Suicide is a major public health concern globally, affecting not only the individuals but also family members and societies through emotional burden, financial costs and productivity loss.Reference Haagsma, Graetz, Bolliger, Naghavi, Higashi and Mullany1,Reference Tsiachristas, McDaid, Casey, Brand, Leal and Park2 Suicidal behaviours (i.e. ideation and attempts) are major predictors of future suicide, and it is important to understand their prevalence to inform suicide prevention strategies. About three-quarters of global suicides occur in low- and middle-income countries (LMICs), which account for around 75% of the global estimated 800 000 annual deaths by suicide.3 In particular, South Asia represents a fourth of the global population, making it the most densely populated low-resource jurisdiction in the world. A recent scoping review including six South Asian countries reported higher suicide rates when compared with the average global suicides rates.Reference Vijayakumar, Chandra, Kumar, Pathare, Banerjee and Goswami4 Recently, nearly 0.25 million suicide deaths were reported in India, with suicide death rates 2.1 and 1.4 times higher in women and men, respectively, compared with the global average prevalence.Reference Dandona, Kumar, Dhaliwal, Naghavi, Vos and Shukla5,Reference Armstrong and Vijayakumar6 Although rates of suicide attempts in other South Asian countries are lower compared with India – for instance, 3681 suicide attempts were reported in Sri Lanka and 22 675 were noted in Bangladesh – underreporting of suicide-related deaths and injuries, along with lack of available data and low-quality data, may contribute to underestimation of suicide rates in South Asia.Reference Knipe, Gunnell, Pearson, Jayamanne, Pieris and Priyadarshana7–Reference Khan, Ratele, Arendse, Islam and Dery9 In addition, a very recent systematic review reported a 5% pooled prevalence of suicide attempts among women, with young women being at increased risk of suicide attempts.Reference Mazumder, Lugemwa, Shimul, Gain, Hossain and Ward10 This review concurs with the global burden study, which indicated an approximate 10% increment in suicide deaths in women compared with only about a 5% increase in men in the past three decades in India.Reference Dandona, Kumar, Dhaliwal, Naghavi, Vos and Shukla5,Reference Jordans, Kaufman, Brenman, Adhikari, Luitel and Tol11
Suicide and mental illness
Suicidal behaviour and suicide can result from several risk factors, including genetic, biological, childhood, psychological, psychiatric and social influences.Reference Chan, Bhatti, Meader, Stockton, Evans and O'Connor12 People with mental illnesses are especially found to be at increased risk of suicidal behaviour and suicide.Reference Chan, Bhatti, Meader, Stockton, Evans and O'Connor12,Reference Sheehy, Noureen, Khaliq, Dhingra, Husain and Pontin13 Research mainly conducted in high-income countries shows that approximately 90% of people who die by suicide have a mental illness, with affective disorders accounting for 32–47% of cases, followed by schizophrenia (15–20%), personality disorders (8–11%) and alcohol dependence (8–17%).Reference Windfuhr and Kapur14 Psychosis including schizophrenia has a lifetime prevalence of approximately 3%, and bipolar disorder has a lifetime prevalence of approximately 2%,Reference Perälä, Suvisaari, Saarni, Kuoppasalmi, Isometsä and Pirkola15 although these conditions are more common among people with lower socioeconomic status and educational level. Psychosis and bipolar disorder are considered chronic and disabling illnesses, which often worsen over the life course and are linked with higher disability, premature mortality, suicide and medical comorbidities worldwide.Reference Haagsma, Graetz, Bolliger, Naghavi, Higashi and Mullany1,Reference Saha, Chant and McGrath16
Systematic reviews consistently report that individuals diagnosed with psychosisReference Girgis17,Reference Yates, Lång, Cederlöf, Boland, Taylor and Cannon18 and bipolar disorderReference San Too, Spittal, Bugeja, Reifels, Butterworth and Pirkis19,Reference Mork, Walby, Harkavy-Friedman, Barrett, Steen and Lorentzen20 are at increased risk for suicidal behaviour and suicide. Patients with schizophrenia who engage in suicide attempts and non-suicidal self-harm have a distinct clinical profile often showing early onset of symptoms, high rates of repeated suicidal behaviour and treatment delays.Reference da Silva Costa, Alencar, Neto, dos Santos, da Silva and Pinheiro21 Likewise, bipolar disorder is associated with higher odds of suicide attempts compared with unipolar depression, and only a few promising pharmacological treatments have been identified to address suicide risk in people with bipolar disorder.Reference Weintraub, Van de Loo, Gitlin and Miklowitz22,Reference Jefsen, Østergaard, Nielsen and Rohde23 A recent systematic review of observational studies reported that 33.9% of people with bipolar disorder had attempted suicide, with female gender positively associated with lifetime suicide attempts.Reference Dong, Lu, Zhang, Zhang, Ungvari and Ng24
Currently, there is a strong evidence that suicide, suicide attempts and suicidal ideation are prevalent in individuals with psychosis and bipolar disorder. However, this evidence is mainly derived from studies conducted in high-income countries. With over 40% of the poorest population, South Asia has approximately 150–200 million people experiencing psychiatric illnesses.Reference Miller and Black25,Reference Thara and Padmavati26 Despite this, only limited research that has been conducted to understand the prevalence of suicide attempts, suicidal ideation and suicide in these individuals in South Asia. Moreover, no previous systematic review has synthesised the available evidence on the prevalence of suicide, suicide attempts and suicidal ideation in individuals with psychosis and bipolar disorder in South Asia. A recent systematic review synthesised suicide attempts and ideation in South Asia, but was limited to women and did not consider any clinical characteristics of participants.Reference Mazumder, Lugemwa, Shimul, Gain, Hossain and Ward10
To address this major gap in the literature, this systematic review and meta-analysis aimed to examine the prevalence of suicidal ideation, suicide attempts and suicide-related deaths in individuals with psychosis and bipolar disorder in South Asia. The findings would be very helpful for guiding clinicians and policy makers in implementing suicide prevention strategies for high-risk groups in South Asia, such as people with psychosis and bipolar disorder.
