Oral health is important for day-to-day functioning and plays a critical role in eating, smiling and talking.Reference Slade1 Conversely, poor oral health is detrimental to general health, self-esteem and quality of life.Reference Kisely2 People diagnosed with psychotic disorders experience worse oral health outcomes than the general population, including higher levels of decayed and missing teeth.Reference Mojtaba, Ulduz ZA, Amirhossein and Mehri3,Reference Kang, Wu, Aggarwal, Shiers, Doran and Palmier-Claus4 Psychotic disorders (e.g. schizophrenia, schizoaffective disorder) have a lifetime prevalence of 3%Reference Sullivan, Kounali, Cannon, David, Fletcher and Holmans5 and are characterised by experiences of hallucinations, delusions and difficulties concentrating or thinking.6 Psychosis commonly develops between late adolescence and early adulthood,7 which is important because research indicates that oral hygiene habits often decline in adolescence.Reference Taiminen8 The prevalence of edentulousness (complete loss of teeth) and periodontal disease are also significantly higher in people with experiences of psychosis.Reference Kang, Wu, Aggarwal, Shiers, Doran and Palmier-Claus4,Reference Kisely, Baghaie, Lalloo, Siskind and Johnson9,Reference Kisely, Quek, Pais, Lalloo, Johnson and Lawrence10 Conversely, rates of filled teeth are significantly lower,Reference Yang, Chen, He, Lu, Wang and Soares11 which may indicate reduced access to dental care and the need for more intrusive treatments, like teeth extraction. This increases demand in emergency dental treatment and places a significant financial burden on the healthcare system.Reference Joury, Kisely, Watt, Ahmed, Morris and Fortune12
Reasons for suboptimal oral health in people experiencing psychosis are likely complex and multifactorial. They may include individual influences, such as motivation to seek treatment,Reference Villadsen and Sørensen13 chronicity of mental health problemsReference Nielsen, Munk-Jørgensen, Skadhede and Correll14 and high-risk behavioursReference Kang, Palmier-Claus, Wu, Shiers, Larvin and Doran15 such as smoking. The prevalence of smoking in people with psychosis appears to be higher than the general population,Reference Cooper, Mancuso, Borland, Slade, Galletly and Castle16 and is a known factor in elevating the risk of all oral health problems in the general population.Reference Chaffee, Couch, Vora and Holliday17 Iatrogenic effects of psychiatric treatments such as medication may also play a role in the oral health disparity in people with psychosis.Reference Cockburn, Pradhan, Taing, Kisely and Ford18
The cost of dental services possibly acts as a barrier for people with experiences of psychosis. In the UK, exemptions may apply for low-income patients. However, the payment system is complex and may be hard for patients to navigate, which may reduce access.Reference Laverty and Harris19 To ensure success of advanced care and protect limited National Health Service (NHS) resources, UK dentists expect patients to have healthy gums and no underlying risk factors like high frequency of sugar intake, smoking or poor oral health self-care behaviours (e.g. regular flossing and tooth brushing).Reference Laverty and Harris19 However, the uptake of oral health self-care behaviours appear low in people with psychosis.Reference Turner, Berry, Aggarwal, Quinlivan, Villanueva and Palmier-Claus20 Therefore, this population may find it difficult to engage in key preventative behaviours that could not only reduce the need for emergency treatments,Reference Denis, Goueslard, Siu-Paredes, Amador, Rusch and Bertaud21 but also allow a restoration of function and aesthetics.
Study aims
The aim of this qualitative study was to interview people with psychosis and seek their perspective about the ways in which oral health and psychosis interact. By doing this, we sought to understand the complex relationship and the unique challenges this population face, to address unmet oral health needs. We aimed to capture the important voice of patients to explore what meaningful changes are needed to improve dental outcomes in people with psychosis. To our knowledge, this is the first qualitative study to explore the relationship between oral health and psychosis in a patient sample.
