Cognition, which encompasses memory, attention and problem-solving, plays an essential role for humans in maintaining independent living. Depression is a common mental disorder, with a 31.7% prevalence rate among older adults. Reference Zenebe, Akele, Selassie and Necho1 Poor cognitive function and greater risks of depression have been found in old age, and late-life cognitive decline was detected in middle age. Reference Gao, Geng, Jiang, Huang, Zheng and Belsky2 One recent study found a negative association between cognition and depressive symptoms in worldwide samples of middle-aged and older adults. Reference Li, Wang, Wei, Lu, Wang and Yao3 Researchers have highlighted intertwined trajectories of cognition and depressive symptoms in older adults. Reference Ren, Nie, Du and Liu4 The health implications of both conditions warrant an in-depth investigation of their interrelationships.
The mechanism behind the associations between cognitive decline and depression has been summarised by Bennett and Thomas. Reference Bennett and Thomas5 Early-life depression is a risk factor for later cognitive decline, through alteration of the threshold of manifesting cognitive decline in the brain. Alternatively, cognitive decline could lead to subsequent depressive symptoms via psychosocial dysfunction and enhanced cognition could protect against depression. Reference Cambridge, Knight, Mills and Baune6 Both conditions share similar neurobiological changes, with common risk factors such as physical inactivity, inflammation and vascular issues. Reference Gallagher, Kiss, Lanctot and Herrmann7 Based on data from large-scale panel studies such as the Health and Retirement Study (HRS) and China Health and Retirement Longitudinal Study (CHARLS), longitudinal studies have found temporal bidirectional associations between cognition and depressive symptoms. Reference Wang, Liang, Qiu, Yan, Fang and Shen8–Reference Zhang, Chao, Cai, Bao and Chen10
Random-intercept, cross-lagged panel model
Most of the existing studies were, however, based on latent class trajectory models and cross-lagged panel models (CLPMs) that do not explicitly decompose the effects into between- and within-person components. The extended measurement time lags (2–3 years) of HRS and CHARLS are too long for precise assessment of dynamic within-person relationships. The traditional CLPM has been shown to violate the key assumption regarding stable person-level influences, which would conflate stable between-person effects with dynamic within-person effects and bias cross-lagged effect estimates. Reference Lucas11 Random-intercept, cross-lagged panel modelling (RI-CLPM) decomposes the observed variance into stable between-person differences and temporal within-person dynamics. Reference Hamaker, Kuiper and Grasman12 This approach accounts for stable trait-like differences between individuals and results in unbiased cross-lagged effects that apply exclusively to within-person fluctuations. Reference Usami13 Although RI-CLPM has been applied to bidirectional relationships between cognition and depressive symptoms in large European population-based cohorts, Reference Csajbók, Aarsland and Cermakova14,Reference Nakanishi, Perry, Bejjani, Yamaguchi, Usami and van der Steen15 this analytic approach remains underused in the Chinese context, particularly among middle-aged adults.
Lifestyle and social determinants of cognition and depressive symptoms
Existing literature has identified lifestyle factors associated with cognition and depressive symptoms in later life. First, excessive alcohol drinking and smoking have been linked with cognitive decline and greater depressive symptoms. Reference Listabarth, Groemer, Waldhoer, Vyssoki, Pruckner and Vyssoki16 Second, self-rated health and activities of daily living are associated with cognitive function and depressed mood. Reference Sun, Yang, Ding and Wang17 Recent longitudinal studies have associated work status with cognitive factors and depressive symptoms in working and ageing adults. Reference Schwartz and Borowiec18,Reference Lekha, Azeez, Singh and Irshad19 Third, social engagement and isolation have been linked with cognition and depressive symptoms in older adults. Reference Paiva, Cunha, Voss and Delerue Matos20 Participation in social activities facilitates mental stimulation and emotional support, which protect against depression and cognitive decline. However, existing research has not empirically examined the potential time-varying effects of covariates on cognition and depressive symptoms under the RI-CLPM framework.
Furthermore, existing studies have examined demographic variables such as age, gender and urbanicity as potential moderators in the association between cognition and depressive symptoms. Cognition–depression relationships have been found to vary across gender and living situation, Reference Zhang, Chao, Cai, Bao and Chen10,Reference Wu, Zhang, Chao, Liu and Zhang21,Reference Stephan, Chai, McVey, Sprague, Wolf and Phillips22 and recent studies have revealed age differences and urban–rural disparities in depression and cognitive functioning in both the Western and Chinese context. Reference Brown, Hill and Haider23,Reference Wu, Su, Chen, Zhao, Zhong and Zheng24 Given the potential moderating role of demographic factors, it is essential to explicitly evaluate the moderating role of sociodemographic characteristics in the cognition–depression relationships under the RI-CLPM framework. Such an examination on the moderating role of sociodemographic characteristics could better inform cognitive and mental health disparities and offer a nuanced understanding of the interplay between cognition and depressive symptoms in the Chinese context.
Current study
In view of the research gaps noted above, the present study had three objectives. First, we aimed to examine the bidirectional relationships between cognition and depressive symptoms via RI-CLPM in middle-aged and older adults using updated 10-year data from CHARLS. Second, we examined the effects of sociodemographic characteristics and lifestyle factors on cognition and depressive symptoms via time-invariant and -varying covariates at between- and within-person levels, respectively. Third, we aimed to examine the potential moderating role of gender, age group and urbanicity on cross-lagged effects and the effects of time-invariant covariates in RI-CLPM. The results of the subgroup analysis could provide nuanced findings on group-specific patterns that inform targeted interventions and public health policies for specific sociodemographic subgroups.
