, Watzke, Hansson and Burns18
-
(h) Global Assessment of Functioning (GAF) is a researcher-rated, single-item scale of impairment in functioning with range from 1 (severe impairment) to 100 (superior functioning). Reference Goldman, Skodol and Lave19
Process evaluation
All contacts with the IPS service were obtained from the IPS service record by researchers to confirm both the number and timing of contacts. Discharge dates from the service were obtained from RESTORE records. In a minority of patients without a recorded discharge but over 3 months without any contact directly preceding the final outcome assessment, the date of discharge was taken as the last contact. Dates of employment were obtained from the patient at the structured research interviews at 9 and 18 months. For patients not interviewed, primary and secondary outcome data were collected by phone or letter.
Statistical analysis
Before modelling, the data were checked for differences between allocation groups for all baseline characteristics using the appropriate test (chi-square test, t-test or Wilcoxon Rank Test), demonstrating no statistical significant differences between groups. The primary outcome was analysed using a logistic regression model to produce the effect size as an adjusted odds ratio with 95% CI. Secondary binary vocational outcomes were also analysed using a logistic regression model. Count outcomes (number of days worked, job tenure and number of contacts with service) were analysed using an adjusted negative binomial model that accommodated for the overdispersion and the results presented are rate ratios with 95% CIs. Treatment effects were estimated using hierarchical models with a random patient intercept. The effect sizes were adjusted for stratification factors.
The two survival curves (time to first job and time to discharge) were calculated using non-parametric Kaplan-Meier method. The corresponding adjusted hazard ratios (HRs) and 95% CIs were estimated using a Cox Proportional Hazards model. For clinical and social outcome measures, we estimated treatment effect and change over time using hierarchical models with random patient intercept. For all effect sizes presented, the models were adjusted for stratification factors. All analyses were conducted according to the intention-to-treat principle and the results were obtained by using R software version 3.0.2.
Results
Figure 1, the CONSORT diagram, outlines the patient flow. Of 148 consented patients, 123 were randomised, 62 to IPS-LITE and 61 to IPS. The main reason for exclusion (18 individuals) was duration of unemployment of less than 6 months. Of these 123 patients, 115 had a baseline interview with a researcher (IPS-LITE = 58 and IPS = 57) and 91 at 18-month follow-up (IPS-LITE = 48 and IPS = 43).

Figure 1 Trial profile
IPS, individual placement and support; IPS-LITE, time-limited IPS.
Table 1 presents the baseline data for the participants showing there are no significant differences in baseline characteristics between the two groups. This was an early middle-aged group (mean 38 years), slightly more male subjects (59%), 85% white and 83% born in the UK. They had been ill for an average of 10 years and 58% were diagnosed with a psychotic disorder. Virtually, all (97%) had worked at some time in the past and they had been currently unemployed for a median of 24 months.
TABLE 1 Patient characteristics at baseline
| Total sample (n = 123) | Missing data | IPS-LITE (N = 62) | IPS (N = 61) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean Median n |
(s.d.) [IQR] % |
n | (%) | Mean Median n |
(s.d.) [IQR] % |
Mean Median n |
(s.d.) [IQR] % |
|
| Demographics | ||||||||
| Age, years | 38 | [30.0, 47.0] | 0 | (0%) | 39 | [29.3, 48.0] | 38 | [32.0, 46.0] |
| Male | 72 | (59%) | 0 | (0%) | 35 | (56%) | 37 | (61%) |
