People with intellectual disabilities die on average 20 years earlier than the general population.1 Although respiratory and cardiovascular conditions are the leading causes of death, many other conditions, such as constipation, contribute to this premature mortality.Reference Heslop, Blair, Fleming, Hoghton, Marriott and Russ2
Constipation in people with intellectual disabilities
Constipation is a heterogeneous condition with multiple aetiology.Reference Talley3 Most prevalence rates of constipation in people with intellectual disabilities vary between 25 and 50%.Reference Maslen, Hodge, Tie, Laugharne, Lamb and Shankar4 Of 31 studies in a recent systematic review, constipation rates of over 33% were reported in 21 studies.Reference Robertson, Baines, Emerson and Hatton5 There is a general acceptance that rates are higher than in the general population, with a quarter of people with intellectual disabilities prescribed repeated laxatives in a 12-month period, compared with 0.1% of the general population.Reference Straetmans, van Schrojenstein Lantman-de Valk, Schellevis and Dinant6
Despite constipation being a common issue, it continues to be a significant problem in people with intellectual disabilities, often causing suffering and even leading to death.Reference Roy and Simon7,Reference AlMutairi, O'Dwyer, Burke, McCarron, McCallion and Henman8 Hospital admission rates and mortality rates are difficult to estimate because of the varying methodologies by which they are recorded.Reference Maslen, Hodge, Tie, Laugharne, Lamb and Shankar4 Therefore, the evidence base is primarily from case reports, which have been described in the UK, Germany and Serbia,Reference Maslen, Hodge, Tie, Laugharne, Lamb and Shankar4 and a case series of 12 people with intellectual disabilities who died of constipation between 2015 and 2018.1
Factors associated with constipation in intellectual disability
People with intellectual disabilities have several risk factors for developing problems with constipation.Reference Robertson, Baines, Emerson and Hatton5 Factors associated with constipation in people with intellectual disabilities from previous studies include profound intellectual disability, cerebral palsy, lack of mobility, Down syndrome, certain medications (including anti-epileptic medication, benzodiazepines, histamine H2-receptor antagonists and proton pump inhibitors) and non-ambulatory status.Reference Bohmer, Taminiau, Klinkenberg-Knol and Meuwissen9
Current challenges in assessment of constipation-related risk factors
The commonly used diagnostic checklists, including the Rome IV checklist and Bristol Stool Chart, are focused on identifying constipation and not the risk factors for constipation specific to people with intellectual disabilities. These checklists can be difficult to use because people with intellectual disabilities may not have the cognitive ability to use them directly. It can be challenging for carers to bring detailed insight and information to such a personal matter of toileting, especially for individuals who are faecally incontinent and those who are non-verbal, thus resulting in poor data acquisition. There is a need for prospective studies to further clarify risk and mitigating factors. Evidence-based frameworks are needed for staff to consult in order to produce individualised programmes of bowel management.Reference Robertson, Baines, Emerson and Hatton10
We aimed to survey the carers of people with an intellectual disability to identify the presence or absence of constipation in those they cared for and identify the presence of possible risk factors for constipation.
Method
We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidance for cross-sectional studies (www.strobe-statement.org/).
Survey tool
Constipation was defined as opening bowels two or fewer times per week or using laxatives three or more times weekly. This is a definition used in another study on people with intellectual disabilities, including severely disabled people who are non-verbal and/or incontinent of faeces.Reference Bohmer, Taminiau, Klinkenberg-Knol and Meuwissen9
The questionnaire was devised from the literature and a consensus of a group of experts including psychiatrists working with people with intellectual disabilities, pharmacists, a dietician, a specialist bowel nurse and a general practitioner (Supplementary Appendix, available at https://dx.doi.org/10.1192/bjo.2024.12). The focus of the questionnaire was to detect the symptoms of constipation and the presence or absence of possible risk factors for constipation. The questionnaire was devised such that it could be completed on paper, over the telephone or digitally. The target audience for the questionnaire were families and non-clinical professional carers. The draft survey was shared with the Inclusive Communication team in Cornwall County Council, a team dedicated to promoting and supporting delivery of effective communication. They provided guidance on inclusive communication measures and further adaptations to the survey. It was made explicit that this questionnaire is for carers of people with intellectual disabilities and not for people with intellectual disabilities themselves.