Method
Study design and procedures
The present study sample originated from CHARLS, Reference Zhao, Hu, Smith, Strauss and Yang25 which is a population-based panel survey designed to better understand the socioeconomic determinants and health consequences of ageing among middle-aged and older adults in China. CHARLS recruited nationally representative samples of middle-aged and older adults in five waves, from 2011 (wave 1) to 2020 (wave 5). Reference Zhao, Hu, Smith, Strauss and Yang25 The baseline wave (wave 1) was conducted in 2011 using a multistage, stratified, probability-proportionate-to-size sampling method. The baseline survey invited 21 739 eligible adults aged 45 years or above from 450 villages or urban communities to participate in the study in 150 counties or districts across China. A total of 17 500 Chinese middle-aged and older adults from around 10 000 households voluntarily joined and completed the baseline survey, giving an overall response rate of 80.5%.
Among the 19.5% rate of non-responders, 8.8% refused to participate in the survey, 8.2% was due to interviewers’ non-contact of sampled residents and 2.0% for other reasons such as health-related issues. Efforts were made to follow up with participants in subsequent waves to reduce attrition bias. CHARLS adopted a multistage, stratified sampling method by urbanicity and region, and the high response rate ensured that the recruited sample closely resembled the demographic profile of the broader population of middle-aged and older adults in China. These provided empirical support to the representativeness of the sample.
Follow-up interviews were conducted to collect four subsequent waves of data in 2013 (wave 2), 2015 (wave 3), 2018 (wave 4) and 2020 (wave 5) on the original and booster samples, for assessment of temporal changes in participants over time. All participants provided written informed consent, and trained researchers conducted face-to-face assessment interviews using structured questionnaires. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation, and with the Helsinki Declaration of 1975 as revised in 2013. All procedures involving human subjects/patients were approved by the Institutional Review Board at Peking University (no. IRB00001052-11015). Written informed consent was obtained from all participants in all five waves of CHARLS.
Participants
The present study utilised data from all five CHARLS waves by merging the Harmonized CHARLS data-set in the first four waves with those from wave 5. As shown in Supplementary Fig. 1 (available at https://doi.org/10.1192/bjo.2025.10074), in the combined data-set (N = 25,783), 394 individuals were removed in wave 5 because of age <45 years and 964 because of missing responses to cognition and depressive symptoms. The final sample comprised 24 425 individuals with a mean age of 64.5 years (s.d. = 10.8) at wave 5. Half (51.7%) of the respondents were female. Most participants had less than lower secondary education levels (86.6%) and were married (84.7%). Less than half of the sample reported lifetime smoking (44.7%) and 43.3% resided in urban regions.
Measures
Cognition was assessed in CHARLS on five domains from the modified Telephone Interview of Cognition Status (TICS) by trained professional interviewers; TICS is a valid and comparable alternative to the Mini-Mental State Examination for assessment of global cognitive function. Reference Seo, Lee, Kim, Kim, Kim and Kim26 Orientation was measured by naming the year, month, day of the month and day of the week (range 0–4). Visuospatial construction was assessed by reproducing a figure of two overlapping pentagons (range 0–1). The serial-7 test assessed executive function and working memory by serial subtraction of 7 from 100 for five times (range 0–5). Ten random Chinese words were read to the participants, who were then evaluated on the number of correct words that were immediately recalled (range 0–10) and recalled again 4 minutes later (range 0–10). The five components were summed to produce the total cognition score, with higher scores denoting better cognitive function (range 0–30). A previous study has supported TICS as a valid assessment tool of cognitive function in the Chinese population. Reference Meng, Wang, Strauss, Langa, Chen and Wang27 Confirmatory factor analysis found excellent model fits for the 1-factor cognition model for all five waves (comparative fit index (CFI) 0.998–1.000, Tucker–Lewis index (TLI) 0.998–1.000, root mean square error of approximation (RMSEA) 0.004–0.015, standardised root mean square residual (SRMR) 0.002–0.005). The cognition score showed acceptable reliability (ω = 0.69–0.76) across the five waves, with adequate levels of test–retest and interrater reliability in older adults. Reference Desmond, Tatemichi and Hanzawa28
CHARLS uses the ten-item Center for Epidemiologic Studies Depression Scale (CESD-10) to measure the severity of depressive symptoms of participants. A previous study demonstrated adequate factorial validity and reliability of CESD-10 in a baseline CHARLS sample. Reference Chen and Mui29 CESD-10 has shown good convergent validity with other depression scales such as the Beck Depression Inventory and Patient Health Questionnaire. The 10 items were answered on a 4-point Likert scale from 0 (‘rarely or none’) to 3 (‘most or all of the time’). The total CESD-10 score has a theoretical range of 0–30, with higher scores denoting more depressive symptoms. One recent study suggested a cut-off point of ≥10 for CESD-10 score in screening of depression cases. Reference Fu, Si and Guo30 Confirmatory factor analysis found satisfactory model fits for the 1-factor CESD-10 model for all five waves (CFI 0.964–0.978, TLI 0.952–0.971, RMSEA 0.048–0.063, SRMR 0.030–0.034). CESD-10 showed good reliability (ω = 0.75–0.81) across the five waves.
The present study included a range of demographic variables, socioeconomic status, family characteristics and lifestyle factors as time-invariant and -varying covariates in the model. The time-invariant covariates at baseline included three demographic characteristics on age, gender (female and male) and education level (less than lower secondary education, upper secondary education and vocational training and tertiary education), two socioeconomic status variables on total household per capita consumption and rural region (versus urban region), two family characteristics on marital status (married or not) and relationships with parents on a 5-point scale (1, ‘poor’, to 5, ‘excellent’), and one lifestyle factor on lifetime smoking history (smoked or not). The time-varying covariates assessed in each wave included work status (currently working or not) and three time-varying covariates on self-rated physical health on a 5-point scale (1, ‘very poor’, to 5, ‘very good’), frequency of alcohol drinking over the past 12 months on a 10-point scale (0, ‘none’, to 9, ‘more than twice a day’) and participation in social activities in the past month (yes or no).