| General education, years | 13 | [11.0, 14.0] | 5 | (4%) | 13 | [12.0,14.0] | 13 | [11.0, 13.0] |
| Entered tertiary education | 49 | (40%) | 5 | (4%) | 29 | (47%) | 20 | (33%) |
| Ethnicity | ||||||||
| White | 102 | (85%) | 3 | (2%) | 55 | (90%) | 47 | (80%) |
| Other | 18 | (15%) | – | – | 6 | (10%) | 12 | (20%) |
| Born in the UK | 99 | (83%) | 4 | (3%) | 51 | (84%) | 48 | (83%) |
| Living situation | ||||||||
| Married/co-habiting | 25 | (21%) | 2 | (2%) | 14 | (23%) | 11 | (18%) |
| Independent accommodation | 104 | (89%) | 6 | (5%) | 55 | (95%) | 49 | (83%) |
| Living alone | 50 | (43%) | 7 | (6%) | 24 | (42%) | 26 | (44%) |
| Employment statistics | ||||||||
| Worked previously | 119 | (97%) | 0 | (0%) | 60 | (97%) | 59 | (97%) |
| Duration of current unemployment, months | 24 | [12.0, 52.5] | 0 | (0%) | 24 | [10.0, 53.3] | 24 | [12.0, 50.0] |
| Diagnoses | ||||||||
| Psychosis | 71 | (58%) | 0 | (0%) | 36 | (58%) | 35 | (57%) |
| Non-psychosis | 52 | (42%) | 0 | (0%) | 26 | (42%) | 26 | (43%) |
| Psychiatric history | ||||||||
| Duration of illness, years | 10 | [3.5, 17.0] | 0 | (0%) | 12 | [4.3, 18.5] | 8 | [3.0, 16.0] |
| Number of past psychiatric hospitalisations | 1 | [0.0, 3.0] | 1 | (1%) | 1 | [0.0, 3.0] | 1 | [0.0, 2.0] |
| Clinical outcomes | ||||||||
| Brief Psychiatric Rating Scale, | ||||||||
| range 24–168 | 38 | [34.0, 45.0] | 8 | (7%) | 37 | [34.0, 43.0] | 40 | [34.0, 46.0] |
| Global Assessment of Functioning (GAF), | ||||||||
| range 1–100 | 60 | [52.0, 65.0] | 8 | (7%) | 60.5 | [52.0, 67.3] | 59 | [52.0, 63.0] |
| Euro-QoL Index | 0.743 | [0.62, 0.85] | 8 | (7%) | 0.804 | [0.63, 0.85] | 0.725 | [0.62, 0.85] |
| Euro-QoL Visual Analogue Scale | 54.5 | −19.8 | 9 | (7%) | 52.3 | −18.8 | 56.8 | −20.6 |
IPS, individual placement and support; IPS-LITE, time-limited IPS; IQR, interquartile range.
Table 2 presents the employment outcomes. Overall, 51 patients (43%) obtained employment and of these 33 (28%) worked for at least 13 weeks. The median time to first job was 137 days (just over 4 months) and for those who did obtain employment the median duration of employment was 65 days (44 days in IPS-LITE and 74 days in IPS). The median duration for the longest employment was 122 days. In all of these vocational outcomes, the IPS group scored marginally better but in none was the difference statistically significant. Figure 2 shows the time to first job in the two groups. There is no difference in time to employment (HR = 0.90, CI = 0.51–1.58, P = 0.71). Only 11 participants obtained employment after 9 months (4 in IPS-LITE and 7 in IPS).
TABLE 2 Employment and treatment outcomes at 18 months

| Total sample (n = 123) | IPS-LITE (n = 62) | IPS (n = 61) | Effect size (ES) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Median n |
[IQR] (%) |
Sample size |
Median n |
[IQR] (%) |
Sample size |
Median n |
[IQR] (%) |
Sample size |
HR/OR/RR | (95% CI) | |
| Employment outcomes | |||||||||||
| Worked for at least 1 day | 51 | (43%) | 118 | 24 | (41%) | 59 | 27 | (46%) | 59 | OR = 0.82 | (0.38, 1.78) |
| Worked for at least 13 weeks | 33 | (28%) | 118 | 15 | (25%) | 59 | 18 | (31%) | 59 | OR = 0.75 | (0.32, 1.73) |
| For those who worked at least 1 day | |||||||||||
| Number of days to first job | 137.0 | [59.0, 253.5] | 51 | 137.0 | [53.8, 233.5] | 24 | 136.5 | [68.8, 282.5] | 27 | HR = 0.90 | (0.51, 1.58) |
| Number of days worked | 65.0 | [16.0, 112.5] | 51 | 44.0 | [17.3, 108.3] | 24 | 74.0 | [16.0, 123.0] | 27 | RR = 0.94 | (0.51, 1.76) |
| Duration of longest employment, days (includes part-time work) |
122 | [49.0, 232.0] | 51 | 119.5 | [49.8, 202.5] | 24 | 124 | [66.5, 264.0] | 27 | RR = 0.92 | (0.51, 1.65) |
HR, hazard ratio; IPS, individual placement and support; IPS-LITE, time-limited IPS; IQR, interquartile range; OR, odds ratio; RR, rate ratio.