Population and sample
The questionnaire was sent to the carers of all patients on the case-loads of four community intellectual disability teams across southern England, in Cornwall (population 538 000), Devon (750 000), Haringey (300 000) and Essex (population 500 000). The survey was disseminated via email and/or post, along with a cover letter and, if postal, a stamped return envelope.
Ethics and governance
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. The National Health Service (NHS) Health Research Authority tool (www.hra-decisiontools.org.uk/research/index.html) confirmed that no formal NHS ethics approval was required (Supplementary information 2). The project was registered as a quality improvement project at uk.lifeqisystem.com. Each participating site registered the project at their respective NHS trust as a service evaluation/improvement project. Only the authors who worked for the respective intellectual disabilities services had access to any patient-identifiable information. Participants were informed in the cover letter that return of their survey via the pre-paid return envelope constituted informed consent to use the information provided. Collected clinical data at each NHS site were stored on an Excel spreadsheet, anonymised and then shared for analysis. The project used anonymised pooled data from the four centres, with each site having conducted a Data Protection Impact Assessment (DPIA) with support from their governance departments.
Analysis
The analysis of the data focused on summarising the carers’ responses for the total sample of people with intellectual disabilities (‘participants’), and also comparing results between participants with and without constipation. The anticholinergic burden score was calculated from medication listed as taken by the participant,Reference Boustani, Campbell, Munger, Maidment and Fox11 summarised and compared. Questionnaire responses were categorical in nature. These factors were compared between those with constipation and those without constipation using the chi-squared test. Fisher's exact test was used to determine whether there are non-random associations between two categorical variables. Continuous measurements were found to have a skewed distribution and the Mann–Whitney test was used to compare between the two groups. Significance was taken at P < 0.05.
Results
The questionnaire was sent to the carers of individuals on the case-loads of four intellectual disability teams (approximately 800 people) and we received responses for 181 of these individuals. Responses on the two questions relating to presence or absence of constipation and/or laxative use are summarised in Table 1. The figures are the number of responses in total, and then the number in each category.
Table 1 Summary of constipation variables from questionnaires regarding 181 participants with intellectual disabilities
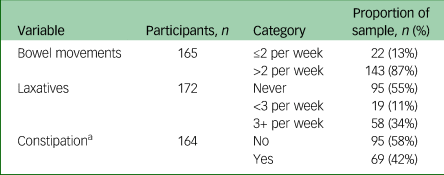
a. Defined as ≤2 bowel movements per week or laxatives ≥3 times per week.
The results suggested that 13% of participants had two or fewer bowel movements per week. One-third (34%) had three or more laxative uses per week.
Overall, constipation was assessed in 164 of the 181 participant forms received. Constipation could not be assessed for 17 participants owing to missing values for one or both components of the definition. Of those where constipation could be assessed, the data suggested that 42% of all participants had constipation defined as two or fewer bowel movements per week or regular laxatives three or more times weekly.
Table 2 summarises the demographics of the participants, along with other comorbid health conditions. The figures reported are the number of responses in each group, along with the number and percentage of responses in each category. Comparisons between those with and without constipation was made.
Table 2 Demographics and health conditions
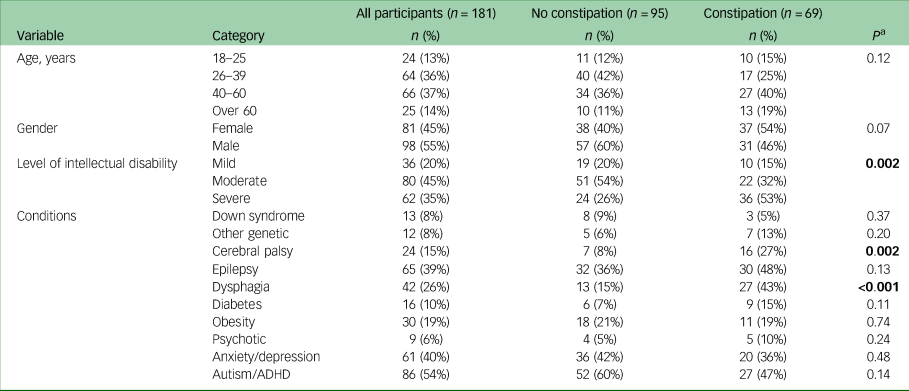
ADHD, attention-deficit hyperactivity disorder.
a. Significant correlations based on P < 0.05 are indicated in bold.
