Background
Older adults in need of psychiatric treatment differ from younger ones with higher rates of suicide,Reference Värnik1 somatic comorbidity, physical frailty, cognitive and functional decline, symptom presentation and pharmacokinetic characteristics.Reference Skoog2–Reference Draper5 Most current guidelines recommend specialised psychogeriatric treatment when mental illness starts after the age of 65.6–9 Consequently, older adults are often treated within general adult psychiatry if they have a previously established mental disorder with few age-related complications,8 if they are formerly known to service providers7 or if preferred by the patient.10 Although psychogeriatric units have been shown to be superior to general adult psychiatry at providing a comprehensive medical and psychiatric work-upReference Yazgan, Greenwald, Kremen, Strach and Kramer-Ginsberg11 and at meeting the needs of elderly patients,Reference Abdul-Hamid, Lewis-Cole, Holloway and Silverman12 there is no clear international consensus concerning the subdivision in general adult or psychogeriatric services – which is based on expert opinion rather than clinical evidence.
The proposal in a guideline in the UK by the Royal College of Psychiatrists, omitting the original age-based World Health Organization definition and instead further emphasising the patient's need and choice,10 was also primarily motivated by political decisions rather than the emergence of new evidence.Reference Warner13 Against this backdrop, several guidelines emphasise the need for further research.7,8,14
In the very few studies specifically investigating the characteristics of older adults with mental illness presenting in later life the most robust finding is the association between first admissions and organic psychiatric disorders.Reference Freyne and Wrigley15–Reference Shulman, Marton, Fisher and Cohen17 In in-patients with depression, a link between first admissions and increased suicide risk has been reported.Reference Erlangsen, Zarit, Tu and Conwell18 However, the mentioned studies show significant heterogeneity with regard to sample sizes, setting, age cut-off and methodological quality. Information about first admission and/or previous psychiatric history (PPH) is usually only mentioned briefly. The only prior study conducting subgroup analyses based on psychiatric history reported that patients with no previous psychiatric history (NPH) were more likely than elderly patients with PPH to have concurrent medical and cognitive problems and less likely to have bipolar or psychotic disorders.Reference Shulman, Marton, Fisher and Cohen17 However, this study was set in a general hospital emergency room, employed an age cut-off of 60 and the sample size was small.
Study objectives
In Norway, despite national guidelines recommending psychogeriatric treatment for patients with mental illness presenting at ≥65 years,8 older adults in need of acute hospital admission are initially admitted to general adult psychiatric acute units (PAUs) – however, knowledge about these patients is scarce. As research suggests that psychogeriatric units are superior to general adult psychiatric units at providing a comprehensive assessment and treatment to complex geriatric patientsReference Yazgan, Greenwald, Kremen, Strach and Kramer-Ginsberg11,Reference Abdul-Hamid, Lewis-Cole, Holloway and Silverman12 it may be assumed that central guideline criteria would allocate the patients most in need to this service. Thus, patients with NPH should be more likely than elderly patients with PPH to present with more physical frailty, somatic comorbidity and impaired everyday functioning, also in the general adult acute psychiatric setting. However, evidence to support this hypothesis is scarce. In order to provide a stronger empirical basis for how to organise mental health services for elderly people, further investigation of psychiatric admissions of older adults, especially those with mental illness presenting at ≥65 years, is needed. The main objective of our study was, in a cohort of older adults admitted to a PAU, to examine differences between patients with NPH and patients with PPH.