Statistical analysis
The present study analysed the longitudinal relationships between cognition and depressive symptoms via RI-CLPM. Both cognition and depressive symptoms showed approximate normal distributions (skewness –0.46 to 0.98) with no floor or ceiling effects, and these were modelled as continuous variables in the analysis. To analyse the effects of the COVID-19 pandemic, measures on cognition, depressive symptoms and the time-varying covariates in wave 5 were compared with those in the previous four waves. We specified traditional CLPM with first- and second-order autoregressive effects for comparison. In the first-order autoregressive model (model 1), the measure at wave t was predicted by the most recent measure at wave t – 1. In the second-order autoregressive model (model 2), the measure at wave t was predicted by the two most recent measures at waves t – 1 and t – 2.
RI-CLPM (model 3) was first estimated by the robust maximum-likelihood estimator using structural equation modelling in Mplus 8.11 for Windows (Muthén & Muthén, Los Angeles, California, USA; https://www.statmodel.com/). The large sample size (N >10 000) and five panel waves ensured adequate statistical power for conducting RI-CLPM in the present study. Missing data on cognition, depressive symptoms and other study variables were handled in the analysis using full-information maximum likelihood under the missing-at-random assumption. Community identification was specified as a cluster variable in all analyses, to account for the nested sampling design and adjust standard errors. Statistical significance was set at 0.05.
Figure 1 shows the graphical presentation of RI-CLPM, where C it and D it denote the observed scores of cognition and depressive symptoms of individual i at wave t, respectively. In RI-CLPM, these were decomposed into ‘between’ and ‘within’ components. Reference Hamaker, Kuiper and Grasman12 The between components (BC i for cognition and BD i for depressive symptoms) are the random intercepts that denote stable individual differences. The within components (WC it for cognition and WD it for depressive symptoms) indicate the individual’s deviation from the expected score based on the random intercepts. Among the within components, autoregressive effects estimate the within-person carry-over effects for the same variable (e.g. from WC i1 to WC i2 ). Cross-lagged effects indicate the spill-over effects of cognition into depressive symptoms (e.g. from WC i2 to WD i3 ) and vice versa (e.g. from WD i4 to WC i5 ). A negative cross-lagged effect indicates that a negative deviation from an individual’s expected level of cognition will be followed by a positive deviation in that individual’s expected level of depressive symptoms at the next occasion. Reference Usami13
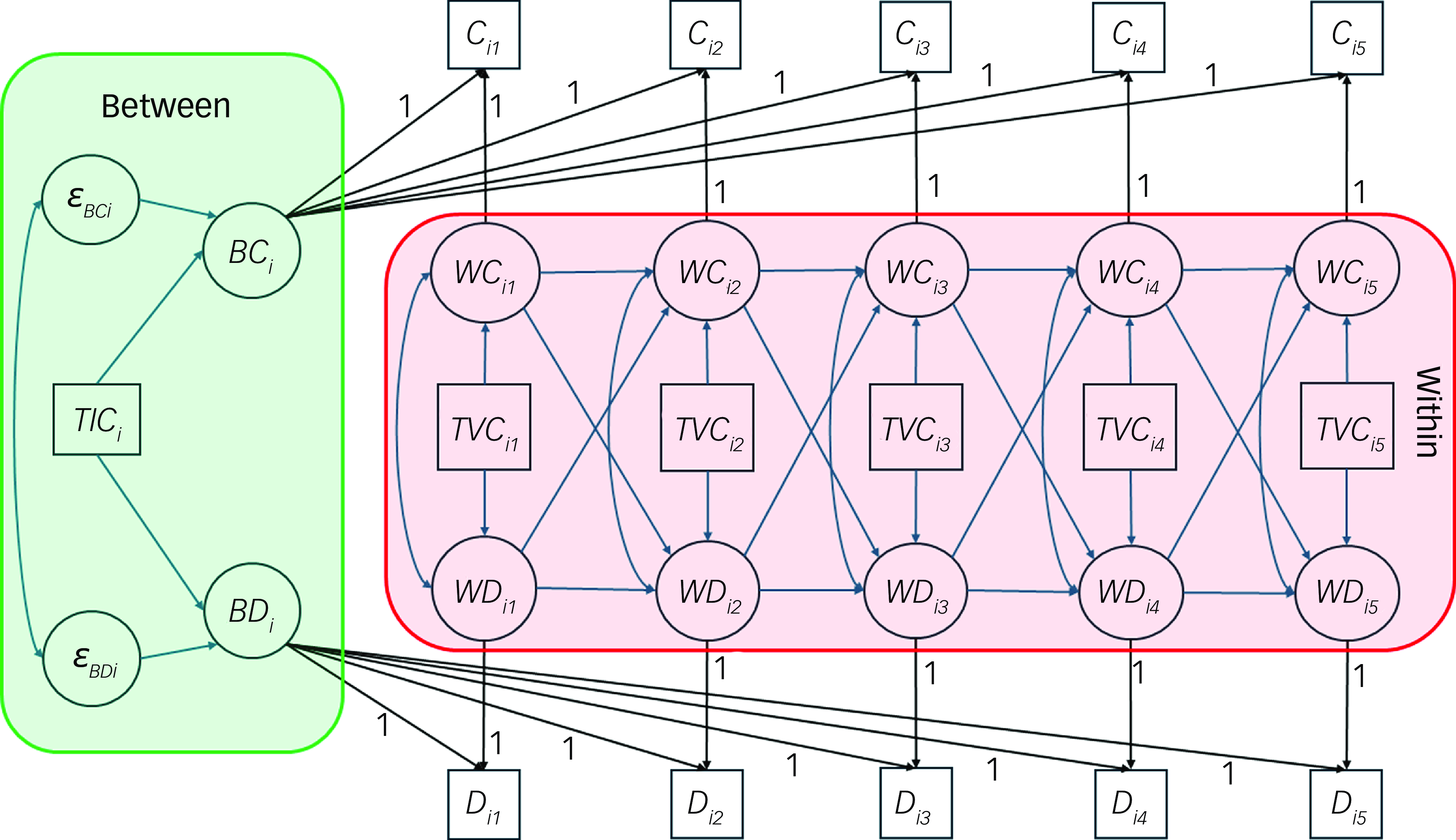
Fig. 1 Graphical depiction of the random-intercept, cross-lagged panel model (RI-CLPM). C it , observed score for cognition of individual i at wave t; D it , observed score of depressive symptoms of individual i at wave t; BC i and BD i , random intercepts for cognition and depressive symptoms, respectively, at the between level; WC it and WD it , within-person components of cognition and depressive symptoms, respectively, of individual i at wave t, indicating that individual’s deviation from the expected score based on random intercepts; TIC, time-invariant covariates; TVC, time-varying covariates; ε, residual variance in between-person components. In RI-CLPM, the observed scores were decomposed into stable between components and changing within components with fixed factor loadings of 1.
