Admission criteria for high secure hospitals
Secure forensic services in England provide care and treatment to mentally disordered offenders at high, medium and low levels of therapeutic security.Reference Duke L, Furtado, Guo and Vollm1,Reference Rutherford and Duggan2 Admission criteria for high secure hospitals have rarely been studied. Patients admitted to these secure units, particularly at the higher levels of security, typically have very complex needs including treatment-resistant mental illness, personality disorder, neurocognitive diagnoses and substance misuse.Reference Coid, Kahtan, Gault, Cook and Jarman3 There are also high rates of comorbidity of the above disorders seen among this very vulnerable group.Reference Coid, Kahtan, Gault, Cook and Jarman3 The majority of secure admission beds are in medium- and low-security hospital units, with only a small number reserved for high secure care.Reference Duke L, Furtado, Guo and Vollm1,Reference Rutherford and Duggan2 High secure care in England is provided at three hospitals, Broadmoor serving London and the South of England, Ashworth Hospital serving Merseyside and the West and Rampton High Secure Hospital, which serves the North of England but also provides the national high secure services for women and for those with intellectual disability.
Admission to high secure services in England requires careful assessment and consideration. To admit a patient to a higher level of therapeutic security than absolutely necessary is a human rights issue as the individual may be subject to unnecessary restriction. This also has resource implications as high secure forensic admission beds are scarce and expensive.Reference McCrone4,Reference Kennedy5 Admitting patients to too low a level of therapeutic security places fellow patients and staff at risk.Reference Kennedy5 It also limits the ability of therapists to safely challenge patients, which is a key component of therapeutic security, as appropriate challenge is inherent in all effective therapy. Therefore, careful assessment of the security needs of those referred for high secure care is essential for safe and effective running of mental health services in any jurisdiction. We identified only one study to date that systematically examined admission processes for high security hospitals.Reference Brown and Lloyd6
Background
In the early 1990s the National Health Service (NHS) England completed a large scale evaluation of the mental health and security needs of those who were, at that time, detained in conditions of high therapeutic security.7 A significant cohort of individuals in high secure settings who could have been managed at lower levels of therapeutic security were identified. This led to the development of additional medium secure units across England and large numbers of patients were appropriately transferred to these units.Reference Coid, Kahtan, Gault, Cook and Jarman3 At present in the three high secure hospitals, there is much oversight of those admitted to high secure services, but also clinicians are expected to frequently review the ongoing security needs of in-patients with a view to transferring people out to medium secure units as soon as it is safe to do so. As a result, the high secure services in England now work with a smaller number of more unwell, more acutely disturbed individuals with much higher security needs than in the past.
Needs assessment tool for secure care
The DUNDRUM-1 toolkit is a set of structured professional judgement instruments designed to assess a patient's need for secure care.Reference Kennedy, O'Neill, Flynn, Gill and Davoren8 It is a needs assessment, not a violence risk assessment, although history of violence clearly plays a role in any such assessment. The tool consists of five parts, the DUNDRUM-1 triage security scale and the DUNDRUM-2 triage urgency scale are designed to assess the level of security a patient should be admitted to and the urgency of need for admission, respectively.Reference Kennedy, O'Neill, Flynn, Gill and Davoren8–Reference Flynn, O'Neill and Kennedy10 The DUNDRUM-3 programme completion scale and the DUNDRUM-4 recovery scale are dynamic scales designed to assess a patient's current readiness to move to a less secure setting, for example transfer from high secure care to medium secure care, or medium secure care to low security or to the community.Reference Kennedy, O'Neill, Flynn, Gill and Davoren8,Reference Davoren, O'Dwyer, Abidin, Naughton, Gibbons and Doyle11,Reference Davoren, Abidin, Naughton, Gibbons, Nulty and Wright12 The fifth scale is the self-rated DUNDRUM scale that is designed to allow a patient to self-rate their own readiness to move to a less secure setting, i.e. to rate their own forensic recovery.Reference Kennedy, O'Neill, Flynn, Gill and Davoren8,Reference Davoren, Hennessy, Conway, Marrinan, Gill and Kennedy13 It is a mirror image of the programme completion and recovery scales. The DUNDRUM tools have been validated