Method
Setting and study population
All data was retrieved from the cohort study Suicidality in Psychiatric Emergency Admissions (SIPEA), which includes all admissions to the PAU at Haukeland University Hospital in Bergen, Norway, from May 2005 to July 2014.Reference Mellesdal, Kroken, Lutro, Wentzel-Larsen, Kjelby and Oedegaard19,Reference Mellesdal, Mehlum, Wentzel-Larsen, Kroken and Jørgensen20 The Norwegian state provides free universal healthcare with virtually no competition from the private sector, and the PAU received 95% of all acute psychiatric admissions from a catchment area of approximately 350 000 people aged ≥18 years. A total of 7000 patients were admitted to the PAU during the study period. The present study included a subsample consisting of all patients aged ≥65 years at the time of admission (n = 918; 13.1% of the total patient population) (Fig. 1). Based on the patient records, we separated patients into two groups: patients with either psychiatric admissions or follow-up from a psychiatrist, psychologist or a psychiatric out-patient clinic before the age of 65 were defined as having PPH (the PPH group, n = 391), whereas those whose psychiatric specialist follow-up started after the age of 65 or who had no known psychiatric history before their admission(s) at the PAU were defined as having NPH (the NPH group, n = 526). One patient was excluded from the analyses as information regarding previous psychiatric follow-up was unavailable.

Fig. 1 Patient flow chart.
Measurements
Demographic patient information and information concerning the use of coercion (involuntary medical treatment and seclusion) during the admission was extracted from the patient files by research nurses. Length of stay at the PAU and total psychiatric hospital stay was calculated as well as information about discharge/transfer to other units (general adult psychiatry, psychogeriatric or somatic) and to nursing homes.
Information on the legal formality of the admission included: (a) involuntary referral/admission to psychiatric assessment at the PAU under the Norwegian Mental Health Act and (b) the decision about involuntary commitment (or not) by a specialist in psychiatry or clinical psychology within 24 h of admission to the PAU.
Patients were assessed at the time of admission by the psychiatric resident on-call as to whether suicidality was the reason for admission or not (yes/no). Details on suicidality were coded as (a) no known suicide ideation, (b) suicide ideation, (c) non-suicidal self-harm, (d) suicide attempt, and (e) unknown.
Alcohol and drug use was recorded using the Clinician's Alcohol/Drug Use ScalesReference Mueser, Drake, Clark and McHugo21 and results dichotomised to ‘no abuse’ (scores 1–2) and ‘abuse’ (scores 3–5). Data regarding aggressive behaviour, symptoms and functioning in the 2 weeks preceding admission was collected using the data from Health of the Nation Outcome scales (HoNOS),Reference Wing, Beevor, Curtis, Park, Hadden and Burns22 which was scored at admission. HoNOS is a rating tool developed to measure the health and social functioning of people with severe mental illness and comprises 12 items (see Table 2) that are all scored from zero (no problem) to four (severe to very severe problem).
At admission, functioning in daily life was assessed by the General Assessment of Functioning (GAF) – split version: GAF is a numeric scale ranging from zero through 100 that is used to subjectively rate the social, occupational and psychological functioning of adults.Reference Pedersen and Karterud23,Reference Hall24 The split version assesses the patient's level of symptoms (GAF-S) and functioning (GAF-F), respectively.
Clinical diagnoses assigned by clinicians in the PAU according to the ICD-1025 were grouped into categories based on ICD-10 subchapters: organic, including symptomatic, mental disorders (F00–F09), schizophrenia, schizotypal and delusional disorders (F20–F29), affective disorders (F30–F39) and neurotic, stress-related and somatoform disorders (F40–F49). The remaining diagnostic categories from the F-chapter were subgrouped as ‘other psychiatric diagnoses’, and diagnoses from the somatic chapters of ICD-10 were clustered into ‘somatic diagnoses’. Up to three diagnoses were registered at discharge. The diagnoses were scored as 1 (present) when given as the main diagnosis or one of the secondary diagnoses, otherwise as 0 (not present).
Drugs acting on the nervous system, i.e. drugs from the N-chapter of the Anatomical Therapeutic Chemical (ATC) classification system were registered at admission for each patient.