Second, we included eight time-invariant covariates (female, age, education level, marital status, rural region, lifetime smoking history, household expenditure in 2011 and relationships with parents) in RI-CLPM as predictors of the between components (model 4). Reference Mulder and Hamaker31 For the within part, we included four time-varying covariates as predictors of the within components. Third, we separately examined the equality of autoregressive effects (model 5), cross-lagged (cross-over) effects (model 7) and the effects of time-varying covariates (model 6) across time in RI-CLPM. We also tested for the equality of cross-lagged effects from cognition to depressive symptoms and vice versa (model 8). Equality was tested by comparing the models with unconstrained and constrained effects. Goodness of fit of RI-CLPM was evaluated using the following criteria: CFI and TLI ≥ 0.95, and RMSEA and SRMR ≤ 0.06. Reference Hu and Bentler32 Comparison between the constrained and unconstrained models was performed via a scaled chi-square difference test, and changes in Bayesian information criterion (BIC) and fit indices (ΔCFI ≤ −0.01 and ΔRMSEA ≥ 0.01). Models with lower BIC indicate a better model fit with greater parsimony.
Finally, we conducted subgroup analysis across gender (males versus females; model 9), age groups (middle-aged, 45–59 years; ‘young olds’, 60–74 years; and older adults ≥75 years; model 10) and region (rural versus urban; model 11) via multiple-group RI-CLPM. Reference Mulder and Hamaker31 This was done to examine potential gender, age and regional differences in the effects of time-invariant covariates. We conducted multiple-group RI-CLPM based on a combination of region × gender and region × age group to elucidate the contextual effect of urbanicity on the bidirectional cross-lagged effects between cognition and depressive symptoms. Sensitivity analysis was conducted on the main RI-CLPM model in the data-set with complete data cases to check for robustness of the results.
Results
Descriptive statistics
Around two-thirds (64–67%) of the sample were currently working and half participated in social activities; 19.8–26.9% of the sample reported drinking at least once per month, and they reported average levels of self-rated health (mean 2.98–3.11, s.d. = 0.91–1.03). Supplementary Table 1 shows the descriptive statistics of cognition and depressive symptoms across the five waves. The proportion of depression cases ranged from 31.4 to 37.5% across the five waves. Strong and moderate bivariate autocorrelations were found among cognition (r = 0.60–0.75, P < 0.01) and depressive symptoms (r = 0.42–0.55, P < 0.01), respectively. Significant and negative correlations (r = −0.19 to −0.29, P < 0.01) were found between cognition and depressive symptoms. The results of attrition analysis are presented in the Supplementary material. Compared with waves 1–4, the CHARLS sample at wave 5 showed significantly higher levels of cognition and depressive symptoms (B = 0.30–0.74, s.e. = 0.06, P < 0.01) but lower levels of self-rated health, drinking frequency and likelihood of working (B = −0.032 to −0.042, s.e. = 0.01, P < 0.01). The wave 5 sample did not show significant difference in regard to participation in social activities from previous waves (B = −0.01, s.e. = 0.01, P = 0.26).
RI-CLPM
As shown in Table 1, CLPM with first-order autoregression effects (model 1) provided a poor fit to the data, while the addition of second-order autoregression effects led to improved model fit. In comparison, RI-CLPM provided a good model fit (CFI and TLI > 0.95, RMSEA and SRMR < 0.04), which was superior to model 2 with a lower BIC. In model 3, the two random intercepts were negatively and moderately correlated (r = −0.40, P < 0.01) on the between part. For the within part, there were significant and negative contemporaneous associations (r = −0.056 to −0.120, s.e. = 0.010–0.019, P < 0.01) between cognition and depressive symptoms for each time point. Next, we added the time-invariant and -varying covariates into RI-CLPM, and model 4 showed an acceptable model fit. Scaled χ 2 difference tests rejected the assumptions of equal autoregressive effects (Δχ 2 = 601.3, Δd.f. = 6, P < 0.01) and equal time-varying covariates effects (Δχ 2 = 284.2, Δd.f. = 32, P < 0.01), but not equal cross-lagged effects (Δχ 2 = 12.5, Δd.f. = 6, P = 0.052). Model 7 showed the lowest BIC as the most parsimonious representation of RI-CLPM with covariates; model 8 showed a BIC similar to that of model 7, with equivalent model fit indices. This suggested comparable cross-lagged effects from cognition to depressive symptoms and from depressive symptoms to cognition.