in forensic mental health hospital settings and prison settings in multiple jurisdictions and have excellent psychometric properties.Reference Flynn, O'Neill, McInerney and Kennedy9,Reference O'Dwyer, Davoren, Abidin, Doyle, McDonnell and Kennedy14–Reference Habets, Jeandarme and Kennedy17 The DUNDRUM-1 triage security scale has been shown to have good internal consistency (Cronbach's alpha 0.95 in a Dundrum sample validation and 0.77 in an international validation study) and good interrater reliability.Reference Flynn, O'Neill, McInerney and Kennedy9,Reference Flynn, O'Neill and Kennedy10,Reference Freestone, Bull, Brown, Boast, Blazey and Gilluley15–Reference Lawrence, Davies, Bagshaw, Hewlett, Taylor and Watt19 Interrater reliability is better following training.Reference Habets, Jeandarme and Kennedy17
Objectives
The aim of our study was to analyse the security needs among referrals to the admission panel at Broadmoor High Secure Hospital over a 2-year period. We also aimed to ascertain if there were differences between referrals to the mental illness pathway and the personality disorder pathway, in terms of security needs or urgency of need for admission to hospital.
Method
Study design
This was a retrospective cohort study comprising a complete cohort of all those referred for admission to Broadmoor Hospital from prisons or medium secure hospitals over a 2-year period, from 2015 to 2017. This comprised a total of 204 referrals. One patient transferred into Broadmoor from another high security hospital during the period of the study and was excluded.
All referrals to Broadmoor Hospital come with a request for admission from a psychiatrist detailing in a referral letter the reasons why high secure admission is being requested. Once a referral is received the patient will be reviewed by a consultant forensic psychiatrist or specialist registrar in forensic psychiatry from Broadmoor Hospital and independently by a forensic mental health social worker. Both professionals will then produce independent reports, recommending that admission is offered or declined. The two Broadmoor reports, together with the original request for admission, are then submitted to the Broadmoor admission panel, which is a multidisciplinary group led by a consultant forensic psychiatrist. The group will then take a view on whether admission is offered or declined. The most common reason the group would decline admission is that the view of the panel is that the patient does not meet the security needs that require a high secure admission and could be managed at a medium secure level.
Independently, two post-membership doctors in forensic psychiatry (H.K.W. and M.S.) completed the DUNDRUM-1 triage security and DUNDRUM-2 triage urgency scales on all 204 referrals for admission during the period of the study. The doctors were supervised by a consultant forensic psychiatrist and author of the DUNDRUM tool (M.D.). The researchers completing the DUNDRUM tool had only the information that was available to the Broadmoor admission panel team. The researchers were masked to the outcome of, or discussions at the Broadmoor admission panel and did not attend the panel for any of the discussions during this period. The clinicians on the admission panel were masked to the research ratings. The research scores did not in any way have an impact on patient care or admission decision-making by the panel of clinicians.
Demographic data, data pertaining to diagnosis and scores on the DUNDRUM-1 triage security scale and the DUNDRUM-2 triage urgency scale were gathered. Subsequent to the completion of the ratings, data pertaining to the admission outcomes were also gathered via hospital medical records. Data were analysed using the statistical package for the social sciences (SPSS-21).
Setting
The study was set in Broadmoor High Secure Hospital, Berkshire, England. Broadmoor is one of three high security hospitals in England, providing care and treatment to mentally disordered offenders who meet criteria for detention under the Mental Health Act and pose a grave and immediate risk to the public because of ‘dangerous and violent criminal propensities’.20 The majority of mentally disordered offenders who require secure forensic hospital admissions in England are offered care and treatment in conditions of medium or low therapeutic security. Offering care and treatment at the lowest level of security appropriate to a patients’ needs, or ‘care in the least restrictive setting’ is a key principle of the UK NHS.21 A total of over 7000 secure mental health beds are available in England, however, the majority of these are at a low and medium secure level with only 795 of these beds being high. Broadmoor provides 200 high secure beds for London and the South of England, a catchment area population of over 24 million. Therefore, those patients admitted to high secure care who cannot be safely managed in lower levels of security comprise a very small, highly selected group.