Statistical analyses
IBM® SPSS® Statistics version 24 was used for the statistical analyses. Subgroup analyses were performed using Pearson χ2-test for nominal dichotomous variables and Wilcoxon-Mann–Whitney non-parametric test for continuous variables. Statistical significance level was set at P = 0.05. In order to adjust for the age difference between the groups, sensitivity analyses were conducted analysing statistically significant results sequentially using logistic regression for dichotomous variables and linear regression for continuous variables. These analyses were then repeated after patients with organic mental disorders were excluded, since organic disorders were disproportionately frequent in the NPH group. For patients with multiple admissions, data from the first admission after turning 65 years was used. Multiple imputation was used to impute values when information for HoNOS variables were missing.Reference Schafer and Graham26 This method draws plausible values from a conditional distribution based on the mean and covariance structure between all variables. Multiple imputation is recommended even if missingness to some degree deviates from the missing at random assumption.Reference Enders27 Integer values were used in order to keep the variable at ordinal level.
Ethics
The study was approved by the Regional Committee for Medical Research Ethics and the Norwegian Social Science Data Service. The Norwegian Directorate of Health gave permission to use patient information.
Results
Patient characteristics
A total of 917 patients, mean age 74.7 years (s.d. = 7.8) and 55.5% of women were included (Table 1). Compared with the PPH group, the NPH group were significantly older (P < 0.001) and a higher proportion were men (P < 0.001). More of the NPH group were married/in a partnership or widowed, whereas those in the PPH group were more likely to be single, divorced or living alone at the time of admission (P < 0.001 for all).
Table 1 Demographic and clinical characteristics differences for patients aged 65 years or older admitted to the psychiatric acute unit (PAU)

NPH = no previous psychiatric history; PPH = previous psychiatric history; GAF = general assessment of functioning.
a. For variables with missing data, the relevant n is indicated within the table.
Admission formalities, discharge and transfer to other units
A higher proportion of the NPH group than the PPH group were referred/admitted involuntarily to the PAU (P < 0.001). In total, length of stay in the PAU before discharge/transfer to other units was 3.6 days (s.d. = 3.7). The NPH group were most likely to be transferred to psychogeriatric units, whereas most of the PPH group were transferred to general adult psychiatric units (P < 0.001 for both) (Table 1). In addition to the 310 patients transferred directly from the PAU to a psychogeriatric unit, a further 51 patients were transferred to a psychogeriatric unit after receiving initial treatment at a general adult psychiatric unit.
Suicidality
In total, 31.6% of admissions were because of suicide risk. Although the PPH group were more likely to report suicidal ideation (P = 0.006), the NPH group were more likely to have made a suicide attempt before the admission (P = 0.004) (Table 1).
Diagnoses, symptoms and functional assessment
A higher proportion of the NPH group were diagnosed with organic mental disorders (P < 0.001) and somatic disorders (P = 0.003), whereas affective and psychotic disorders were more common in the PPH group (P < 0.001 for both) (Table 1). Mean GAF scores were lower in the NPH than the PPH group for both symptoms (GAF-S) and functioning (GAF-F) (P < 0.001 for both). Alcohol and drug abuse/addiction was present in about 10% and 2% of the patients, respectively, with no differences between the NPH and PPH groups. The NPH group scored higher than the PPH group on the HoNOS items agitated behaviour; cognitive problems; problems with activities of daily living (P < 0.001 for all) and physical illness or disability (P = 0.005). The PPH group scored higher on the item depressed mood (P = 0.032) (Table 2).
Table 2 Differences in Health of the Nation Outcome Scale (HoNOS) scores for patients aged 65 years or older admitted to the psychiatric acute unit by group
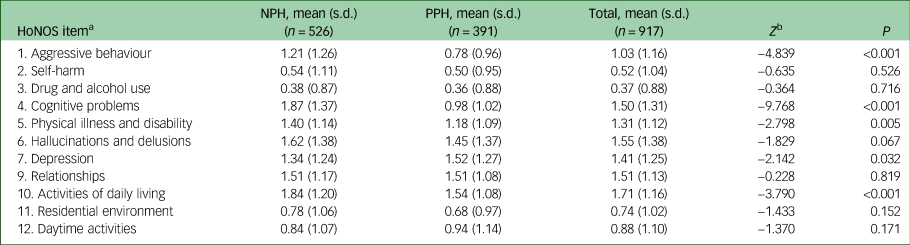
NPH, no previous psychiatric history; PPH, previous psychiatric history.
a. HoNOS item 8: Other problems was omitted due to partly being a qualitative variable.
b. Wilcoxon–Mann–Whitney Z.