There was no evidence of a difference in the age and gender of those with and without constipation. The constipation group had a higher proportion of females than the group without constipation, but the difference did not reach statistical significance.
There was a significant difference in the level of intellectual disabilities between those with constipation and those without constipation (P = 0.002). In the constipation group, over half (53%) had moderate to profound intellectual disabilities, compared with only a quarter (26%) in the group without constipation.
The majority of other health conditions did not vary significantly between groups. However, differences were observed for cerebral palsy (P = 0.002) and dysphagia (P < 0.001). Both of these conditions were more common in those with constipation compared with those without constipation. Cerebral palsy was observed in 27% of those with constipation, compared with 8% without. Dysphagia was present in 43% of patients with constipation, but in only 15% of those without constipation.
Information on the toilet habits and constipation-influencing behaviours is summarised in Table 3. The fluid intake of the two groups did not significantly differ. However, differences between groups were observed for toileting (P < 0.001), toilet routine (P < 0.001) and mobility (P < 0.001). Those with constipation were more likely to require toileting support, more likely to have an assisted toilet routine and had worse mobility compared with those without constipation. There was also evidence that those with constipation were more likely to use a footstool or other toileting aids, although this difference did not quite reach statistical significance (P = 0.07).
Table 3 Constipation-influencing behaviours

a. Significant correlations based on P < 0.05 are indicated in bold.
Three-quarters (76%) of those with constipation required support with toileting, compared with only 29% of those without constipation. Less than half (41%) of those with constipation were reported to have good mobility, contrasting with more than three-quarters (81%) of those without constipation. These findings may be explained by greater physical disability among those with constipation.
Information on medications is summarised in Table 4. Overall, 41% of participants were on anti-epileptic medication, and one-third (33%) were on antipsychotics. These medications, along with benzodiazepines, H2 antagonists and proton pump inhibitors, did not vary significantly between those with and without constipation. However, the total number of medications was significantly higher in the constipation group. The group with constipation had a median of five medications, compared with a median of three for the group without constipation. The anticholinergic burden (ACB) scores of the two groups were not significantly different, although a higher score was found in those with constipation (ACB = 2) than those without (ACB = 1).
Table 4 Medications

ACB, anticholinergic burden.
a. Significant correlations based on P < 0.05 are indicated in bold.
b. Summary statistics are: median (interquartile range).
Laxatives were significantly more common in those with constipation. This result is not surprising as laxative use was part of the definition of constipation. Over 65% of the constipation group used laxatives, compared with 5% of those without constipation. Osmotic laxatives were the most used in both groups. Both osmotic and stimulant laxatives had higher levels of use in the group with constipation than in those without constipation (P < 0.001).
Discussion
Previous studies have suggested that the prevalence of constipation in people with intellectual disabilities is between 33 and 50%Reference Robertson, Baines, Emerson and Hatton5 and the prevalence in this sample was 42%. The main findings of this community survey of people with intellectual disabilities is that those who were constipated were more likely to have greater severity of both physical disability as well as intellectual disability. They were more likely to have cerebral palsy, experience dysphagia, have poor mobility and require an assisted toileting regime. They were also more likely to be on a greater number of medications. The association with severity of the intellectual disability and poor physical mobility is consistent with previous researchReference Robertson, Baines, Emerson and Hatton5,Reference Bohmer, Taminiau, Klinkenberg-Knol and Meuwissen9 but adds to it in emphasising the importance of dysphagia, severity of physical disabilities and polypharmacy as risk factors. The consistency in findings is, however, concerning as one of the main previous studies (in The Netherlands) was conducted over 20 years agoReference Bohmer, Taminiau, Klinkenberg-Knol and Meuwissen9 and the situation has changed little. Our study group devised a constipation questionnaire which has been shown to be feasible in routine clinical services and completed by carers with varying degrees of knowledge.
A concern is the high prevalence of anti-seizure medication and antipsychotics identified in our sample. Recent studies focused on characteristics of people with intellectual disabilities and epilepsy have highlighted the high frequency of antipsychotic prescribing along with associated polypharmacy.Reference Sun, Perera, Henley, Angus-Leppan, Sawhney and Watkins12 Furthermore, in a recent case–control study comparing a group of people with epilepsy and intellectual disability who had died with live controls from the same population, the authors identified significant differences in antipsychotic prescribing and overall polypharmacy as major modifiable factors.Reference Sun, Watkins, Henley, Laugharne, Angus-Leppan and Sawhney13 The links of these factors (antipsychotics, anti-epileptics and polypharmacy) to premature mortality in people with intellectual disabilities and their links in our study to constipation needs to be highlighted.
