Understanding how subject characteristics influence the outcomes of alcohol use disorder (AUD) treatment is crucial for clinical practice. Regardless of treatment modality, factors predictive of treatment outcome may improve personalised interventions, address the needs of specific subgroups and influence treatment planning and prognostic considerations. Reference Adamson, Sellman and Frampton1,Reference Dale, Heather, Adamson, Coulton, Copello and Godfrey2 Despite numerous investigations of outcome predictors, there is still uncertainty regarding how patient characteristics and attendance in treatment influence AUD treatment outcomes.
The severity of alcohol problems or alcohol consumption pretreatment, Reference Adamson, Sellman and Frampton1,Reference Dale, Heather, Adamson, Coulton, Copello and Godfrey2 a history of previous AUD treatment Reference Haug and Schaub3 and level of education Reference Haug and Schaub3,Reference Durazzo and Meyerhoff4 are among subject characteristics that have been suggested as potential predictors of poor outcomes following treatment. Other risk factors include physical health and comorbid medical problems, Reference Durazzo and Meyerhoff4 lack of social support or pro-drinking networks, Reference Dale, Heather, Adamson, Coulton, Copello and Godfrey2,Reference Hunter-Reel, McCrady, Hildebrandt and Epstein5 psychological distress, Reference Adamson, Sellman and Frampton1 certain personality traits Reference Adamson, Sellman and Frampton1,Reference Newton-Howes and Foulds6 and morphological brain changes and neuropsychological impairments. Reference Durazzo and Meyerhoff4,Reference Bates, Buckman and Nguyen7,Reference Le Berre, Fama and Sullivan8 Correspondingly, a literature review examining relapse factors for persons with AUD found that AUD severity, psychiatric comorbidity, comorbid drug use and health and social factors were risk factors for recurrence of drinking. Reference Sliedrecht, de Waart, Witkiewitz and Roozen9 The authors also determined that social networks, self-efficacy and meaning in life were protective factors. However, this review included an array of study designs on AUD and relapse, with conclusions drawn from both clinical and non-clinical populations. Thus, care should be taken in extending these findings to treatment-seeking groups.
Personality disorders and maladaptive personality functioning are common in AUD, Reference Newton-Howes, Foulds, Guy, Boden and Mulder10 with one study estimating a 23.8% prevalence of personality disorders in a sample of individuals from the general population with AUD. Reference Chiappetta, García-Rodríguez, Jin, Secades-Villa and Blanco11 However, prevalence rates vary significantly between studies, and recent research with large samples is lacking. Reference Newton-Howes and Foulds6 Personality problems are related to potentially less favourable treatment outcomes. Reference Newton-Howes and Foulds6,Reference Brorson, Ajo Arnevik, Rand-Hendriksen and Duckert12 They should, therefore, be investigated further because there is a lack of studies examining the association between outcomes in the treatment of AUD and personality. Reference Newton-Howes, Foulds, Guy, Boden and Mulder10
During the past decades, altough cognitive functioning has also been suggested as a critical factor influencing outcomes in AUD treatment, Reference Bates, Buckman and Nguyen7,Reference Le Berre, Fama and Sullivan8 the findings are still inconsistent. There are no clear-cut cognitive profiles of AUD, and the underlying mechanisms explaining exactly how cognitive impairments affect treatment are not fully understood (e.g. Reference Le Berre, Fama and Sullivan8 ).