Patients
All referrals from medium secure hospitals or prisons to Broadmoor Hospital, for potential admission, between 2015 and 2017 were included in the study. Cases were ascertained from the admissions panel register to ensure a whole cohort with no bias. All were men and over 18 years, as Broadmoor does not admit women or children. Those referred were included regardless of whether they were referred for admission to the mental illness or personality disorder pathways and regardless of the source of admission (prison, medium or low secure hospital or in rare cases court referrals).
Ethics
This study was approved as a service evaluation study by the Broadmoor Hospital Audit and Service evaluation committee. The aim of the study was to evaluate the functioning and decision-making of the hospital admissions panel. Patient data was anonymised and no patient-identifiable data used. The decision-making of the panel was observed only, the research did not in any way affect decision-making regarding admission or the care and treatment of any patient. Informed consent was therefore not sought from the individual patients referred to the hospital during the period of the study. The authors assert that this work complies with the Helsinki declaration of 1975, updated in 2008.
Statistical methods
We investigated the associations between scores on the DUNDRUM-1 triage security scale and need for admission as determined by (a) the opinion of the assessing high secure consultant psychiatrist, (b) the assessing high secure forensic social worker and (c) whether or not the patient was offered an admission bed by the high secure admission panel at Broadmoor Hospital. We compared the mean security needs between those referred from prison and medium secure hospital settings and also between the groups referred to the mental illness and personality disorder pathways. Mean scores on the DUNDRUM-1 security scale were compared using ANOVA, a 5% significance level was adopted for the analysis and SPSS version 21 was used throughout.
Results
A total of 204 individual referrals were received by Broadmoor Hospital during the 2-year period 2015–2017 inclusive. All were men and the referrals came from prison (n = 119) and medium secure hospitals (n = 85).
The mean age at time of referral was slightly higher among those referred from other hospitals; 34.22 years (s.d. = 9.5) from medium secure unit settings and 33.98 years (s.d. = 11.5) from prison settings, but this did not reach statistical significance (P = 0.154). Those referred to the personality disorder pathway (mean 36.89 years, s.d. = 10.7, n = 60) were older than those referred to the mental illness pathway (33.02 years, s.d. = 10.65, n = 144) (ANOVA F = 5.028, d.f. = 1, P = 0.026).
The majority of cases (54.1%) had an established diagnosis of schizophrenia at the time of referral, 15.1% had a diagnosis of personality disorder established and 26.8% were referred with an unclear diagnosis, the remainder being other diagnoses. Diagnostic uncertainty was more common among those referred from prison referrals (41.2%) compared with medium secure unit hospital referrals (7.1%), for obvious reasons.
We found that overall the group of patients offered admission to Broadmoor Hospital by the Broadmoor admission panel (n = 111) had significantly higher mean scores on the DUNDRUM-1 triage security scale than those declined (n = 93) by the panel (ANOVA F = 4.209, P = 0.042) (Table 1). We found that those referred from prison had higher security needs than those referred from medium secure forensic hospital settings, although the security needs of all those referred, including those declined for admission by the Broadmoor admission panel were very high.
Table 1 Mean DUNDRUM-1 triage security scores among those referred and admitted to Broadmoor High Secure Hospital
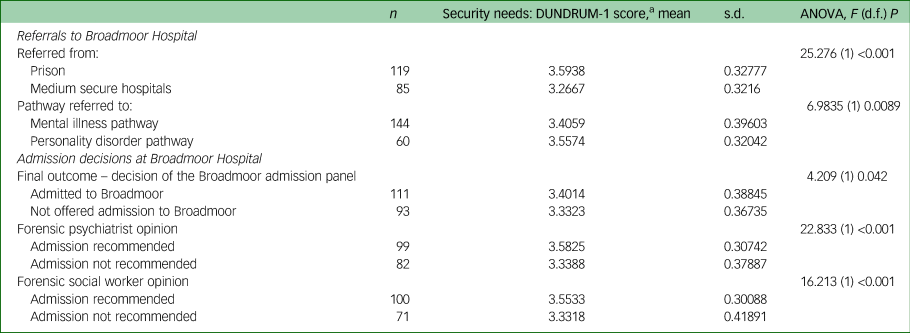
a. Average score across 9 triage security items, each item rated ‘0’ to ‘4’.