Method
The review protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO; registration number: CRD42019159106). We followed the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses for reporting this review.Reference Page, Moher, Bossuyt, Boutron, Hoffmann and Mulrow27
Search strategy and selection criteria
Initially, scoping searches were conducted to identify the relevant search terms. After that, four electronic databases (PsycINFO, Web of Science, EMBASE and Medline) were searched to identify published studies from inception until December 2022. The initial search was carried out in August 2020 and was subsequently updated until December 2022.
The following search terms were used: (‘suicid*’ OR ‘suicid* attempt’ OR ‘self-harm’ OR ‘deliberate self-harm’ OR ‘DSH’ OR ‘fatal self-harm’ OR ‘self-injur*’ OR ‘self-poison*’ OR ‘self-cutting’ OR ‘self-burn’ OR ‘self-mutilation’ OR ‘self-destruction’ OR ‘suicidal intent*’ OR ‘suicidal ideation’ OR ‘suicidal thought*’ OR ‘suicidality’) AND (‘psychosis’ OR ‘psychoses’ OR ‘schizo*’ OR ‘bipolar’ OR ‘affective’ OR ‘mania’ OR ‘severe mental illness*’ OR ‘serious mental illness*) AND (‘prevalence’ OR ‘epidemiology’ OR ‘rate’ OR ‘community based’ OR ‘population-based’ OR ‘cross-sectional’ OR ‘case-control’ OR ‘cohort studies’ OR ‘randomized controlled trial’ OR ‘RCT’). Subsequently, records were limited only to South Asian region with following search terms: (‘South Asia*’ or ‘India*’ or ‘Bangladesh*’ or ‘Pakistan*’ ‘Bhutan*’ or ‘Afghanistan*’ or ‘Maldive*’ or ‘Nepal*’ or ‘Srilanka*’). The reference lists of included studies were also searched to identify potential studies, and corresponding authors were contacted for additional papers in relevant domains (for the complete search history, see Supplementary Material available at https://doi.org/10.1192/bjo.2023.570).
Definition of suicide-related terms
We defined suicide-related terms by referring to the glossary of terms from the United States National Suicide Prevention Strategy,28 whereas definition of psychosis and bipolar disorders were based on the recent version of the DSM-5-TR.
Suicide was defined as death from injury, poisoning or suffocation, where there is evidence that a self-inflicted act led to the person's death. Suicidal ideation was defined as self-reported thoughts of engaging in suicide-related behaviour. Suicide attempt was defined as an act where an individual engages in behaviour that has the potential to cause self-harm, but does not result in a death. However, this act underlies clear evidence that indicates that person intends to kill themselves, although injuries may or may not occur as a result.
Eligibility criteria
We included studies that employed quantitative research designs (e.g. correlational, cross-sectional, prospective designs, longitudinal, case–control, cohort studies, randomised controlled trials), which explored the prevalence of suicidal ideation or attempt or suicide in individuals with psychosis and bipolar disorder. Psychosis, bipolar disorder, suicidal ideation and suicide attempts were identified by examining studies that used a complete or subsection of any standardised diagnostic or monitoring tool, semi- or unstructured clinical interview, case histories, autopsy interviews and/or clinical judgements made by a consultant psychiatrist or psychologist. Given the lack of available data in South Asia and to produce a comprehensive review that utilised all available evidence, no restrictions were placed on mental comorbidity associated with bipolar disorder and psychosis. The South Asian Association for Regional Cooperation includes Afghanistan, Bangladesh, Bhutan, India, the Maldives, Nepal, Pakistan and Sri Lanka. Studies based in countries other than these countries were excluded. We only included peer-reviewed articles written in the English language. We excluded qualitative studies, case studies, narrative reviews, commentary and discussion articles.
Study selection
Four research team members (A.B.K., A. Noureen, Z.U.N. and A.E.) independently screened (in pairs) titles/abstracts, using predefined inclusion and exclusion criteria. Where discrepancies occurred, these were resolved by discussion and the involvement of a fifth reviewer (M.P.), who decided whether studies should be included. Abstracts that did not fulfil the inclusion criteria were excluded. Where it was uncertain if studies meet inclusion criteria, they were retained for the next stage of screening. The full articles were screened by the same team of reviewers and any discrepancies among reviewers were resolved by discussion with the wider team. For any identified conference abstracts, lead authors were contacted to check if they had eligible data.
Data extraction
Initially extraction was conducted between March and August 2021; however, after updating the searches, extraction was further updated in January 2023. A standardised Microsoft Excel, version 365 for Windows spreadsheet was used for data extraction, which was piloted with the first three studies and then further adapted. The independent reviewers (A.B.K., A. Noureen, Z.U.N. and A.E.) extracted the data for each study and agreed on discrepancies. M.P. supervised the data extraction. Data extraction included study characteristics, sample characteristics, study design, methodology and outcomes. Extracted data included study details (author, year, study location), source (peer reviewed), study design information (type of design, number of groups, sampling method, sample population), participant characteristics (target sample, age, gender), measures used (measure of suicidal ideation and suicide attempts, measure of bipolar disorder, measure of psychosis) and prevalence (prevalence of suicide attempts in psychosis and bipolar disorder).