Furthermore, treatment attendance, such as the number of sessions attended and the related concepts of treatment retention and completion, has also been linked to better outcomes. Reference Haug and Schaub3,Reference Dale, Coulton, Godfrey, Copello, Hodgson and Heather13,Reference Pfund, Hallgren, Maisto, Pearson and Witkiewitz14 However, the findings are inconsistent because other studies have found either no or weak associations among treatment attendance, duration of treatment and outcome. Reference Cutler and Fishbain15,Reference Kramer Schmidt, Bojesen, Nielsen and Andersen16
Complicating the matter further, there is no agreed-upon definition of what constitutes a favourable AUD treatment outcome. Reference Sliedrecht, Roozen, de Waart, Dom and Witkiewitz17 Some people aim for complete abstinence, others for controlled drinking or harm reduction. Reference Paquette, Daughters and Witkiewitz18 Thus, the term relapse has different connotations depending on the treatment goal, and literature reviews have found no uniform definition of this concept, Reference Sliedrecht, de Waart, Witkiewitz and Roozen9 with some arguing for abandoning the concept altogether. Reference Sliedrecht, Roozen, de Waart, Dom and Witkiewitz17 In addition, there has been a call for outcome definitions to move beyond the binary drinking outcomes of complete abstinence or drinking. Reference Witkiewitz, Wilson, Pearson, Montes, Kirouac and Roos19 Drinking reduction, or controlled drinking, is established as a viable goal in research. Reference Henssler, Müller, Carreira, Bschor, Heinz and Baethge20 AUD treatment in Norway also considers drinking reduction an option for a number of individuals.
In the present paper, we aimed to investigate how baseline patient factors and treatment attendance predict drinking outcomes (high- or low-risk drinking) at the end of treatment. As a naturalistic study examining individuals in standard substance use disorder (SUD) treatment clinics, variables were selected based on the characteristics and factors usually examined by clinicians in routine practice. These factors are important for understanding the individual’s course through the treatment, in particular in identifying attributes that signal the risk of poor treatment outcomes and the need for personalised interventions. We also ensured that the measures used were widely available and feasible for administration by clinicians. We chose the outcome variable of low- versus high-risk drinking, because this will include individuals having either reduced or gained control over their alcohol use.
Method
Participants and procedures
This study used data from a multisite, longitudinal, prospective study on patient factors predicting outcomes in group treatment of AUD. One hundred and thirty-six participants were recruited from four treatment sites in Eastern Norway, two out-patient clinics and two residential AUD treatment facilities. The study was approved by the Regional Committee for Medical and Health Research Ethics South-east Norway (REK) (REKid: 125666). All participants signed an informed consent.
Participants were recruited between 2021 and 2023. Data from 92 individuals were used in the analyses for the current investigation; these were participants with data on key variables at treatment start and end. Consequently, the subjects included in this study are classified as treatment completers because they completed the planned episode and were available for assessment at the end of treatment. The difference between participants who completed and discontinued treatment was examined and has been published in a separate paper. Reference Høiland, Arnevik, Diep, Mathisen, Witkiewitz and Egeland21 The sample was recruited from referrals to the study sites as part of Norwegian Specialist Addiction Health Services.
All participants had AUD as their primary diagnosis, and all fulfilled the criteria for an ICD-10 diagnosis of F10.1 or F10.2, harmful use of alcohol or alcohol dependence. Ninety per cent of participants had a diagnosis of alcohol dependence or severe AUD.
We did not apply any exclusion criteria, except for (a) not being willing to participate in the baseline assessment for the study or (b) not being able to participate in the baseline assessment for the study due to cognitive, mental or somatic reasons. All patients enrolled in the study began time-limited group treatment at the treatment sites. Patients received what is regarded as standard AUD treatment in Norway, as outlined by the Norwegian Health Directorate, 22 including psychoeducation and psychotherapeutic group treatment. Recruiting from standard treatment facilities representative of the specialist health services allowed us to capitalise on realistic treatment conditions. This increases the possibility of maximising ecological validity and translating findings into clinical practice.
Measures and background information were collected by clinical staff at the different treatment centres at the start and end of treatment.
Measures
Demographic information
Demographic information was retrieved from medical records and interviews with participants. Any missing or discrepant information in medical records was sought for confirmation in the interviews.