All referrals to Broadmoor, as mentioned above, are seen for independent pre-admission reports by a consultant forensic psychiatrist or specialist registrar in forensic psychiatry (under consultant supervision) and subsequently by a social worker from the high secure hospital. Those recommended for admission by the assessing forensic psychiatrist had higher mean DUNDRUM-1 security scores compared with the group not recommended for admission by the doctors (ANOVA F = 22.833, d.f. = 1, P < 0.001), and a similar finding was found in relation to the social worker pre-admission assessments (ANOVA F = 16.213, d.f. = 1, P < 0.001) (Table 1).
Comparison of referrals to the personality disorder and mental illness pathways
Although all referrals to Broadmoor Hospital had very high security needs as measured on the DUNDRUM-1 triage security scale, the security needs among those referred to the personality disorder pathway at Broadmoor were higher than the mean security needs scores of those referred to the mental illness pathway at Broadmoor (ANOVA F = 6.9835, d.f. = 1, P = 0.0089). An item-to-outcome analysis was completed for the DUNDRUM-1 security needs items. We found that on all but two of the items on the DUNDRUM-1 triage security scale, those referred to the personality disorder pathway had higher mean scores than those referred to the mental illness pathway (the exceptions being ‘seriousness of previous violence’ and ‘victim sensitivity and public confidence’). We found no significant difference in terms of urgency of need for admission between those referred to the personality disorder pathway and those referred to the mental illness pathway (ANOVA F = 0.304, d.f. = 1, P = 0.582).
Discussion
Triaging patients to the appropriate level of therapeutic security is one of the most important decisions for any forensic mental health service.Reference Flynn, O'Neill, McInerney and Kennedy9 The use of structured professional judgement instruments can assist this process as unstructured judgement is prone to error and inconsistencies. In this study we found the scores on the DUNDRUM tool were closely aligned to the decisions of both the Broadmoor admission panel and the assessing clinicians.Reference Flynn, O'Neill, McInerney and Kennedy9,Reference Flynn, O'Neill and Kennedy10,Reference Freestone, Bull, Brown, Boast, Blazey and Gilluley15 This demonstrated the strong clinical relevance of the tool. The DUNDRUM tool is designed to support clinical decision-making regarding triaging admissions, but it does not replace clinical decision-making.Reference Kennedy, O'Neill, Flynn, Gill and Davoren8 The aim of the triage tool is to improve the reliability and transparency of decision-making regarding the need for therapeutic security, to allow the hospital and clinicians to explain decisions to patients, commissioners and legal bodies when needed.Reference Kennedy, O'Neill, Flynn, Gill and Davoren8 It ensures that all the necessary factors are considered in the decision-making process, however, the final decision remains with the clinician.
This study demonstrated very high security needs among the group of patients referred for high secure care to Broadmoor Hospital, in keeping with the nature and purpose of high secure services in England. Previous studies using the DUNDRUM tool in other jurisdictions have demonstrated the security needs of referrals to and admissions into other services. We found the published security needs of referrals to a London medium secure service (The John Howard Centre, Hackney) were lower than those referred to Broadmoor, those admitted to Broadmoor and those declined for Broadmoor.Reference Freestone, Bull, Brown, Boast, Blazey and Gilluley15 The outcomes are unclear for the group whose security needs are not high enough to merit high security hospitals, but exceed those of medium secure units. This may represent a potential gap in service provision.