Assessment of risk of bias
Risk of bias for studies included in the review was assessed with an adapted version of the Agency for Healthcare Research and Quality risk-of-bias tool.Reference Williams, Plassman, Burke and Benjamin29 This tool has been used multiple times in reviews related to self-injurious behaviour and its risk factors.Reference Taylor, Hutton and Wood30 The tool assesses the risk of bias across multiple domains, including the representativeness and description of the cohort, the methods utilised to ascertain diagnoses and measure outcomes, and whether analyses were appropriate and consideration of confounding variables. The domains are rated using the terms yes, no, partial and unclear. Two research team members (A. Noureen and Z.U.N.) independently rated the studies and resolved any discrepancies by discussion with team (M.P. and A.B.K.). Ratings were used to identify the similar or common risk of bias and highlight areas of strength.
Analysis
The primary outcome of the analysis was the prevalence of suicide attempts among individuals with psychosis and bipolar disorder in South Asia. Secondary outcomes included the prevalence of suicidal ideation and suicide-related deaths. All data were pooled with the metaprop functionReference Freeman and Tukey31 in Stata version 17 for Windows. Freeman–Tukey random-effects models were used in all meta-analyses. Random effects are generally more conservative and have better properties in the presence of heterogeneity.Reference Borenstein, Hedges, Higgins and Rothstein32–Reference Borenstein, Hedges, Higgins and Rothstein34 Given the expected heterogeneity in studies, random-effects models were utilised. Pooled prevalence was reported as percentages bound by their 95% confidence intervals. Heterogeneity was quantified with the I 2-statistic and estimated 95% confidence interval (0–40%, might not be important heterogeneity; 30–60%, might present moderate heterogeneity; 50–90%, might present substantial heterogeneity; 75–100%, considerable heterogeneity). We conducted subgroup analyses for each condition (psychosis and bipolar disorder), timeframe of suicide attempts and suicidal ideation (lifetime and current), and countries (India and Pakistan). Meta-regressions were performed to examine whether the results were moderated by gender (proportion of females). Sensitivity analyses were conducted to account for variations in study designs (only cross-sectional studies were retained) and risk-of-bias ratings (only studies with low risk of bias were retained).Reference Bender, Friede, Koch, Kuss, Schlattmann and Schwarzer35 We inspected the symmetry of the funnel plots and used Egger's test to examine for publication bias in analyses.Reference Sterne and Harbord36,Reference Egger, Smith, Schneider and Minder37
Results
Figure 1 presents the study selection process. A total of 704 records (647 from databases, 57 from other sources) were initially accessed. Following the removal of duplicates and the title/abstract and full-text screening, 21 studies met the inclusion criteria and were included in the review.
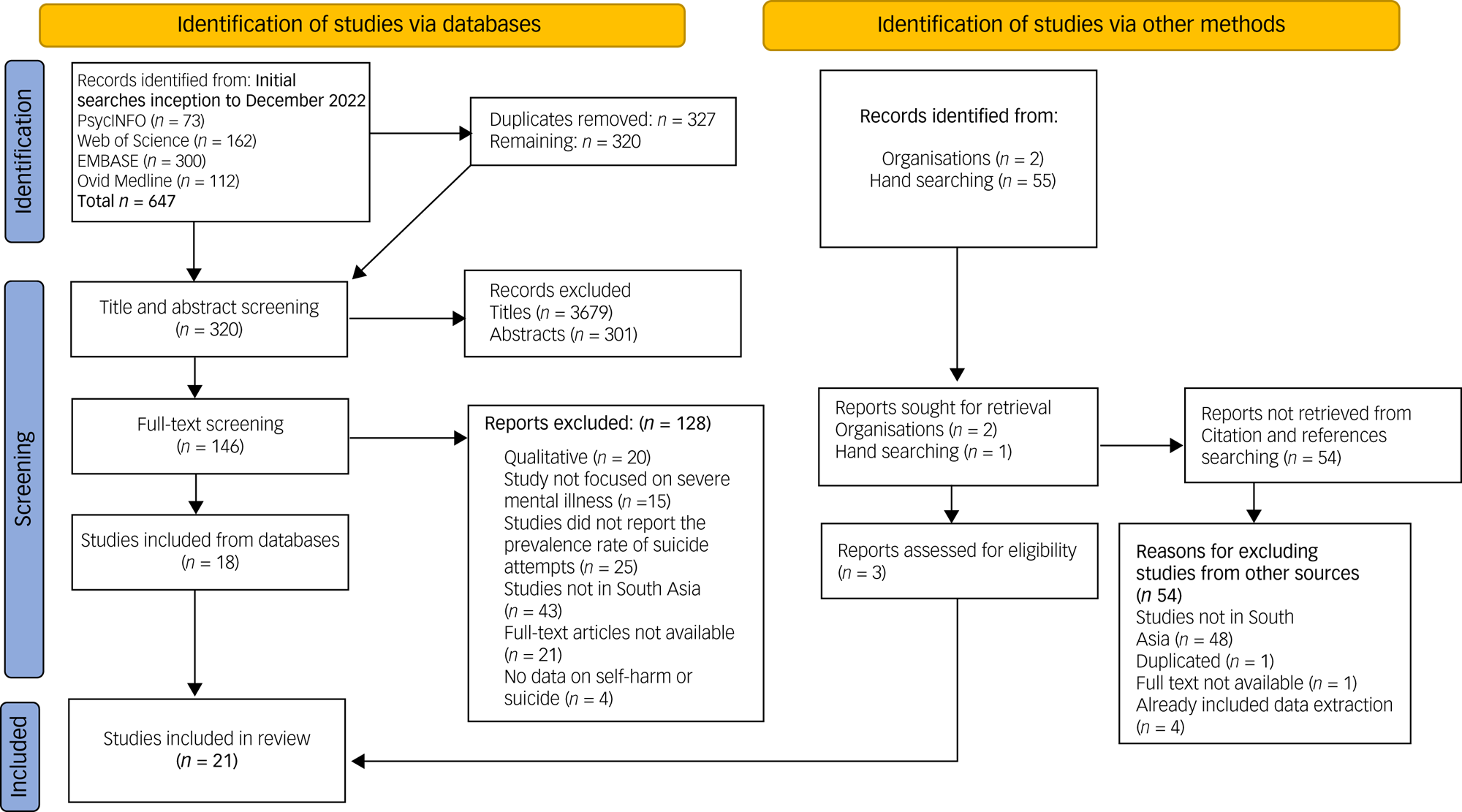
Fig. 1 Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram.