Table 1 Fit indices of CLPM and RI-CLPM for cognition and depressive symptoms in the entire sample and across demographic subgroups
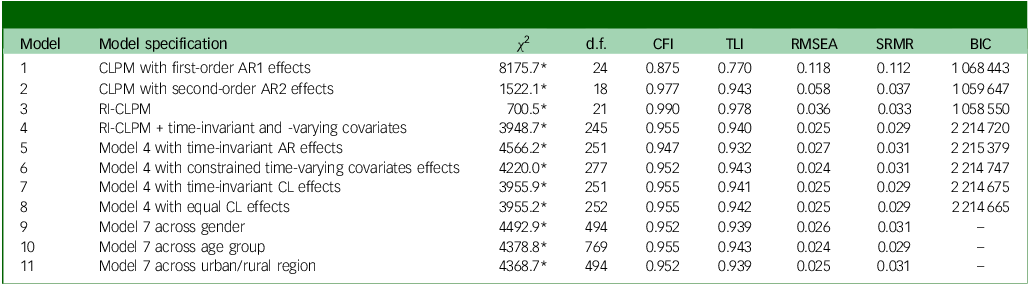
CLPM, cross-lagged panel model; RI-CLPM, random-intercepts CLPM; AR, autoregressive; CL, cross-lagged; χ 2, chi-square; CFI, comparative fit index; TLI, Tucker–Lewis index; RMSEA, root mean square error of approximation; SRMR, standardised root mean square residual; BIC, Bayesian information criterion.
*P < 0.01.
Effects of covariates
Table 2 shows the effects of time-invariant covariates on random intercepts in the between-person part of model 7. Age was significantly and negatively associated with cognition but not with depressive symptoms. Lower levels of cognition and higher levels of depressive symptoms were found among female gender, lower education level, not married, living in rural region, lifetime smoking history, lower household expenditure and poorer relationships with parents.
Table 2 Effects of time-invariant covariates on cognition and depressive symptoms at between-person level in the entire sample and across gender
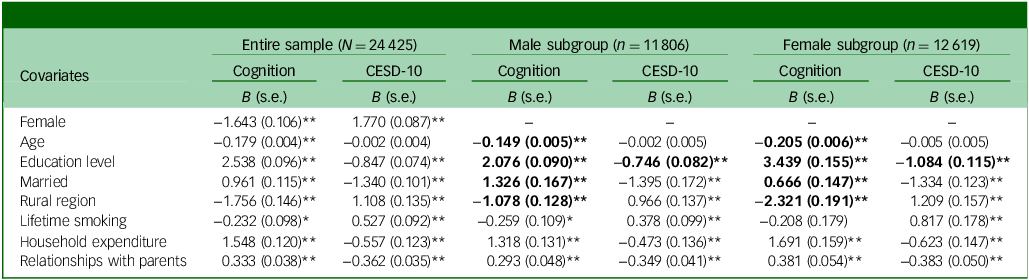
CESD-10, 10-item Center for Epidemiologic Studies Depression Scale; B, unstandardised coefficient.
Bold typeface denotes significant differences (P < 0.01) between male and female subgroups.
*P < 0.05, **P < 0.01.
Table 3 shows the effects of time-varying covariates on cognition and depressive symptoms in the within-person part of model 7. Better self-rated health was associated with higher cognition (B = 0.11–0.36, P < 0.01) and fewer depressive symptoms (B = −1.51 to −2.19, P < 0.01) across the five waves. Similarly, participation in social activities was associated with higher cognition (B = 0.59–1.08, P < 0.01) and fewer depressive symptoms (B = −0.22 to −0.63, P < 0.01) across the five waves. Work status was associated with higher cognition (B = 0.45–0.62, P < 0.01) and fewer depressive symptoms (B = −0.27 to −0.39, P < 0.01) in some waves. Alcohol drinking showed minimal associations with cognition (B = 0.001–0.032, P > 0.01) and fewer depressive symptoms (B = −0.07 to −0.09, P < 0.01) in waves 4 and 5.
Table 3 Effects of time-varying predictors on within-person cognition and depressive symptoms across five measurement waves
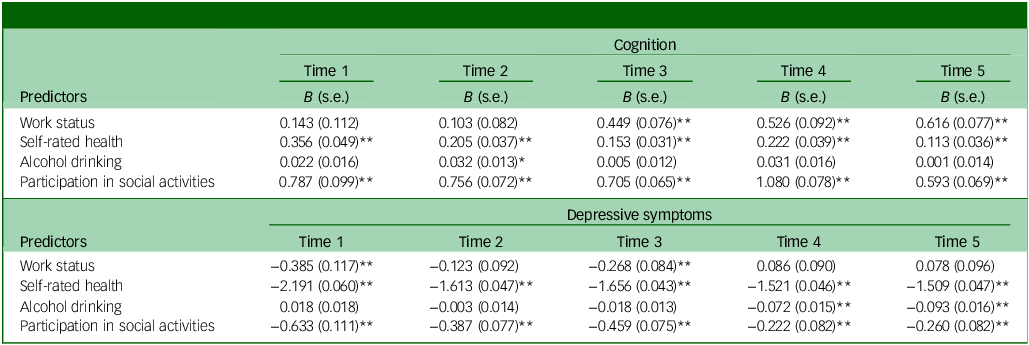
B, unstandardised coefficient.
*P < 0.05, **P < 0.01.
Autoregression and cross-lagged effects of cognition and depressive symptoms
Figure 2 shows the autoregression and cross-lagged effects in the within part of model 7. Significant and positive autoregression effects (autoregression 0.08–0.21, P < 0.01) were found for depressive symptoms. The autoregressive effects for cognition were non-invariant across time, changing from being significantly negative (autoregressive –0.07, P < 0.01) to significantly positive (autoregressive 0.29, P < 0.01) in later waves. Controlling for time-varying covariates, cognition showed a significant and negative cross-lagged effect (B = −0.027, s.e. = 0.008, P < 0.01) on depressive symptoms. Depressive symptoms showed a significant and negative cross-lagged effect (B = −0.024, s.e. = 0.005, P < 0.01) on cognition. For CLPM with second-order autoregression effects (model 2), the corresponding cross-lagged effects were cross-laggedcog → CESD-10 = −0.071, s.e. = 0.004, P < 0.01 and cross-laggedCESD-10 → cog = −0.038, s.e. = 0.004, P <0.01, respectively. In model 7, the explained R 2 for the random intercepts of cognition and depressive symptoms was 41.7 and 15.8%, respectively. For the within part, the explained R 2 ranged from 2.1 to 14.0% for cognition and from 14.6 to 17.7% for depressive symptoms.