Comparing the security needs of those referred to and admitted to Broadmoor with admissions in other countries using previously published studies using the DUNDRUM-1 triage security scale, we found that the security needs of Broadmoor referrals were higher than those referred to forensic mental health services in Ireland,Reference Flynn, O'Neill, McInerney and Kennedy9,Reference Flynn, O'Neill and Kennedy10 the Netherlands TBS (Terbeschikkingstelling) service, which offers medium secure hospital admissions to those at the end of prison sentences who have mental disorder,Reference Eckert, Schel, Kennedy and Bulten22 Netherlands long-stay high secure service,Reference Eckert, Schel, Kennedy and Bulten22 Belgian forensic servicesReference Habets, Jeandarme and Kennedy17,Reference Jeandarme and Habets23,Reference Jeandarme, Habets and Kennedy24 and Australian forensic services.Reference Adams, Thomas, Mackinnon and Eggleton16 In fact, no study using the DUNDRUM-1 triage security tool published to date has found higher security needs among any hospital or prison group than the Broadmoor referrals. This is a strength of this methodology – using a reliable, internationally validated tool with strong psychometric properties can allow international comparisons of such groups.
Limitations
The main limitation of the study is that it is retrospective in nature. However, this methodology allowed a large number of referrals to be reviewed and rated by the researchers in a relatively timely manner. A whole cohort was assessed so that no bias was introduced. A second limitation is that the group only includes men, as Broadmoor only admits male patients. The study only included one of the three high security hospitals in England, and therefore the catchment area encompassed the South of England only. It is unclear if the patterns of very high security needs were specific to the catchment area covering the London Metropolitan area or would hold in the North and West of England. This question would merit a future study also.
Interpretation
Broadmoor Hospital offers care and treatment to a uniquely vulnerable group of patients with very high security needs. The patient group referred to the personality disorder pathway in the high secure hospital had particularly complex security needs, however, it remains unclear why that was the case and this would merit further research. Although the differences in mean scores between the patient groups may not appear large, the scores on the DUNDRUM tool are organised in units of meaningful change, representing the different levels of therapeutic security available in international forensic hospital settings, therefore the differences between the groups in terms of security needs are both statistically and clinically significant.
The very high security needs seen here among the Broadmoor group may in part explain the need for higher staff to patient ratio's and why one might expect a higher need for restrictive practices to prevent violence among the high security patient group, compared with the groups at medium and low therapeutic security. The use of any restrictive practice, for example seclusion or long-term seclusion, must always be as an absolute last resort to prevent serious and immediate violence. The greatest predictor of future violence is past violence.Reference Monaghan25 The DUNDRUM tool rates baseline security needs, such as seriousness of previous violence, violence not exclusive to the context of major mental illness and violence that is particularly complex for example with sadistic features or other unusual aspects.Reference Kennedy, O'Neill, Flynn, Gill and Davoren8 The finding that the group admitted to Broadmoor scored significantly higher on this tool, compared with medium or low secure patient groups, is in keeping with a group that are likely to present with complex challenging behaviour as in-patients.
Specialised therapeutically secure psychiatric services within high secure settings such as Broadmoor are an essential resource, given the significant differences seen between those admitted to Broadmoor and not admitted, and those admitted to mental illness and personality disorder services in this study. High secure hospitals are admitting a different group compared with medium and low secure hospitals. This may, at least in part explain the need for greater levels of physical, procedural and most importantly relational security seen in the English high secure hospital services. These results are likely to be generalisable to other high security hospitals in England and in other jurisdictions, and this may be an area of future collaborative research.
Data availability
Due to the uniquely sensitive nature of this data-set, access to data will only be provided on a strict case-by-case basis.
Acknowledgements
The authors would like to acknowledge the medical records department at Broadmoor Hospital for their support in completing this study.
Author contributions
M.D. designed the study and formulated the research question with C.C.R., H.K.W. and M.S. completed the DUNDRUM-triage tool ratings. M.D. and H.K.W. analysed the data. All contributed to the authorship of the paper.
Declaration of interest
None.
ICMJE forms are in the supplementary material, available online at https://doi.org/10.1192/bjo.2020.35.




eLetters
No eLetters have been published for this article.