Alcohol use
The Alcohol Use Disorders Identification Test (AUDIT) is a validated screening test Reference Saunders, Aasland, Babor, De La Fuente and Grant23 and is currently the instrument used most widely internationally to identify hazardous or harmful drinking. Reference Babor and Robaina24 There is evidence that AUDIT is a sensitive instrument in assessment of alcohol dependence severity in the clinical setting, extending its utility beyond its original use as a brief screening tool. Reference Donovan, Kivlahan, Doyle, Longabaugh and Greenfield25 AUDIT is also frequently used as an outcome measure in alcohol intervention trials. Reference Tan, Shufelt, Behan, Chantara, Koomsri and Gordon26
AUDIT comprises 10 questions yielding a score of between 0 and 40, addressing different areas: consumption, dependence and alcohol-related problems. A score of 0–7 indicates low-risk drinking or abstinence, 8–15 indicates medium-risk alcohol problems, 16–19 indicates high risk and 20–40 indicates a very high risk of alcohol problems. To measure who achieved low-risk drinking or not at the end of treatment, we constructed a binary outcome variable from the AUDIT score: LOW-RISK, abstinence or AUDIT score 0–7, and HIGH-RISK: AUDIT score 8–40. The high-risk group encompassed individuals with any problematic and harmful alcohol use following treatment; previous studies have shown that a cut-off of 8 offers good sensitivity and specificity in detecting harmful consequences of alcohol use. Reference Conigrave, Hall and Saunders27 Participants were instructed to report their alcohol use during the treatment period. To ensure that the historical items on AUDIT did not interfere with the total score, we inspected the consumption items (items 1–3). Participants who did not report present alcohol use on these items were classified as LOW-RISK, even if their scores on the other items exceeded a total score of 7.
Other drug use
Comorbid drug use was measured using the Drug Use Disorders Identification Test (DUDIT), a well-validated, 11-item, self-report questionnaire for drug-related problems. Reference Berman, Bergman, Palmstierna and Schlyter28 Responses are scored on a scale from 0 to 4, and DUDIT yields a maximum score of 44. A total score of 0–1 indicates low risk, 2–19 increasing risk, 20–29 high risk and 30–44 very high risk.
Percentage of treatment attendance
Staff at the different treatment sites recorded participants’ attendance in group treatment. We calculated attendance as a percentage based on the number of sessions attended versus the number of planned sessions that participants were expected to attend. We followed this procedure as the data were collected from routine practice, and the number of treatment sessions that participants could attend varied between sites. The median number of maximum sessions possible to attend across sites was 18, the median percentage of attendance was 84.4% and the individual percentage of attendance varied between 32 and 100.
Neuropsychological functioning
Participants’ neuropsychological functioning was assessed with subtests from the Wechsler Adult Intelligence Scale (WAIS-IV) Reference Wechsler29 and the Delis–Kaplan Executive Function System (D-KEFS). Reference Delis, Kaplan and Kramer30 WAIS-IV is a standardised test of general cognitive ability with ten core and five supplemental subtests. D-KEFS is a comprehensive test battery designed to assess a wide range of verbal and non-verbal executive functions; it consists of nine subtests.
A measure of general intellectual functioning, the General Ability Index (GAI), and three cognitive domain scores describing key cognitive abilities for everyday functioning, were derived from these tests. GAI is presented as IQ scores, with a mean of 100 and standard deviation of 15. All other test scores from WAIS-IV and D-KEFS were transformed into scaled scores, with a mean of 10 and standard deviation of 3.
GAI was estimated from four subtests derived from WAIS-IV: two verbal comprehension subtests (similarities and information) and two perceptual reasoning subtests (block design and visual puzzles). Working memory was assessed using digit span, conditions backward and sequencing.
Mental processing speed was assessed using the colour word test (CWT), conditions 1 and 2, and the trail-making test (TMT), conditions 2 and 3 from the D-KEFS. Last, executive functioning was examined using CWT conditions 3 and 4 and TMT condition 4.
Psychological distress
Psychological symptoms were measured using Symptom Checklist 90 (SCL-90-R), Reference Derogatis31 a self-report inventory of 90 questions scored on a five-point scale (0–4). Psychological distress was described using the General Symptom Index (GSI). SCL-90-R is a measure widely used for psychological distress, also in AUD and SUD populations. Reference Bergly, Nordfjærn and Hagen32
Quality of life
We used the World Health Organization Quality of Life Scale (WHOQOL-BREF) 33 to measure quality of life. This consists of 26 items scored on a 1- to 5-point Likert scale and measures quality of life in four domains: physical health, mental health, social and environmental. Domain scores are scaled in a positive direction: higher scores denote higher quality of life.