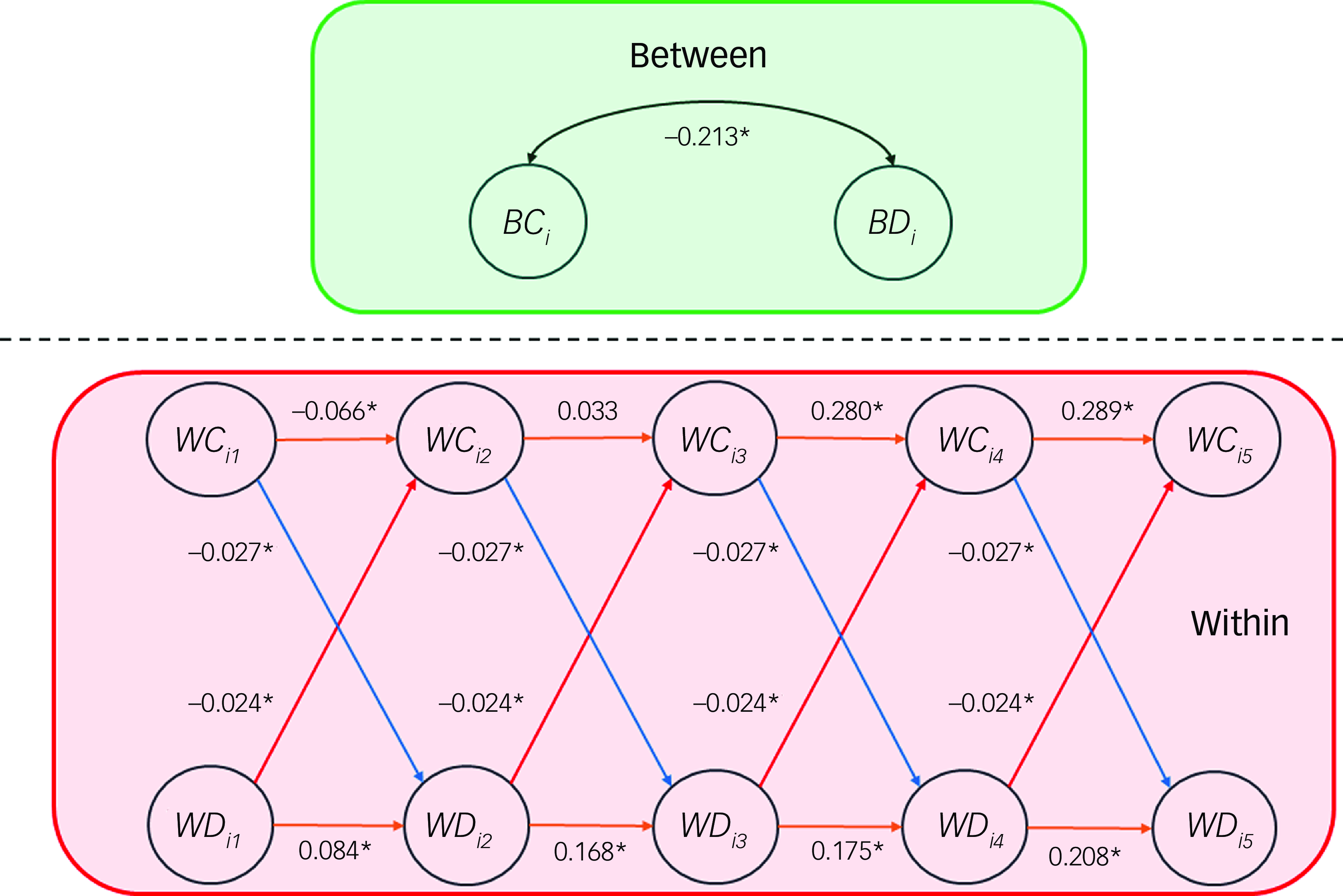
Fig. 2 Autoregressive and cross-lagged effects in the within part of the random-intercept, cross-lagged panel model. BC i and BD i , random intercepts for cognition and depressive symptoms, respectively, at the between level; WC it and WD it , within-person components of cognition and depressive symptoms, respectively, of individual i at wave t. Autoregressive effects are shown in orange, and cross-lagged effects in red and blue; the correlation between random intercepts is shown in black. For simplicity of presentation, the time-invariant and -varying covariates and contemporaneous associations between cognition and depressive symptoms are not shown. *p < 0.05.
As shown in Table 4, male and female subgroups showed similar cross-lagged effects between cognition and depressive symptoms. The cross-lagged effects were, however, significant in rural regions but not in urban regions. The cross-lagged effect of cognition on depressive symptoms was not significant in older adults aged 75 years or above. In subgroup analysis across region × gender, negative bidirectional cross-lagged effects were found between cognition and depressive symptoms in rural males. Across region × age group, there was a significant and negative cross-lagged effect from cognition to depressive symptoms in rural middle-aged adults and a significant and negative cross-lagged effect from depressive symptoms to cognition in rural young olds and older adults.