Descriptive characteristics of included studies
The key descriptive characteristics of the included studies are presented in Table 1. The majority of studies took place in India (k = 18; 85%), with two in Pakistan (k = 2; 10%) and only one in Bangladesh (k = 1; 5%). All of the studies involved cross-sectional designs (k = 14; 67%), with the exception of four studies. These four studies involved retrospective longitudinal,Reference Grover, Avasthi, Chakravarty, Dan, Chakraborty and Neogi46 case–controlReference Shrivastava, Berlemont, Campbell, Johnston, De Sousa and Shah56,Reference Manoranjitham, Rajkumar, Thangadurai, Prasad, Jayakaran and Jacob62 and prospective designs.Reference Shrivastava, Johnston, Shah, Innamorati, Stitt and Thakar63 Only one study was based in a community setting and 16 studies were based in hospital settings, including tertiary care mental health facilities and general hospitals. Three studies did not report information about the setting they were based in. The earliest study was published in 2000 and the most recent was published in 2022. The pooled sample size across the 21 studies comprised 3745 participants (psychosis n = 2096, bipolar disorder n = 1676), with a combined slightly higher percentage of males (n = 1941, 51.8%) than females (n = 1804, 48.2%); three studies did not report the gender composition of their sample. Validated psychiatric rating scales such as the Positive and Negative Syndrome Scale and the Mini-International Neuropsychiatric Interview (MINI) were used in 18 studies to diagnose psychosis and bipolar disorder. Three studies relied on clinical judgement by consultant psychiatrists and psychologists, and one study did not provide diagnostic information. For assessing suicidal ideation and attempts, nine studies used validated tools such as the Suicidality – Management, Assessment and Planning of Care and Beck Suicide Inventory. Six studies used subsections of tools like the MINI and Hamilton Rating Scale for Depression, whereas the remaining six employed informal methods like semi-structured or autopsy interviews to assess suicidal ideation and attempts. Fifteen studies (71%) reported data on suicidal attempts, ten (48%) studies reported data on suicidal ideation and only one study reported data on suicide-related deaths. This study reported that two out of 100 individuals with psychiatric morbidity (2%) with schizophrenia died by suicide. Across the 15 studies that reported suicide attempts, three studies reported recent suicide attempts and 12 reported lifetime suicide attempts. Across the ten studies that reported suicidal ideation, seven studies reported recent or current suicidal ideation and three studies reported lifetime suicidal ideation. Fifteen studies (71%) focused on individuals with psychosis, and six (29%) studies focused on people with bipolar disorder. Four studies took an inverse approach and examined the prevalence of psychosis and bipolar disorder in South Asian people who had attempted suicide or thought about suicide.
Table 1 Study characteristics and prevalence of suicidal ideation and attempts in psychosis and bipolar disorder
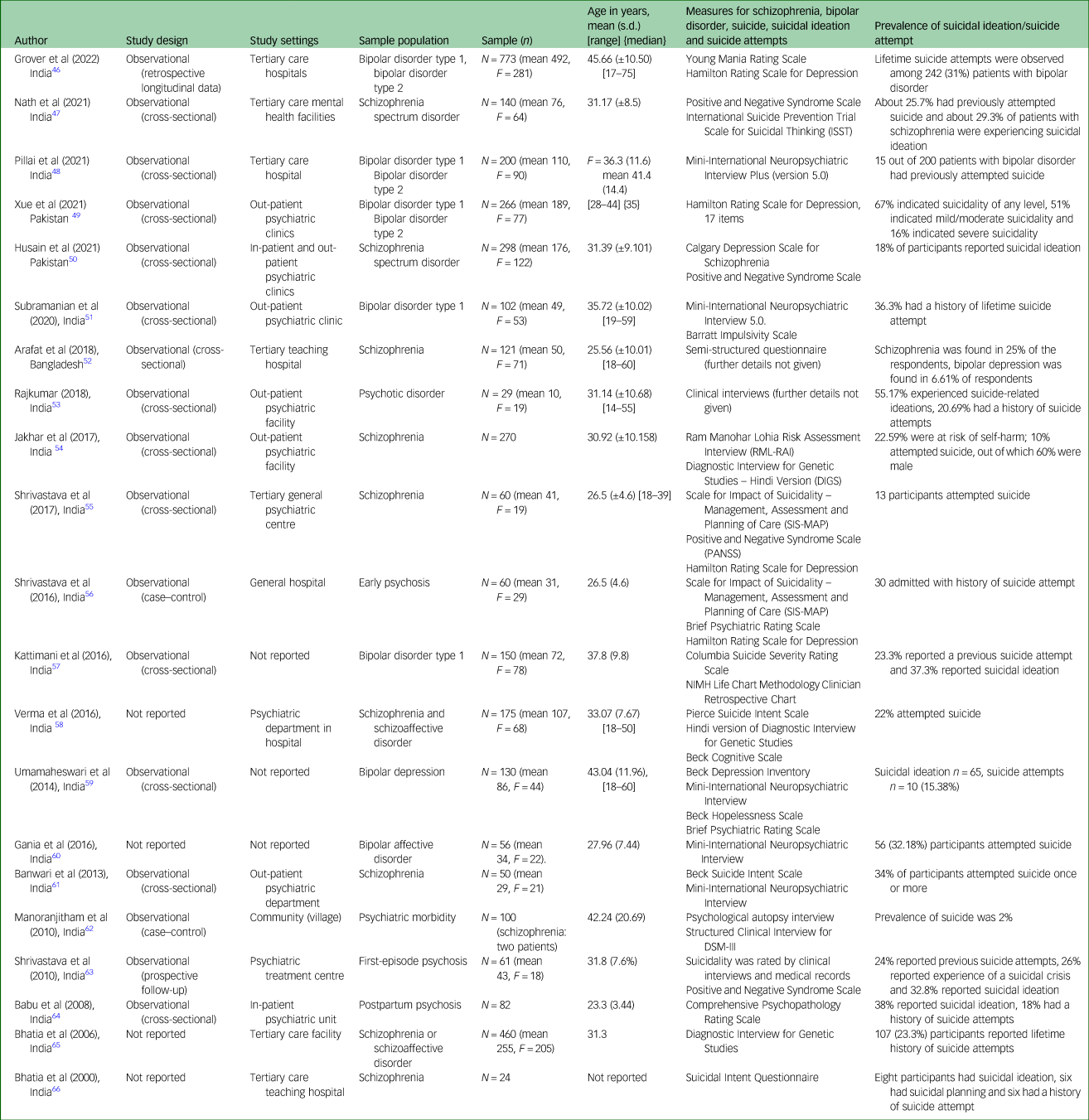
Studies are presented in reverse chronological order.
Risk-of-bias assessment
The detailed results of the risk-of-bias assessment are presented in the Supplementary Material and Table 2. Fifteen studies (71%) at least partially met the criteria of the risk-of-bias assessment, indicating low risk of bias. The most common methodological problems were related to the measurement of the outcome, missing data, blinding of researchers and control of confounders in analyses. All studies used appropriate method of analysis. Suicidal ideation and attempts were mostly determined with single self-report items or continuous subscale measures such as the Calgary Depression Scale for Schizophrenia.
Table 2 Overview of assessment of study methodological quality and risk of bias

Studies are presented in reverse chronological order.
Prevalence of suicide attempts
The pooled prevalence of suicide attempts in South Asian people with either psychosis or bipolar disorder was 22% (95% CI 17–27, n = 15 studies). Overall, there were large variations across the studies, as indicated by substantial to considerable heterogeneity (I 2 = 87.65%, P = 0.000).
In terms of specific diagnoses, the pooled prevalence of suicide attempts in people with psychosis was 21% (95% CI 17–26, I 2 = 73.30%, n = 10), and the pooled prevalence of suicide attempts in people with bipolar disorder was 23% (95% CI 13–35, I 2 = 94.2%, n = 5) (see Fig. 2).
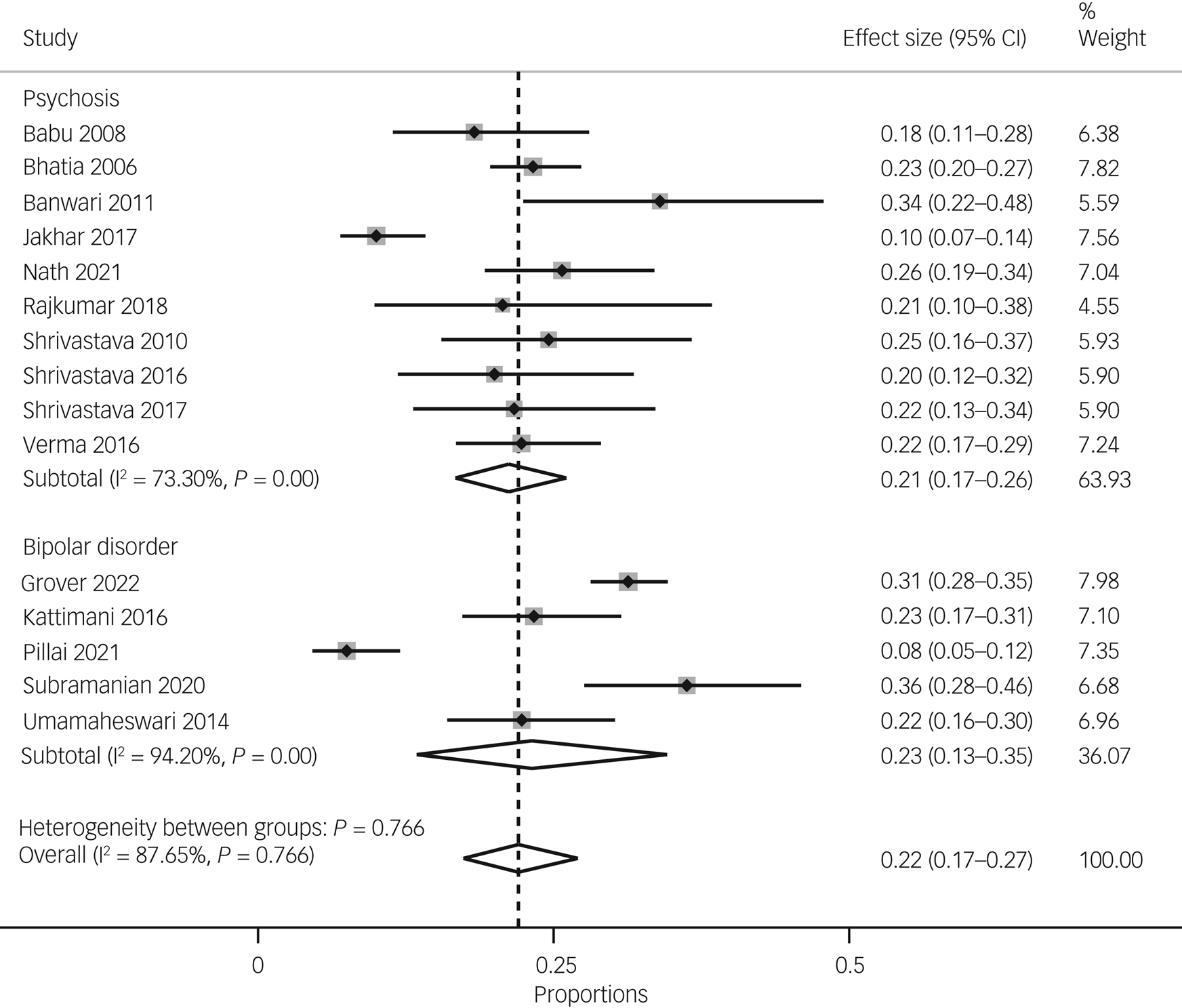
Fig. 2 Pooled prevalence of suicide attempts overall and by diagnosis (i.e. psychoses versus bipolar disorder).