Personality functioning
The Severity Indices of Personality Functioning (SIPP-118) measures core elements of maladaptive personality functioning. Reference Andrea, Verheul, Berghout, Dolan, van der Kroft and Bateman34 SIPP-118 contains 118 items covering 16 facets, constituting five higher-order domains: self-control, identity integration, responsibility, relational functioning and social concordance; response categories range from 1 to 4 (entirely disagree to fully agree), with higher total scores indicating more adaptive functioning.
Statistical analyses
STATA/MP (v.18.0 for Windows) was used for statistical analyses. We inspected assumptions of normality using histograms and QQ plots. Chi-square and t-tests were performed to check for gender and age differences in the categorical outcome variable.
To examine the magnitude of change in alcohol use before and after treatment, we computed a change score for participants’ AUDIT between baseline and treatment end.
First, we screened for baseline variables significantly associated with high- or low-risk drinking. We also examined whether the percentage of treatment attendance was associated with the binary drinking outcome. We conducted univariate analyses using two-tailed t-tests, Mann–Whitney U-tests and chi-square tests, depending on the distribution. The P-level was set to 0.05. Due to the large number of bivariate comparisons, we applied a Bonferroni correction to the analyses. Variables that remained significant were included in the binary logistic regression prediction model. Collinearity was examined using Spearman correlations and variance inflation factors (VIFs). The Hosmer–Lemeshow test was used to examine the model’s goodness of fit to the data. Marginal probabilities were estimated with the Delta method.
Results
Univariate analyses
Before analysing predictors of treatment related to alcohol reduction, we needed to assess whether a reduction in alcohol consumption had occurred. The group reduced their drinking while in treatment, and mean change scores between pretreatment and treatment end were 9.66 (s.d. = 11.63) points on AUDIT. This corresponds to Cohen’s d of 0.83, suggesting a large effect size.
There were no significant age or gender differences in the outcome measure at the end of treatment. Table 1 presents the demographic characteristics of the sample at baseline. Around two-thirds of the sample was male, and mean age was 50 years.
Table 1 Demographic characteristics (N = 92)
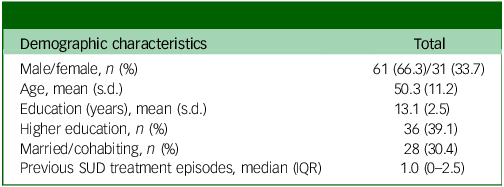
SUD, substance use disorder; IQR, interquartile range.
Table 2 presents the results from the univariate analyses. Pretreatment drinking, other drug use, psychological distress, quality of life and neuropsychological variables pretreatment were not significantly associated with either high- or low-risk drinking at the end of treatment. The personality domains of self-control (P = 0.024) and social concordance (P = 0.021) were initially significant but not following Bonferroni correction. Only the percentage of attendance in treatment and the responsibility domain from SIPP-118 showed significant associations with outcome following Bonferroni correction, and were included in the prediction model.