Table 4 Cross-lagged effects between cognition and depressive symptoms across demographic subgroups
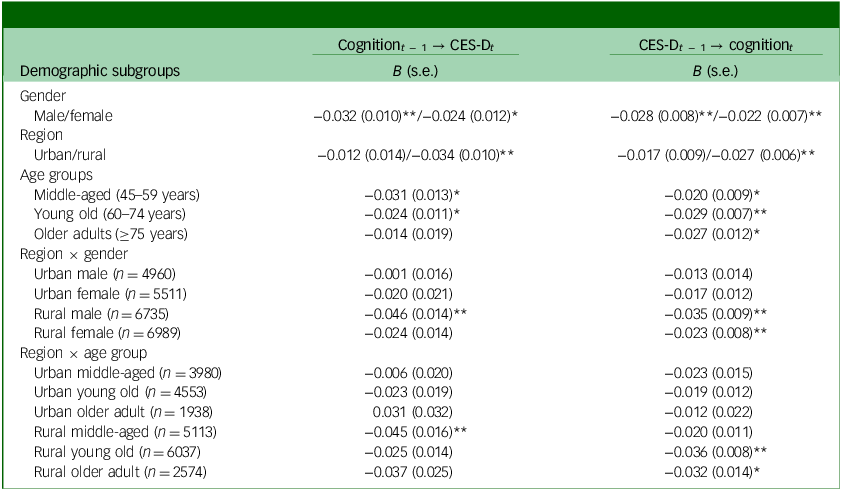
t, wave; B, unstandardised coefficient; CES-D, 10-item Center for Epidemiologic Studies Depression Scale.
*P < 0.05, **P < 0.01.
RI-CLPM with covariates across demographic subgroups
Satisfactory model fit was obtained for RI-CLPM with covariates across gender, age group and rural region (models 8–10). The effects of time-invariant covariates on cognition and depressive symptoms across gender, region and age group are shown in Table 2 and Supplementary Tables 2 and 3, respectively. Across gender, the effects of age, education level and rural region on cognition were significantly (P < 0.01) stronger in females than in males. Across regions, the effects of education level on cognition and depressive symptoms were significantly stronger (P < 0.01) in rural regions than urban regions. The negative effect of age on cognition was strongest in older adults, followed by middle-aged adults and young olds. The effect of age on depressive symptoms was significant and positive in middle-aged adults but significant and negative in older adults. Supplementary Tables 4–7 display the effects of time-varying covariates on cognition and depressive symptoms across gender and regions. Most of the effects were consistent across gender and regions, except for greater protective effects of work status on cognition and depressive symptoms in males than females, and greater protective effects of work status on cognition in rural regions compared with urban.
Discussion
Main findings
Using RI-CLPM, the present study evaluated the bidirectional relationships between cognition and depressive symptoms and the effects of sociodemographic and lifestyle factors in a large and representative sample of Chinese middle-aged and older adults over a 10-year period. RI-CLPM modelled long-term, trait-like stability as random intercepts and provided a well-fitting and systematic representation of the dynamical relationships of between- and within-person levels. Reference Mulder and Hamaker31 After controlling for between-person variation and the effects of time-varying covariates, the present study found significant and negative bidirectional relationships between cognition and depressive symptoms at the within-person level. In addition, the present study elucidated the factors associated with cognition and depressive symptoms at between- and within-person levels. Our results highlight health disparities in cognitive and emotional health across gender, age group and urbanicity.
This study found a better model fit for RI-CLPM than for traditional CLPM. This is in line with the findings of the existing literature, in which second-order lagged relations were required to obtain an acceptable fit in CLPM. Our results corroborate dynamic relationships between cognition and depressive symptoms over a 10-year period, where cognitive decline predicts increased depressive symptoms in the next wave. This could, in turn, lead to further declines in cognitive abilities and result in vicious cycles in subsequent waves. The present cross-lagged effects estimated using RI-CLPM showed values similar to those estimated in recent studies, Reference Csajbók, Aarsland and Cermakova14 and were considerably lower (34.2–60.6%) than the corresponding estimates with CLPM. Because CLPM does not separate between-person from within-person variances, previous CLPM studies could have overestimated the cross-lagged effects between cognition and depressive symptoms. Cognition showed greater between-person variance in the random intercept than the within-person components. The greater proportion of between-person variances plausibly explains the greater discrepancy for the estimates of cross-lagged effect from cognition to depressive symptoms between CLPM and RI-CLPM.
Our study found consistent and positive associations between smoking and depressive symptoms across gender, regions and age groups. In the present sample, age was significantly linked with greater and fewer depressive symptoms in middle-aged and older adults, respectively. The quadratic relationship between age and depressive symptoms indicated different sources of mental health stressors (such as work or retirement stress) for different age groups. We found a negative effect of smoking on cognition in males and older adults, which is in line with the existing literature on the detrimental effects of smoking. Reference Gallagher, Kiss, Lanctot and Herrmann7 Alcohol drinking did not show any adverse effects on cognition and depressive symptoms at the within-person level in this study. We found consistent associations between participation in social activities and better cognition and fewer depressive symptoms across the five waves. This agrees with recent findings on the protective role of social engagement in cognition and depression. Reference Paiva, Cunha, Voss and Delerue Matos20 Future research should elucidate the role for different types and frequency of social participation in improving cognitive functions and emotional well-being.
Subgroup analysis across sociodemographic characteristics revealed interesting findings in the present study. The gender difference in cognition favouring males over females is consistent with existing findings. Reference Lei, Hu, McArdle, Smith and Zhao33 Subgroup analysis across gender found significantly stronger effects of age, education level and rural region on cognition in females than in males. Among Chinese older adults, females had lower education levels and social status than males, particularly in rural regions. Reference Zhang, Pang, Zhang, Medina and Rozelle34 Subgroup analysis across age groups showed that gender differences in cognition gradually diminished across birth cohorts. One recent RI-CLPM study found significant cross-lagged effects from cognition to depressive symptoms only in older adults. Reference Csajbók, Aarsland and Cermakova14 In contrast, the present study found a decreasing trend in cross-laggedcog → CESD-10 effect across age groups, which was not significant among older adults.