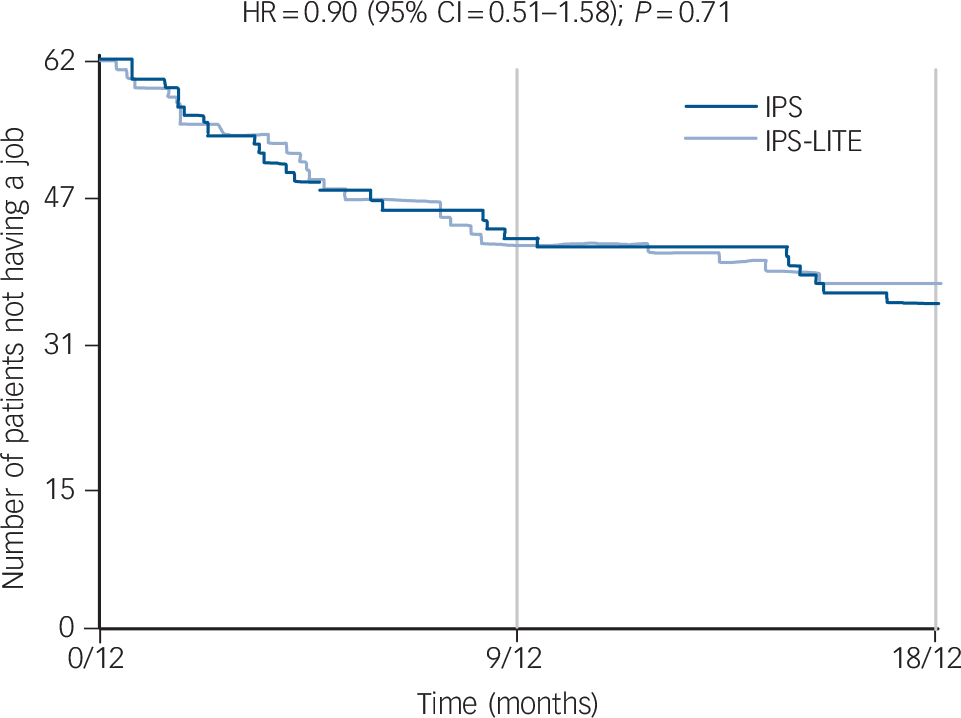
Fig. 2 Time to first job.
HR, hazard ratio; IPS, individual placement and support; IPS-LITE, time-limited IPS
Table 3 shows that there were no significant differences in the clinical or social outcomes. A total of 22 patients were admitted to hospital (10 to IPS-LITE and 12 to IPS) during the 18-month follow-up. Overall symptoms were marginally down and social outcome measures including quality of life, needs etc. were either unchanged or marginally better apart from the GAF which reduced from a mean of 57.9 to 54.3. None of these changes are clinically significant. There are no significant differences in these outcomes between the two arms other than a minor reduction in the 9-month MANSA score.
TABLE 3 Clinical outcomes at baseline, 9 month and 18 months
| IPS-LITE (N = 62) | IPS-STANDARD (N = 61) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean (s.d.) Baseline |
N | Mean
(s.d.) 9-month follow-up |
N | Mean
(s.d.) 18-month follow-up |
N | Mean (s.d.) Baseline |
N | Mean
(s.d.) 9-month follow-up |
N | Mean
(s.d.) 18-month follow-up |
|
| Treatment outcome | ||||||||||||
| Hospital admission during 18 months follow-up, yes |
10 (17%) | 12 (20%) | ||||||||||
| Clinical | ||||||||||||
| Hospital Anxiety and Depression | ||||||||||||
| Scale – Anxiety | 58 | 9.6 (4.08) | 54 | 8.8 (4.10) | 47 | 8.5 (4.31) | 57 | 9.8 (5.31) | 44 | 9.9 (4.92) | 43 | 8.4 (4.53) |
| Hospital Anxiety and Depression | ||||||||||||
| Scale – Depression | 58 | 7.7 (3.62) | 54 | 6.6 (4.22) | 47 | 6.4 (4.34) | 57 | 7.2 (5.03) | 44 | 7.5 (5.59) | 43 | 5.3 (5.10) |
| Brief Psychiatric Rating Scale (BPRS) | 58 | 39.1 (7.73) | 54 | 39.7 (9.80) | 47 | 39.4 (9.73) | 57 | 40.0 (7.19) | 44 | 39.9 (9.98) | 43 | 38.1 (9.13) |
| Social | ||||||||||||
| Manchester Short Assessment of Quality of Life (MANSA) |
58 | 4.1 (0.57) | 54 | 4.3(0.75) | 48 | 4.4 (0.80) | 57 | 4.1 (0.93) | 44 | 3.9 (0.96) | 43 | 4.6 (0.91) |