Table 2 Associations between key variables pretreatment and outcome at treatment end (low- versus high-risk drinking)
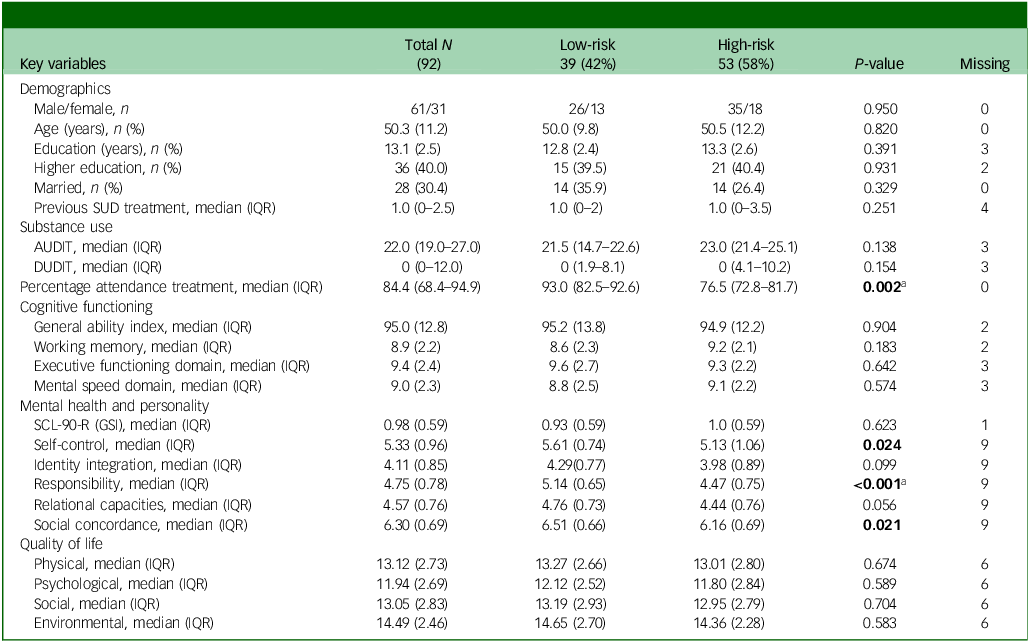
SUD, substance use disorder; IQR, interquartile range; AUDIT, Alcohol Use Disorders Identification Test; DUDIT, Drug Use Disorders Identification Test; SCL-90-R (GSI), Symptom Checklist 90 (General Symptom Index).
a Significant following Bonferroni correction.
All predictor variables were examined at baseline, except for the percentage of treatment attendance. Group differences are described based on two-tailed t-tests, means and standard deviations, or based on Mann–Whitney U-tests, medians and IQR for non-normal variables and chi-square tests for categorical variables.
Mental health: GSI from SCL90-R: personality domain scores from Severity Indices of Personality Functioning; quality of life: domain scores from World Health Organization Quality of Life Scale.
P-values <0.05 are indicated in bold.
Multivariate analyses
The percentage of treatment attendance and the responsibility domain were entered into a binary logistic regression model.
The results are given in Table 3, and show that a 1-unit increase in treatment attendance led to a 4% decrease in the odds of high-risk drinking at treatment end. Likewise, a 1-unit increase in the responsibility domain accounted for a 70% decrease in the odds of high-risk drinking at treatment end. Marginal probabilities were estimated for key values for the predictors in the model: 25% attendance led to a predicted probability of 92% for high-risk drinking at treatment end; at 50% attendance it was 81%, at 75% attendance it dropped to 63% and at 99% attendance the predicted probability of high-risk drinking further decreased to 43%. Similarly, individuals with scores on the responsibility domain at the 25th percentile of the sample had a 73% probability of high-risk drinking at treatment end, those at the 50th percentile 56% probability, those at the 75th percentile 42% probability and those at the 99th percentile 25% probability.
Table 3 Odds ratios for high-risk drinking at treatment end, defined by AUDIT cut-off of 8
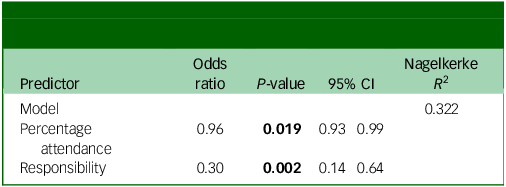
AUDIT, Alcohol Use Disorders Identification Test; percentage attendance, percentage of treatment attended.
Responsibility domain from Severity Indices of Personality Functioning.
P-values <0.05 are indicated in bold.
The model fitted well to the data, as indicated by the Hosmer–Lemeshow test (X 2 [8] = 11.215, P = 0.190). Finally, we examined potential issues with collinearity in the model. Spearman rank-order correlations showed a weak correlation between percentage of attendance and responsibility (r s = 0.28, P = 0.01), suggesting that no strong association between the two variables. A VIF of 1.05 also indicates no issues with collinearity, because VIF <5 indicates low multicollinearity.