Limitations
In terms of limitations, the present study did not include other potential mediators such as diet and nutrition, physical activity and sleep quality. Further studies could elucidate environmental factors such as air quality, urbanisation and residential greenness that could contribute to cognition. Second, CHARLS included only single-item measures of lifestyle and social factors, which could potentially have biased regression coefficients of the covariates. Future studies could consider the use of multiple-item scales or latent factors to account for measurement errors. Third, the present study focused on the overall cognitive function but did not differentiate separate domains of cognition, such as memory, executive function, language and attention. Further research could aim for a deeper investigation of the relationships between specific cognitive domains and depressive symptoms, and other modifiable factors at the symptom level, using network analysis.
Fourth, the present analysis relied on the missing-at-random assumption for missing data. Cognition decline and subsequent mortality would be associated with greater item missingness and non-response rate at follow-up, which implies that missing data were missing not at random. The present results are subject to potential attrition bias and mortality bias. Fifth, the latest CHARLS wave 5 data were collected during the pandemic in summer 2020. The social distancing measures associated with the pandemic could have prolonged impacts on the psychosocial well-being of the respondents, and their effects on cognition might not have manifested within 6 months. Follow-up assessments are needed to gauge the long-term effects of social isolation on cognition in older adults in a post-pandemic context. Sixth, the present study was mostly based on self-reported measures and was subject to common method bias. Previous studies have found significant associations between depressive symptoms and type 2 diabetes, Reference Zhao, Pan, Yang, Meng, Ye and Wang39 and associations between cognitive function and biological ageing. Reference Wu, Huang, Zhang, Zhang and Lan40 Further studies should investigate the relationships between psychocognitive measures and biomarkers.
Study implications
The present results have clinical implications for the development of interventions. In the present study, participants living in rural regions showed worse cognition and greater depressive symptoms than those living in urban regions, and such differences persisted after controlling for individual characteristics, including education level and contextual-level household socioeconomic status. These are in agreement with findings on neighbourhood context and cognition among American older adults. Reference Wight, Aneshensel, Miller-Martinez, Botticello, Cummings and Karlamangla35 The negative effect of age on cognition was stronger in middle-aged adults than in young olds. Cognition showed a significant and negative cross-lagged effect on depressive symptoms in middle-aged adults in the rural, but not urban, context; this indicates stronger comorbidity between cognitive decline and emotional distress in the rural context. One CHARLS study found greater impacts of neighbourhood environment on cognition in rural regions than in urban. Reference Luo, Zhang and Pan36 Further research should aim to elucidate the contextual difference in linkages between cognition and depressive symptoms.
In the rural context, establishment of primary mental health care screening could enable early identification of early cognitive decline to prevent subsequent mental distress in middle-aged adults. The provision of psychosocial interventions in relieving psychological distress could possibly delay the associated cognitive decline in young olds and older adults. Depression should be an intervention element as well as an outcome of cognitive stimulation activities. Sharkey and Elwert Reference Sharkey and Elwert37 have linked exposure to neighbourhood poverty across two consecutive generations to reduction in children’s cognitive function, and the effects of neighbourhood environment on cognition extended across generations. One 10-year longitudinal study found that education level mitigated the influence of depressive symptoms on cognition in older adults. Reference Cano-López, Aliño, Duque, Martínez, Almela and García-Rubio38 More resources should be allocated to rural regions to promote overall educational attainment to reduce health disparities. Public health initiatives should strive for maintenance of emotional health and cognitive function as key factors that contribute to healthy ageing. Long-term cognitive function assessments in large-scale depression-reduction programmes can verify their impact on mitigating cognitive decline.
Using a large representative sample of Chinese middle-aged and older adults, the present study contributes to a better understanding of bidirectional relationships between cognition and depressive symptoms and associated factors. The present RI-CLPM provided nuanced results on negative bidirectional relationships between cognition and depressive symptoms in Chinese middle-aged and older adults. Our results have clinical implications in highlighting the health disparities in cognitive and emotional health across urbanicity and age groups.
Supplementary material
The supplementary material is available online at https://doi.org/10.1192/bjo.2025.10074
Data availability
The China Health and Retirement Longitudinal Study (CHARLS) data-sets are available from https://charls.charlsdata.com/pages/Data/harmonized_charls/en.html and https://charls.charlsdata.com/pages/data/111/en.html upon registration. The Mplus syntax in this study is available from the corresponding author, T.C.T.F., on email request.
Acknowledgements
This analysis uses data or information from the Harmonized CHARLS data-set and Codebook, Version D as of June 2021, developed by the Gateway to Global Aging Data (https://g2aging.org/). CHARLS is supported by Peking University, National Natural Science Foundation of China, National Institute on Aging and the World Bank. The development of Harmonized CHARLS was funded by the National Institute on Aging (nos R01 AG030153, RC2 AG036619 and R03 AG043052). The present study was not preregistered.
Author contributions
T.C.T.F.: conceptualisation, data curation, formal analysis, investigation, methodology, software, visualisation, writing (original draft). R.T.H.C.: conceptualisation, investigation, methodology, writing (review and editing). M.W.: conceptualisation, resources, validation, writing (review and editing). P.S.F.Y.: conceptualisation, resources, validation, writing (review and editing). All authors approved the final submitted version.
Funding
This study received support from the Strategic Topics Grant (STG4/M-701/23-N) of the Hong Kong Research Grants Council. The sponsors had no role in the study design, the collection, analysis and interpretation of data, the writing of the report or the decision to submit the article for publication.
Declaration of interest
T.C.T.F. is a member of the BJPsychOpen editorial board. He did not take part in the review or decision-making process of this paper. All other authors declare no potential conflicts of interest.










eLetters
No eLetters have been published for this article.