The pooled prevalence of recent or current suicide attempts was 21% (95% CI 16–26, I 2-statistic unavailable because of the small number of studies, n = 3), whereas the pooled prevalence of lifetime suicide attempts was 22% (95% CI 17–28, I 2 = 90%, n = 10) (see Fig. 3).

Fig. 3 Pooled prevalence of suicide attempts overall and by duration (lifetime versus current).
We performed sensitivity analysis by retaining cross-sectional studies and studies with low risk of bias. We removed two retrospectiveReference Grover, Avasthi, Chakravarty, Dan, Chakraborty and Neogi46 and prospectiveReference Shrivastava, Johnston, Shah, Innamorati, Stitt and Thakar63 studies, as well as all studies with high risk of bias. We found no significant differences in pooled prevalence (dropped from 21 to 19%, but confidence intervals for both estimates overlapped) and heterogeneity levels of suicide attempts (see Supplementary Fig. 1).
Meta-regression did not reveal a significant association between the proportion of females and the pooled prevalence of suicide attempts (see Supplementary Table 1).
Visual representation of the funnel plot indicated slight uneven distribution of study estimates against inverse standard error (see Supplementary Fig. 3), but Egger's test formally indicated the absence of any significant asymmetry in the funnel plot (beta1 = −0.03, z = −0.03, P = 0.97).
Prevalence of suicidal ideation
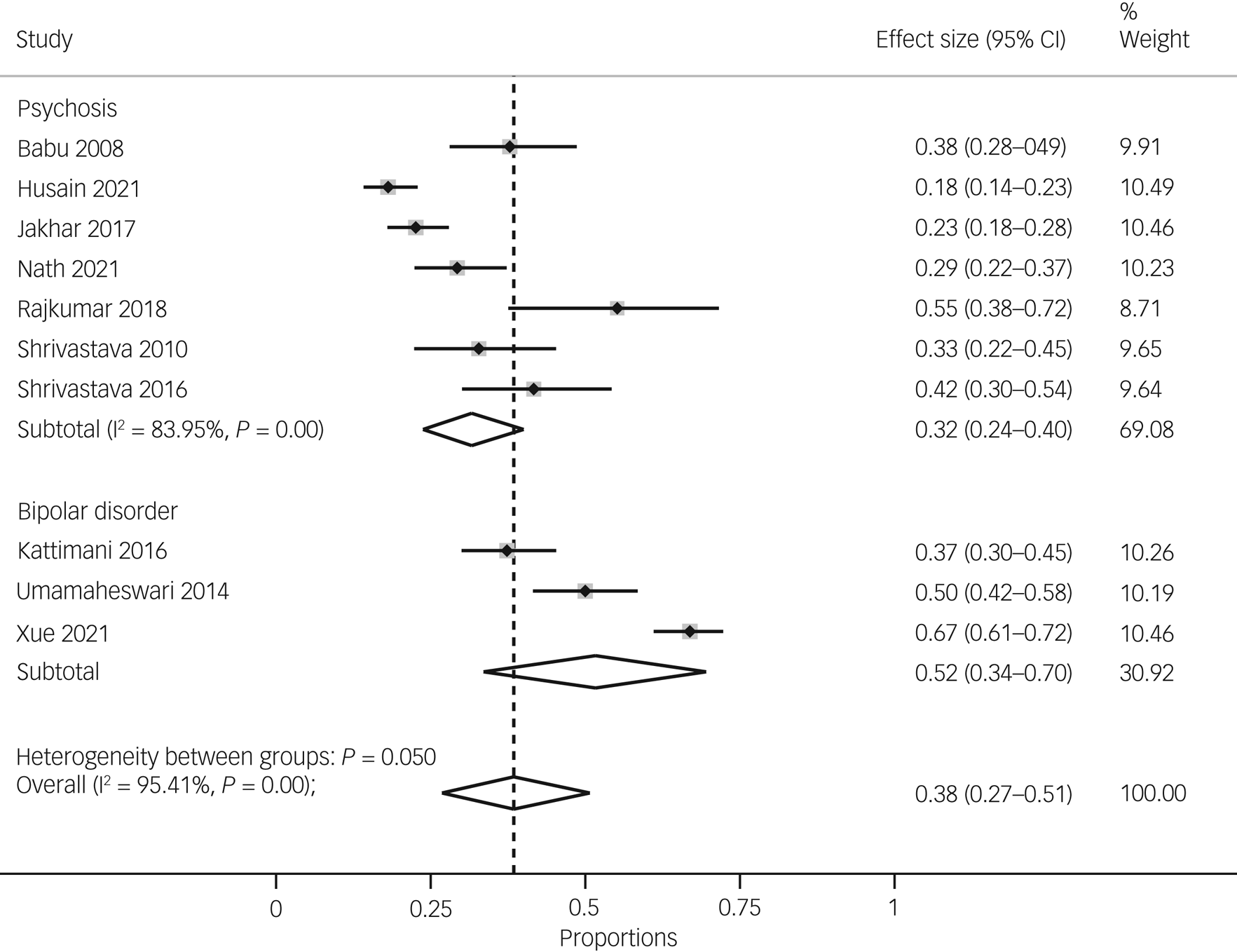
The pooled prevalence of suicidal ideation for South Asian people with either psychosis or bipolar disorder was 38% (95% CI 27–51, n = 10), with considerable heterogeneity (I 2 = 95.41%, P = 0.000).