Discussion
In the present study, we examined potential predictors of high- and low-risk drinking at treatment end in individuals with AUD in group treatment. Our results showed that the percentage of attendance in treatment had a small but significant influence on high- or low-risk drinking after treatment. However, the personality functioning domain of responsibility was demonstrated to have the most significant impact on drinking level following treatment. Individuals who are more responsible and have the capacity to set and achieve realistic goals are more likely to achieve low-risk drinking or abstinence after completing treatment. Factors found to predict outcomes in other studies, including overall psychological distress, quality of life, the severity of drinking before treatment, other drug use and neuropsychological functioning, were not associated with high- or low-risk drinking at treatment end in the current study.
It is notable that neither general intellectual functioning nor executive functioning affected treatment outcomes in this study. This is an important finding, because it suggests that these individuals may also benefit from standard treatment for AUD, thus arguing against a common belief that they do not. However, individuals with impaired executive functioning may benefit from interventions targeted at retaining them in treatment.
Attendance in treatment has been hypothesised to be an essential factor in improving psychological distress and reducing alcohol use, because it is necessary to attend therapy to benefit from the interventions. As discussed above, research supports this idea (e.g. Reference Dale, Coulton, Godfrey, Copello, Hodgson and Heather13,Reference Pfund, Hallgren, Maisto, Pearson and Witkiewitz14 ), but results are not unequivocal because some studies have failed to find a relationship between attendance and improvement. However, our findings indicate that attendance is important, at least for short-term outcomes, although the effect was not strong. Another factor, the personality domain of responsibility as measured by SIPP-118, had a much more substantial impact on short-term outcomes. This personality domain involves the individual being able to set goals and achieve these goals in line with their expectations and those of others. Furthermore, it is closely related to ‘the big five’ factor of conscientiousness. Reference Bastiaansen, De Fruyt, Rossi, Schotte and Hofmans35,Reference Berghuis, Kamphuis and Verheul36 Thus, it is closely related to the skills necessary to attend treatment. Theoretically, treatment attendance and responsibility can be construed as closely related and dependent upon each other but, in our sample, they were only weakly correlated. Furthermore, the facets of the responsibility domain exceed the capability of attending the sessions. This also reflects the ability to set goals and remember and apply the interventions provided in therapy. As such, it is also connected to the construct of therapeutic alliance, where agreement on tasks and goals is an important factor that predicts outcomes. Reference Magill, Martino and Wampold37 It probably also underlines that the individual is in a position to set a goal of low-risk drinking and abstinence and adhering to it throughout the treatment.
With a mean score on the responsibility domain of 4.47, the high-risk group’s scores are equivalent to those of individuals with one diagnosable personality disorder (mean score of 4.59). Reference Andrea, Verheul, Berghout, Dolan, van der Kroft and Bateman34 The low-risk group had higher scores and, thus, better functioning (mean score 5.14) than individuals who did not meet the criteria for personality disorder in the normative sample (mean score 4.84). Accordingly, individuals with high-risk drinking in our sample may have some degree of personality pathology, but participants were not assessed for personality disorders in the present study. However, we do know from the medical records that few individuals had a previous diagnosis of personality disorder. Whether this is due to the absence of personality pathology or lack of screening and assessment for personality pathology, we do not know.
In addition, responsibility is related to the construct of impulsivity, the ability to inhibit or withhold responses, encompassing both trait and behavioural impulsivity. Reference Sliedrecht, Roozen, Witkiewitz, de Waart and Dom38 There may be some degree of overlap between responsibility and impulsivity, because individuals scoring high on responsibility can control and withhold responses more effectively than those with lower scores. In contrast to responsibility, the construct of impulsivity has attracted considerable research interest and is a driving factor in the initiation of addictive behaviours, Reference Koob and Volkow39 but may also be crucial for treatment outcomes. Reference Sliedrecht, Roozen, Witkiewitz, de Waart and Dom38 In our opinion, responsibility covers a broader set of traits and behaviours and is a viable construct to explore in future studies of individuals with AUD.