Limitations
Our questionnaire was devised by experts in a wide range of fields and made use of the published literature. However, although the questionnaire has face validity it has not been tested for other psychometric properties. We cannot claim our sample to be representative of the intellectual disability population as the responses depended on the willingness of carers to complete the questionnaire. Further, the questionnaires are only in English and we failed to capture respondent and participant ethnicity, which could influence the feedback. Our study sample comprised individuals under the care of secondary specialist community services for people with intellectual disabilities and therefore will not reflect people with intellectual disabilities not under the care of secondary services and solely cared for in primary care. It could be considered a convenience sample. The study population was selected through clinical networks and is not necessarily representative of the whole population. However, it includes urban and rural communities in the south of England.
We included all questionnaires that were sent back and could not monitor response rates or the characteristics of those who did and did not respond. Therefore, we cannot claim that those responding are representative of all patients on the case-loads of the secondary specialist teams.
Implications for clinical practice
Our study suggests that people with more severe intellectual disabilities, more severe physical disabilities (including dysphagia and cerebral palsy) and on multiple medications are more likely to suffer from constipation. This subset of people with intellectual disabilities need vigilance over their bowel health. Regular and possibly enhanced screening, together with an individualised bowel health plan, may benefit them. This should be coupled with regular medication reviews, especially if there is polypharmacy and particularly if the polypharmacy is suspected to affect bowel health. The Annual Health Checks could be an important vehicle to provide a basic and essential level of oversight on these matters for this vulnerable cohort.
It is recognised that carers and family members value good person-centred communication from professionals on constipation management.Reference Rooney, Hodge, Smith, Vanstone, Laugharne and Shankar14 The risk factors identified could provide improved feedback from clinicians to carers.
The finding that 181 carers were able to complete the questionnaire and the findings were coherent suggests that it is feasible to use this questionnaire in clinical practice to detect constipation and identify risk factors that can be modified, although further research needs to be conducted to establish whether it can lead to changes in outcomes. Individualised bowel care plans may be based on the feedback from the questionnaire, and this has been delivered for some patients.
Implications for research
Although there has been significant work done in this area and reviews of the literature, the focus has been more on understanding the broader problem than specific influencers. We suggest the following:
(a) there is a need for large-scale studies using multivariate analysis to further clarify the modifiable and non-modifiable risk factors associated with constipation in people with intellectual disabilities;
(b) constipation questionnaires and individualised bowel care plans need to be evaluated to examine whether they improve bowel health and quality of life, which should be the goal of our endeavours;
(c) targeted screening and interventions for people with intellectual disabilities most vulnerable to constipation, particularly those with severe intellectual and physical disabilities, should be tested and interventions examined;
(d) implementation science needs to be utilised to enable research findings to be implemented in routine clinical care and not just in research arenas.
Implications for policy
Clear guidelines are needed on monitoring, detecting and treating constipation in people with intellectual disabilities, emphasising the greater vulnerability of those with severe physical disabilities.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2024.12.
Data availability
The data that support the findings of this study are available from the corresponding author on reasonable request.
Author contributions
All authors satisfy the ICMJE guidance by substantially contributing to the design, analysis and interpretation of the work, drafting of the manuscript, final approval of the manuscript and all agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work is appropriately investigated and resolved.
Funding
This research received no specific grant from funding agency, commercial or not-for-profit sectors.
Declaration of interest
R.L. is the UK chief investigator for studies with Janssen and Boehringer-Ingelheim outside the submitted work. R.S. has received institutional and research support from LivaNova, UCB, Eisai, Veriton Pharma, Bial, Angelini, UnEEG and Jazz/GW pharma outside the submitted work; he holds grants from the National Institute for Health and Care Research (NIHR) AI Health and Care Award, the Small Business Research Initiative (SBRI) Healthcare and other funding bodies all outside this work. R.S. is a member of the BJPsych Open editorial board and did not take part in the review or decision-making process of this paper.







eLetters
No eLetters have been published for this article.