Psychotropic medication
At admission, the mean number of psychotropic drugs was 1.27 (s.d. = 1.3) in the NPH group and 1.8 (s.d. = 1.45) in the PPH group (P < 0.001). A higher proportion of the NPH group had prescriptions for anti-dementia drugs (P < 0.001), whereas a higher proportion of the PPH group had prescriptions for mood stabilisers (P < 0.001), antipsychotics (P < 0.001) and benzodiazepines (P = 0.027) (Table 3).
Table 3 Differences in psychotropic drugs for patients aged 65 years or older admitted to the psychiatric acute unit by group

NPH, no previous psychiatric history; PPH, previous psychiatric history.
Adjusting for age differences and organic disorder diagnosis
After adjusting for age difference the majority of subgroup differences remained statistically significant, including psychiatric diagnoses, suicide attempts, involuntary admissions, use of psychotropic medication, problems with aggression, cognitive impairment, severity of psychiatric symptoms (GAF-S) and psychiatric discharge/transfer destination (supplementary Tables 1 and 2 available at https://doi.org/10.1192/bjo.2020.45). Variables that did not remain statistically significant included suicide ideation, functional impairment and disability, severity of depression, somatic comorbidity and transfer to a general hospital.
Repeating the age-controlled analyses after excluding patients with organic mental disorder, subgroup differences that were robust for these sensitivity analyses were most of the sociodemographic and discharge characteristics, diagnosis within psychotic disorders and suicide attempts. Variables that did not remain statistically significant included involuntary admissions, discharge to nursing home, problems with aggression, cognitive impairment and severity of psychiatric symptoms (GAF-S). See supplementary Tables 3 and 4 for more details.
Discussion
Main findings
Our study is the largest to date to investigate demographic and clinical characteristics of people ≥65 years admitted to a general adult PAU and the first to compare older adults with regard to PPH or NPH in this setting. Corresponding with our hypothesis we found that patients with NPH were more likely than patients with PPH to present with physical frailty, somatic comorbidity and functional and cognitive problems. Not least, the NPH group were more likely to have made a suicide attempt before admission.
Despite most guidelines recommending that older adults with recent presentation of mental illness should receive specialised psychogeriatric treatment,6–9 there are few studies that specifically investigate the characteristics of older adults with no previous psychiatric treatment history of any kind before their first psychiatric admission. In line with our aim to strengthen the empirical basis for how to organise old-age mental health services, our findings add important information about this severely ill group and highlight the multifactorial nature of the problems with which they present in a clinical setting.
Suicidality
There were no statistically significant differences between the NPH and PPH groups with regard to admission because of suicide risk. However, in the NPH and PPH groups combined, the proportion of patients with suicide-risk-related admissions (31.6%) was much lower than that of the total patient cohort regardless of age from the same study (55%).Reference Mellesdal, Kroken, Lutro, Wentzel-Larsen, Kjelby and Oedegaard19 This might seem like a paradox considering the high suicide rates found in older age groupsReference Värnik1 and might indicate that psychiatric services are currently not sufficiently reaching these patients. This hypothesis is further supported by the studies showing that although older adults who end their life have often been in contact with a primary physician shortly before death, somatic problems are usually the topic of the consultation and mental issues such as depression remain undetected.Reference Conwell, Van Orden and Caine28 Moreover, relatively few have had recent contact with specialised psychiatric services.Reference Walby, Myhre and Kildahl29 In other studies reporting on admissions of older adults because of suicide risk, the rates vary from 13.3%Reference Wetterling, Gutzmann and Haupt30 to 48.1%.Reference Carpar, McCarthy, Adamis, Donmezler, Cesur and Fistikci31 However, these studies were set in specialised psychogeriatric units with differing intake criteria, making comparison with our findings difficult. Further, we found that although the patients in the PPH group were more likely to report suicidal ideation at the time of admission, the patients in the NPH group were more likely to have made a suicide attempt, the latter finding being robust for sensitivity analyses controlling for differences in age and organic disorders. This finding might indicate a difference in the expression of suicidality between these two groups, with the PPH group possibly being more likely to verbalise their suicidal ideation and the NPH group being more likely to act on it, which may be important for clinical practice. Cognitive impairment, significantly more common in the NPH group, may complicate suicide risk assessment further.