| Euro-QoL Index | 58 | 0.670 (0.26) | 54 | 0.653 (0.24) | 48 | 0.625 (0.25) | 57 | 0.680 (0.27) | 44 | 0.618 (0.31) | 43 | 0.714 (0.21) |
| Euro-QoL Visual Analogue | ||||||||||||
| Scale | 57 | 52.3 (18.83) | 54 | 60.3 (19.88) | 48 | 59.7 (19.53) | 57 | 56.8 (20.57) | 44 | 54.4 (22.79) | 43 | 66.3 (23.22) |
| Camberwell Assessment of Need | ||||||||||||
| Short Appraisal Schedule | 58 | 7.3 (2.16) | 54 | 6.3 (2.89) | 47 | 6.3 (2.87) | 57 | 7.4 (2.68) | 44 | 7.2 (2.59) | 43 | 5.9 (2.98) |
| Social Outcomes Index | 58 | 3.5 (0.84) | 55 | 3.8 (1.15) | 48 | 3.8 (1.18) | 57 | 3.3 (1.02) | 44 | 3.5 (1.36) | 45 | 4.0 (1.31) |
| Global Assessment of
Functioning (GAF) |
58 | 58.5 (11.65) | 54 | 54.4 (12.68) | 48 | 54.7 (11.49) | 57 | 57.3 (11.19) | 44 | 51.4 (14.71) | 43 | 53.8 (11.81) |
Significant difference between IPS-STANDARD and IPS-LITE (P<0.05) is highlighted. IPS, individual placement and support; IPS-LITE, time-limited IPS.
Discharge and impact on capacity
Figure 3 shows that IPS-LITE patients were rapidly discharged after 9 months. By 18 months, only two of the original patients were still on the IPS-LITE caseload as compared to 42 in IPS. We calculated the potential capacity by summing the days from discharge/disengagement to the 18-month follow-up and dividing by 547 (days in 18 months). This generates the equivalent number of extra places available to take on new patients averaged out over 18 months. In the IPS-LITE group, this amounted to 15 766 days (equivalent to 28.8 extra patients) and in the IPS group it amounted to 4263 days (equivalent to 7.8 extra patients). We then assumed that these new patients would have the same rate of employment as the measured samples (41% in IPS-LITE and 46% in IPS). This is equivalent to 11.81 new jobs in IPS-LITE and 3.64 new jobs in IPS.
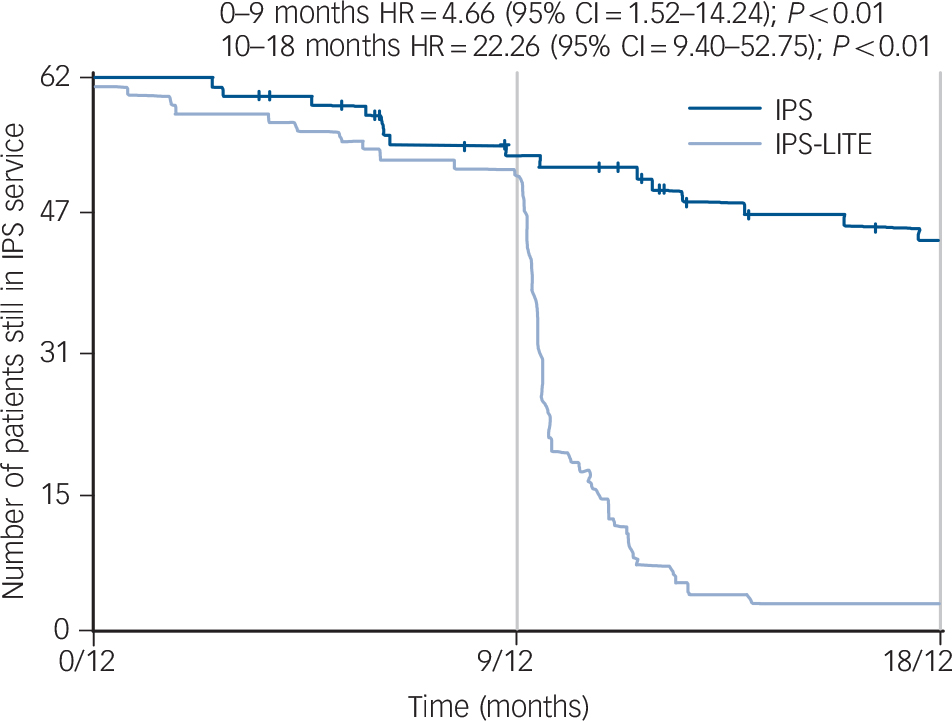
Fig. 3 Time to discharge from IPS service.