In terms of specific diagnoses, the pooled prevalence of suicidal ideation in psychosis was 32% (95% CI 24–40, I 2 = 83.95%, n = 7), and the pooled prevalence of suicidal ideation in bipolar disorder was 52% (95% CI 34–70, I 2-statistic was unavailable because of the small number of studies, n = 3). There was considerable between-group heterogeneity (P = 0.05), indicating a higher rate of suicidal ideation in bipolar disorder compared with psychosis, but there were fewer studies in the bipolar disorder subgroup (see Fig. 4).

Fig. 4 Pooled prevalence of suicidal ideation overall and by diagnosis (i.e. psychoses versus bipolar disorder).
The pooled prevalence of recent or current suicidal ideation was 37% (95% CI 23–54, I 2 = 96.87%, n = 7), and the pooled prevalence of lifetime suicidal ideation was 39% (95% CI 30–50, I 2-statistic was unavailable because of the small number of studies, n = 3) (see Fig. 5).

Fig. 5 Pooled prevalence of suicide ideation overall and by duration (lifetime versus current).
The pooled prevalence of suicidal ideation in psychosis and bipolar disorder did not differ between India (37%, 95% CI 29–45%, n = 8) and Pakistan (40%, 95% CI 36–44%; I2-statistic unavailable because of the small number of studies, n = 2) (see Fig. 6).

Fig. 6 Pooled prevalence of suicide ideation overall and by countries.
Meta-regression did not show a significant association between the proportion of females and pooled prevalence of suicidal ideation (see Supplementary Table 2). After removing the studies with high risk of bias, the overall prevalence for suicidal ideation remained similar (see Supplementary Fig. 2).
The funnel plot showed that a few study estimates gathered on the top side of graph, indicating potential asymmetry (see Supplementary Fig. 4); however, Egger's test was non-significant (beta1 = 1.09, z = −0.65, P = 0.51).
Discussion
Summary of main findings
This is the first systematic review and meta-analysis examining the prevalence of suicide attempts, suicidal ideation and suicide among individuals living with psychosis and bipolar disorder in South Asia. The findings suggest that both suicide attempts and suicidal ideation are highly prevalent in South Asian individuals living with psychosis and bipolar disorder. Approximately one in four individuals with psychosis and bipolar disorder reported suicide attempts, and up to one in three individuals with psychosis and bipolar disorder reported suicidal ideation. Both suicidal ideation and attempts were more prevalent in people with bipolar disorder. Despite our comprehensive approach, we found scarce evidence about the prevalence of suicide-related deaths in people living with psychosis and bipolar disorder in South Asia.
Comparison with previous literature
Our pooled prevalence estimates of suicidal attempts were nearly similar with the pooled estimates of previous meta-analyses of studies mainly based in high-income countries. These include recent meta-analyses that have shown that the prevalence of lifetime suicide attempts is 33.9% in people with bipolar disorder,Reference Dong, Lu, Zhang, Zhang, Ungvari and Ng24 18% in people with first-episode psychosis and 11% in people with psychosis after 7 years of treatment.Reference Perez38,Reference Hettige, Bani-Fatemi, Sakinofsky and De Luca39 It is likely that the small sample sizes of most of the studies included in our analyses might have inflated our pooled prevalence estimates of suicide attempts. However, these high estimates may also reflect the concurrent presence of several risk factors for suicidal attempts among people with psychosis and bipolar disorder living in South Asian countries, including unemployment, low education level, low socioeconomic class, stigma toward mental illnesses and no reliable official data.Reference Gajalakshmi and Peto40,Reference Trivedi, Goel, Kallivayalil, Isaac, Shrestha and Gambheera41
Implications for researchers, clinicians and policy makers
The review focused on the prevalence of suicide attempts, suicidal ideation and suicides among people with psychosis and bipolar disorder in South Asian countries, where suicide risk often remains under-addressed because of several common challenges, such as unemployment, disparities in health systems, poverty, the limited number of health professionals and limited investment in health by the government.Reference Hossain, Hasan, Sultana and Faizah42 The main implication of our findings is that suicidal ideation and suicide attempts among individuals with psychosis and bipolar disorder in South Asia are major, but overlooked, clinical and research concerns. Our pooled prevalence estimates of suicide attempts and suicidal ideation are high, but not definitive, because of the small number and low methodological quality of studies that have been conducted in South Asian countries. National epidemiological surveys and prospective studies are needed to accurately estimate the prevalence of suicides, suicide attempts (at present and lifetime) and suicidal ideation (at present and lifetime) in South Asia, and to identify subgroups of patients with psychosis and bipolar disorder that are at higher risk of suicide (e.g. based on health, demographic and social characteristics). Given the disproportionately higher burden of mental illness and suicide in LMICs, as well as the stigma associated with mental illness and suicide, it is imperative to address this global health concern by continuing to build on the sparse evidence base, to inform the development of cost-effective prevention strategies and policies in these settings.