Diagnostic and pharmacological differences
Organic disorders were diagnosed almost six times more often in the NPH group than in the PPH group. Two previous studies found an association between first admissions in psychiatry and organic psychiatric disorders (ICD-10)Reference Furukawa, Odawara, Yamada, Fujita and Hirayasu16 or organic brain syndrome (DSM-III-R).Reference Shulman, Marton, Fisher and Cohen17 The latter also found that patients admitted to hospital with NPH were more likely to have a concurrent medical problem, corresponding with the HoNOS scores and diagnostic findings in the present study. While affective disorders was the most frequently diagnosed category in the PPH group, nearly a third of the NPH group were diagnosed with an affective episode, corresponding with previous studies showing that late-life depression is commonly encountered in first admissions of older adults in psychiatry.Reference Choi, Rozario, Morrow-Howell and Proctor32,Reference Burke, Roccaforte and Wengel33 Depression is strongly associated with increased suicide risk in elders,Reference Erlangsen, Zarit, Tu and Conwell18 further underlining the importance of detecting and treating the disorder in this age group. Focusing on the important subject of addiction, one tenth of the patients in the study had issues with substance misuse (mainly alcohol), highlighting the clinical importance of these issues in the elderly population, which has been emphasised by previous studies.Reference Aich, Dhungana and Muthuswamy34,Reference Tueth and Zuberi35
The PPH group were prescribed a higher number of psychotropic drugs than the NPH group. However, the numbers in both groups point to a tendency to polypharmacy that is unfortunate given the high risk of adverse effects and interactions from these drugs especially in this age group.Reference O'Mahony, O'Sullivan, Byrne, O'Connor, Ryan and Gallagher3 Of the NPH group, a substantially higher proportion were given antipsychotic drugs than were diagnosed with a psychotic disorder. This may illustrate some of the challenges when treating older adults with cognitive impairment experiencing psychotic symptoms and behavioural difficulties in whom non-pharmacological interventions have failed. While antipsychotics such as risperidone can have an alleviating effect on aggression and agitation in dementia,Reference Devanand, Mintzer, Schultz, Andrews, Sultzer and de la Pena36 caution should be taken in this patient group because of the potentially life-threatening adverse effectsReference O'Mahony, O'Sullivan, Byrne, O'Connor, Ryan and Gallagher3 and limited evidence of a clinically meaningful benefit.Reference Corbett, Burns and Ballard37
Clinical and sociodemographic differences
Although in the total cohort of older adults both gender distribution and mean age were similar to the findings in previous studies,Reference Choi, Rozario, Morrow-Howell and Proctor32,Reference Burke, Roccaforte and Wengel33,Reference Moss, Wilson, Harrigan and Ames38–Reference Chung, Oh, Suh, Lee, Oh and Yoon40 the NPH group were significantly older than the PPH group and a higher proportion were men, the former being a novel finding. One of the very few previous studies that included a subsample of elderly patients with no prior contact with the mental healthcare system reported a similar gender distribution.Reference Shulman, Marton, Fisher and Cohen17 Both age and gender differences may be relevant when reviewing the HoNOS and GAF scores. These indicate that the patients in the NPH group present with a more complex, severe and multifaceted symptomatology and more impaired functioning than the patients in the PPH group, including problems with aggressive or disruptive behaviour, physical illness and disability, cognition and with activities of daily living.