HR, hazard ratio; IPS, individual placement and support; IPS-LITE, time-limited IPS.
If all four IPS workers were to regularly fill up their caseloads to the recommended 25 at all times then over a period of 18 months two IPS-LITE workers would provide input to 91 patients and two IPS workers would provide input to 69 patients. Based on the figures derived from this trial (IPS-LITE = 41%, IPS = 46%), the two IPS-LITE workers would get 35.81 patients back into employment and the two IPS workers would achieve 30.64, equivalent to a 17% increase in efficiency.
Discussion
IPS principles include a ‘no-discharge’ policy. Active support is not withdrawn although patients may disengage from services. This no-discharge policy has been found to be difficult to operate in some services Reference Howard, Heslin, Leese, McCrone, Rice and Jarrett20 and powerfully restricts access to IPS in resource-limited public services. Our trial indicates that little is lost in terms of obtaining employment by limiting the duration of involvement of IPS services to 9 months. Of the 51 patients who did obtain employment during the trial, 40 (78%) did so within their first 9 months. Six of the 11 patients who obtained employment after 9 months were no longer in receipt of IPS care – all four of the IPS-LITE patients and two of the seven IPS patients who had disengaged from the service. This leaves only five patients (10%) who can confidently be assumed to have obtained employment as a direct consequence of continuing IPS involvement.
While it is a condition of such services that patients are genuinely motivated for work this may not always remain consistent. Some patients may profess themselves keen for employment and find the reality more daunting than they anticipated. Others may lose their commitment for a range of reasons including changes in their mental state or in family and social circumstances. This cannot be accurately predicted and all patients who entered the IPS-LITE trial, as in other IPS trials, had been assessed to be strongly motivated for employment. Our findings would suggest that there is merit in deciding on a time limit to avoid persisting with patients who are currently unlikely to succeed. Further trials could test whether subsequent re-referral of such discharged patients is successful or not. This would help to disentangle whether the original failure was due to temporary aspects of the clinical condition or reflected more enduring motivational and attitudinal characteristics.
An unanticipated finding in our trial was the six patients who obtained employment without current active input. There are no good data to estimate the likelihood that this is the same as or greater than would have been expected without IPS input. The numbers are small and the clinical characteristics do not permit confidently comparing with other non-input control groups. However, it is worth considering that there may be some enduring effect of the IPS input.
Our findings confirm the utility of the internationally accepted IPS primary outcome measure of one day of open employment. Of the 51 patients who achieved this 33 also achieved the UK employment target of remaining in their job for 13 weeks.
Is IPS-LITE cost-effective?
We have resisted speculative forward-modelling of costs for the two services and restricted ourselves to presenting the data for the 18 months of the study. Our calculated potential 91 patients for two IPS-LITE workers versus 69 patients for two IPS workers is highly conservative. It does not take into account the number of IPS patients who would remain on the caseload yet unemployed beyond the 18 months of the study.
The rate of throughput will diverge markedly in subsequent years as new cohorts of IPS-LITE patients are recruited while the IPS caseload only dwindles slowly. If an IPS-LITE alternative is to be pursued then a more sophisticated cost-effectiveness study with more comprehensive data collection would be indicated. However, the figures we obtain with a potential 17% increase in number of jobs with the same resource would suggest that IPS-LITE may be more cost-effective than routine IPS. A larger and longer trial would be needed to test this definitively.
Conclusions
Our study confirms the growing international literature that IPS as a highly successful form of vocational rehabilitation for individuals with enduring mental health disorders. It also confirms that this can be successfully delivered within non-statutory services that provide adequate staff training and support. A limit of the duration of support to 9 months appears not to significantly reduce the number obtaining employment. Whether limiting in-work support reduces the average duration of employment remains an open question, and our study is not powered to answer this and gives mixed, non-significant results. Staff were easily able to adapt to the adjusted model of care and the improved access with no significant fall-off in effectiveness would suggest that there may be potential improvements in cost-effectiveness that would increase over time. Given current difficulties in implementing IPS in times of austerity, we would recommend that a time-limited model should be the first choice for new services. Different durations should be tested to identify the optimal service configuration.









eLetters
No eLetters have been published for this article.