In terms of clinical practice, the results highlight how important it is for clinicians to routinely assess and monitor suicidal ideation and suicide attempts in individuals with psychosis and bipolar disorder in South Asia. The lack of effective training of clinicians in suicide risk assessment, and the stigma and legal implications of suicide in South Asia, are key reasons why suicide attempts and suicidal ideation remain undetected and untreated. Many of the South Asian countries do not have effective policies, legislations, strategic plans, programmes and other instrumental measures to address mental health problems across communities.Reference Gajalakshmi and Peto40–Reference Hossain, Hasan, Sultana and Faizah42 National policies and investments are therefore needed to develop culturally relevant, acceptable and effective suicide prevention strategies for individuals living with psychosis and bipolar disorder.
Strengths and limitations
This is the first systematic review and meta-analysis to estimate the prevalence of suicidal ideation, suicide attempts and suicide in individuals with psychosis and bipolar disorder in South Asia. Given the dearth of literature on the topic, we combined lifetime and current suicide attempts in the analysis and included any observational study designs (although the majority of the studies were cross-sectional), to provide a comprehensive understanding of the overall prevalence of suicide attempts and suicidal ideation regardless of timeframe, and to make use of all available data. This review has several important limitations. The prevalence of suicidal attempts and suicidal ideation varied considerably across studies, as did the methods for their assessment. For example, variations in the timeframe of suicide attempts or suicidal ideation (current or lifetime) might be important when interpreting the differences in the prevalence estimates. A related concern is that across half of the studies (n = 9), it was unclear when did the suicidal attempt and suicidal behaviour occurred and whether it coincided or preceded the emergence of psychosis or bipolar disorder. Large longitudinal studies in community settings are needed to better understand the patterns of suicidal behaviours in people with psychosis and bipolar disorder; for example, to determine the timeframe and phase of illness in which they appear, and their duration and impact. Additionally, the measures used to assess suicidal ideation and attempts in the review were often single item and subscales taken from other instruments. Future research in South Asia would benefit from validated and dedicated measures of suicide attempts and suicide. The COVID-19 pandemic has greatly affected people with and without mental illnesses. Our updated searches did not find any eligible study on suicidal ideation and attempts among individuals with psychosis and bipolar disorder in South Asia during the COVID-19 pandemic. Finally, we do not know the severity and length of illness of participants with psychosis and bipolar disorder in the included studies. This could affect the prevalence estimates of suicidal ideation and behaviours; for example, in first-episode psychosis, the risk of suicidal attempts and suicide is greater in the beginning of the disease course.Reference Hossain, Hasan, Sultana and Faizah42 Similarly, suicide attempts and suicide in bipolar disorder vary significantly between illness phases, with mixed and depressive phases having the highest risk.Reference Challis, Nielssen, Harris and Large43–Reference Holma, Haukka, Suominen, Valtonen, Mantere and Melartin45 Future studies should also consider the severity and duration of illnesses, to better understand the phenomenon of suicidal ideation and behaviours.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2023.570
Data availability
The data that support the findings of this study are available from the corresponding author, A.B.K., on reasonable request.
Author contributions
A.B.K., A. Noureen, Z.U.N., A.E., U.A., A. Naz and M.A. completed the screening of the titles, abstracts and full-text papers, and contributed to drafting the manuscript. A.H. and M.M.B. performed the statistical analysis. M.P., A.H. and M.M.B. contributed to the interpretation of results and drafted the manuscript. M.P. also supervised the review throughout its completion. N.H. and M.P. conceived the idea and contributed to drafting the review. I.B.C., M.O.H., M.I.H. and N.C. contributed to drafting the review. All authors have read and approved the final review.
Funding
This review has been funded by the Global Challenges Research Fund-South Asia Self-Harm and Suicide Reduction Movement (grant number MR/P028144/1) awarded to Pakistan Institute of Living and Learning (SASHI awarded to University of Manchester) and the Medical Research Council/Department of International Development/National Institute of Health and Care Research–funded youth self-harm and suicide prevention programme (grant number MR/R022461/1) awarded to University of Manchester, and was partly funded by the Pakistan Institute of Living and Learning (grant number PILL/R0163) awarded to Division of At-Risk Mental State and Schizophrenia Spectrum and other Psychotic Disorders. The funders had no role in the review design, collection, analysis or interpretation of the data, writing of the review or the decision to submit the manuscript for publication.
Declaration of interest
I.B.C. and N.H. report giving lectures and advice to Eli Lilly, Bristol Myers Squibb, Lundbeck, AstraZeneca and Janssen Pharmaceuticals, for which they or their employing institution have been reimbursed. N.H. and I.B.C. report previously being trustees of the Pakistan Institute of Living and Learning. N.H. also reports being the Trustee of Manchester Global Foundation, a charitable incorporated organisation registered in England and Wales, and was a past Trustee of Lancashire Mind and Abaseen Foundation, UK. N.H. is also NIHR senior investigator and Director of Research and Innovation at Mersey Care NHS Foundation Trust. None of the companies listed above have a financial interest in this research. M.I.H. is a member of the BJPsych Open Editorial Board. He did not take part in the review or decision-making process of this paper. All other authors declare no competing interests.











eLetters
No eLetters have been published for this article.