The NPH group being older is probably associated with the high degree of somatic comorbidity, dementia and other organic psychiatric disorders we identified in this group, which was in part confirmed by the analyses adjusting for age. The preponderance of organic and somatic disorders may again be associated with more behavioural difficulties, cognitive problems and a reduced level of functioning, as previously also shown in psychogeriatric populations assessed with HoNOS.Reference Cheung and Strachan41 Regarding gender, prior studies have found that men with advanced dementia are more assaultive than women,Reference Tueth and Zuberi35,Reference Savage42 potentially causing them to be particularly difficult for caregivers to manage and increasing the likelihood of psychiatric admission.Reference Stevenson, Khan and Perumal43 This could in part explain the disproportionate amount of male patients in the NPH group. However, the male preponderance in the NPH group was robust for the age and organic disorder sensitivity analyses. More aggressive behaviour may also in part explain the high rate of involuntary admissions in the NPH group. Furthermore, the decreased cognitive functioning in the NPH group may impair the capacity to consent to voluntary measures. The sensitivity analyses excluding organic disorders and controlling for age indicate that behavioural difficulties, cognitive problems and involuntary referral was in fact associated with age and a diagnosis of organic disorders.
Although the rates of patients in the NPH group who were married or widowed were comparable with that of the average elderly population in Norway,Reference Mørk44 patients in the PPH group were more likely to be divorced or single and living alone at the time of admission. This could be a reflection of the social consequences experienced by many in the PPH group chronically struggling with serious mental illness, possibly decreasing the chance of a stable marriage or partner.Reference Agerbo, Byrne, Eaton and Mortensen45 These findings were strengthened by the fact that single and married status was robust for sensitivity analyses, indicating that the NPH group are more similar to the general elderly population irrespective of age. For patients with functional impairment, the lack of a supportive living partner might be relevant regarding the level of follow-up needed after the admission.
Psychogeriatric transfer and guideline adherence
Despite being the most common destination of transfer in the NPH group, psychogeriatric units actually received less than half of patients in the NPH group. This number might seem low, and could point to psychogeriatric capacity issues and/or indicate that current guidelines are not sufficiently adhered to. As demonstrated by the other findings of our study, it is highly likely that many of these patients have complicating assessment and treatment needs relating to somatic comorbidity, cognitive and functional impairment, which have a higher risk of going unmet at a general adult unit than at an old age psychiatric unit.Reference Abdul-Hamid, Lewis-Cole, Holloway and Silverman12 The question needs to be raised whether general PAUs without any specific geriatric competence or facilitation are adequately suited to meet the needs of this frail patient group. Although most patients with a PPH were transferred from the PAU to general adult psychiatric units, one out of five were transferred to psychogeriatric units. We do not know the reason(s) for psychogeriatric transfer for these particular patients, however, it may be assumed that they were transferred to psychogeriatric units after individual assessment of need, even though their mental illness started before the age of 65. This highlights the fact that while complex assessment and treatment needs were most frequently found in the NPH group, clearly many patients with a PPH also presented with such needs. Although a detailed evaluation of patient transfer practice and comparison of different psychogeriatric intake criteria was not the focus of this article, our findings call for further research into this area.
Strengths and limitations
Strengths of this study are the large number of patients and the complete, prospective recruitment of patients in a defined geographical area. The naturalistic setting that included 95% of all emergency admissions in the catchment area in the study period, combined with a universal free healthcare with (virtually) no competition from private healthcare facilities ensure high generalisability and representability. Demographic information, as well as the variables concerning clinical diagnoses and medications on discharge are robust and nearly complete. Moreover, data registration from hospital records was performed and controlled by well-trained research nurses.