Moreover, responsibility may be an important underlying factor explaining the association between other individual factors and treatment outcomes. Findings concerning sociodemographic characteristics and outcomes are inconsistent. Reference Adamson, Sellman and Frampton1,Reference Brorson, Ajo Arnevik, Rand-Hendriksen and Duckert12 Potentially protecting factors, such as caring for children (e.g. Reference Mellentin, Ellermann, Nielsen, Mejldal, Möller and Nielsen40 ), could be a marker of responsibility rather than a causative factor. Future studies should explore whether the ability to act responsibly mediates or moderates sociodemographic findings related to income, marriage or education level.
The clinical implications of the results are twofold: first, it suggests that assessing the current personality functioning of individuals with AUD has beneficial effects on treatment planning. Because the responsibility domain predicts drinking levels at treatment end, clinicians would benefit from knowing which individuals score low on this domain. The association between being responsible and drinking at low-risk levels following treatment is not surprising in itself, but has notable implications from the perspective of personalised medicine. Individuals who are less responsible will probably need more personalised treatment to obtain favourable outcomes. In particular, these individuals may require additional support to complete treatment, and care should be taken to ensure they attend the planned sessions. Second, concerning the therapeutic alliance, it may be necessary to approach individuals with lower levels of responsibility with particular attention, because they also might attend therapy but struggle to commit to therapeutic tasks and goals.
The present study has several limitations. First, we examined alcohol use only at treatment end, which is a short-term outcome. Short follow-up periods are a problem in most studies on AUD treatment outcomes, and future studies should be designed with more extended follow-up periods. Second, our sample is relatively small, possibly affecting the power of the study to detect effects. Relatedly, due to limitations in the data, we had to dichotomise the outcome variable, which necessarily led to a loss of information and statistical power. Third, because the sample mainly consisted of persons who had completed the treatment. the results are therefore probably generalisable only to groups completing treatment. We know from a study of the same sample that those discontinuing treatment had lower executive functioning than those completing treatment, and the latter group constitutes the sample of the current study. Reference Høiland, Arnevik, Diep, Mathisen, Witkiewitz and Egeland21 Other factors may affect individuals who discontinue treatment. In contrast, neuropsychological functioning did not predict drinking outcomes in the present study. Consequently, different factors and paths may predict discontinuation compared with those predicting favourable outcomes upon completing treatment. Fourth, as the majotity of of the sample were out-patients, the results may apply to persons in the higher-level functioning of the AUD spectrum. Fifth, as a study on routine practice, we had limited access to outcome measures other than AUDIT. Using biological markers such as PEth or the Timeline Follow-Back method might have given different and more nuanced results. In addition, aside from attendance, the study used baseline variables as predictors of outcome; more frequent monitoring of outcomes throughout treatment could have offered more detailed information on change trajectories. Future studies with larger samples could investigate these questions, using, for example, latent profile analyses to provide a more nuanced picture of trajectories of change following treatment.
While attendance seems to influence high-/low-risk drinking at the end of treatment, the personality domain of responsibility appears to have a more substantial impact. Strategies to improve attendance, particularly among individuals with low levels of responsibility, would be valuable in enhancing their otherwise poorer prognosis. Clinicians are advised to screen for personality functioning before treatment when planning treatment for those with AUD.
Data availability
The data that support the findings of this study are not publicly available due to confidentiality issues. Please contact the corresponding author with any questions.
Acknowledgements
The authors thank all the individuals participating in the study as well as the staff involved at the treatment sites.
Author contributions
K.H., J.E. and E.K.A.A. conceptualised the study. K.H., J.E. and L.M.D. conducted statistical analyses. K.H. wrote the first draft of the manuscript, with supervision from J.E., E.K.A.A., L.M.D. and A.S.N. All authors contributed substantially to revising and rewriting the final manuscript.
Funding
This work was funded by Vestfold Hospital Trust.
Declaration of interest
The authors have no conflicts of interest to declare.
Trial registration
Clinical Trials ID: NCT04822987, registered 26 March 2021 (https://www.clinicaltrials.gov/study/NCT04822987?id=NCT04822987).






eLetters
No eLetters have been published for this article.