Some limitations apply to the study: a majority of the data, including information on whether or not the patients had any PPH before the age of 65, is restricted by the accuracy of the hospital records from which they were obtained. Our definition of PPH, defined by contact with specialised psychiatric services or not, does not rule out that some patients in the NPH group may have experienced mental health problems at some point in their life that were not treated, treated a long time ago or was in primary care. The clinical ratings were administered by on-call psychiatric residents and reliability scoring was not conducted. There was some missing data for some of the variables, especially the HoNOS. The imputation of these variables should give more precise estimates, as we assume that relevant predictors were included in the conditional imputation model.
Implications of our findings
The present study shows that in patients of ≥65 years admitted to a general adult PAU no previous contact with mental healthcare system is associated with more frequent concurrent problems relating to physical frailty, somatic comorbidity and functional and cognitive impairment, as well as higher rates of preadmission suicide attempts. Even though cognitive and somatic findings were associated with the NPH group being older and more frequently diagnosed with organic disorders, several characteristics of the NPH group were robust for age correction even after exclusion of patients with organic disorders. Still, the main aim was to investigate if a crude division of elderly patients with and without former psychiatric treatment captures a distinct clinically relevant subcohort, which we conclude that it did. As psychogeriatric units are superior to general adult psychiatric units at providing elderly patients with comprehensive medical and psychiatric work-up,Reference Yazgan, Greenwald, Kremen, Strach and Kramer-Ginsberg11 as well as meeting the multi-faceted needsReference Abdul-Hamid, Lewis-Cole, Holloway and Silverman12 undoubtedly present in this patient group, our findings support the current recommendation of several psychogeriatric guidelines of assigning elderly patients to either geriatric or general psychiatry based on the age at onset of mental illness.
Subdividing patients to treatment in psychogeriatric services based on the age of mental illness presentation is a practical and unequivocal approach and may be especially clinically useful in a busy acute unit when triaging the needs of elderly psychiatric patients. As it was not within the scope of our study, we cannot offer a substantial evaluation of ‘ageless’ psychogeriatric intake criteria based on individual assessment of need;10 however, our findings clearly show that needs typically indicating psychogeriatric rather than general psychiatric treatment more commonly occur in elderly patients with onset of mental illness >65 years. In any case, our findings highlight the multifactorial problems of this severely ill patient group and call attention to the importance of any admitting facility being adequately suited to manage them. Future research in this field should focus on longitudinal data such as causes of death, suicide, re-admissions to hospital as well as somatic comorbidity and complications, further evaluating the current system treating the most ill elderly psychiatric patients. We will endeavour to investigate follow-up data of the present cohort in future publications.
Supplementary material
Supplementary material is available online at http://doi.org/10.1192/bjo.2020.45.
Data availability
The data are not publicly available due to restrictions given by the Committee for Medical Research.
Acknowledgements
The authors thank Jill Bjarke, RN, Geirr Fitje, BBA, Petter Jacobsen, RN, Linn Aaberg, RN, Anne Synnøve Thomassen, RN and Marianne Langeland, RN for their contribution to the high quality of the data.
Author contributions
H.L.-H. drafted the manuscript, participated in data analysis and interpretation of data. E.K. helped draft the manuscript and made substantial contributions to project design and the analysis and interpretation of the data. L.M. helped draft the manuscript, provided expertise in the field of suicidology and participated in project design and interpretation of data. R.G. helped draft the manuscript and supervised data analysis and interpretation. G.S. helped draft the manuscript and provided expertise in the field of geriatric psychiatry. R.A.K. helped draft the manuscript and contributed to project design and interpretation of data. E.J. helped draft the manuscript and contributed to project design and interpretation of data. K.J.O. was a principal investigator during data collection and helped draft the manuscript. L.S.M. helped draft the manuscript and made substantial contributions to project design, data collection, data analysis and interpretation.
Funding
This project was supported by a research grant from the Western Norway Regional Health Authority.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjo.2020.45.








eLetters
No eLetters have been published for this article.