Method
Sample and recruitment
A pragmatic qualitative approachReference Cornish and Gillespie22 was utilised to ascertain knowledge about the relationship between psychosis and oral health, using semi-structured interviews. We aimed to recruit a sample large enough to develop a rich understanding of the research question.Reference Hennink, Kaiser and Marconi23 Clinical teams from two NHS Trusts in England referred patients meeting criteria for an ICD-10 or DSM-IV diagnosis of a psychotic disorder (e.g. schizophrenia, schizoaffective disorder), as diagnosed by the referring clinical service. We also include participants with first-episode psychosis as indicated by meeting the operational criteria for an Early Intervention for Psychosis Service. See Table 1 for full inclusion criteria.
Table 1 Criteria for inclusion

Ethics statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human participants were approved by the North-West – Greater Manchester East Research Ethics Committee (approval number 19/NW/0723). All participants provided informed consent to take part.
Data collection
The first author (E.T.) conducted face-to-face (n = 3) or telephone (n = 16; during the COVID-19 pandemic) interviews, following a topic guide developed with input from three people with lived experience of psychosis and one carer. Interviews ranged from 18 to 62 min (median: 31.22, interquartile range: 28–40) and were transcribed verbatim. Participants provided key demographic and clinical information before interview and completed the Oral Health Impact Profile-14 (OHIP-14)Reference Slade1 and the Oral Health SurveyReference Aggarwal, Javidi, Joughin, Crawford and Sharif24 to assess their oral health-related quality of life and knowledge of dental risk factors. The majority of the sample were recruited from a community mental health team. Therefore, the majority had chronic mental health difficulties with multiple in-patient admissions.
Analysis
The analysis process was both systematic and iterative, following guidance for reflexive thematic analysis outlined by Braun and Clarke.Reference Braun and Clarke25,Reference Braun and Clarke26 The lead author (E.T.) actively engaged with the data-set for familiarisation and completed line-by-line coding, which led to the development of preliminary themes. Authors L.Q. and V.A. coded a subsection of transcripts to provide other perspectives, and the research team developed and refined these themes during regular multidisciplinary discussions. Data was managed with NVivo 12 for Windows (QSR International Ply Limited, Denver, USA; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home).
Reflexivity statement
The first author (E.T.) was a trainee clinical psychologist with a Master's in Health Psychology and experience of clinical working with psychosis. E.T. engaged with the relevant research on dental literature before analysis, which informed deductive coding.Reference Fereday and Muir-Cochrane27 The data was collected through a psychological lens, given the first author's professional training. During the process of the initial interviews, the first author noted a tendency to communicate approval in the presence of good oral health routines, which may have made it difficult to disclose any difficulties faced. Given the potential for self-stigma and societal beliefs about good oral hygiene, efforts were taken to ensure that interview questions were not asked from a place of judgement, rather to explore individual perspectives on oral health and psychosis. The interviewer explained that she had no professional experience in dentistry and therefore was not adopting a critical stance when exploring oral hygiene and habits.
The research group comprised of two clinical psychologists (K.B. and J.P.-C.), a non-clinical qualitative researcher (L.Q.), a dentist (V.A.) and a carer representative (D.S.). This diversity in perspectives supported a broader interpretation of the data.
Results
Demographic and dentist visit information is reported in Table 2, alongside results from the OHIP-14 (Supplementary Fig. 1 available at https://doi.org/10.1192/bjo.2023.33). Findings from the Oral Health Survey indicated variable knowledge of oral health related risk factors, compared with a similar aged general population sample.Reference Aggarwal, Javidi, Joughin, Crawford and Sharif24 Study participants demonstrated a slightly better knowledge of risk factors pertaining to erosion (47% correct response rate compared with 31%) and caries (51% and 47%, respectively) than the general population sample. However, risk factor knowledge of periodontal disease was greatly reduced, with the study sample answering 30% of questions correctly, whereas 77% of the general population sample provided a correct response. Table 2 shows the percentage of participants experiencing difficulties in each oral health-related quality of life domain of the OHIP-14. A high proportion of the sample reported difficulties in all domains of the OHIP-14.
Table 2 Demographic information and dental data (n = 19)

Theme 1: psychosis creates barriers to good oral health
Table 3 includes further supporting quotes from the data. The first theme related to participants’ perception of the ways in which psychosis directly and indirectly affected oral health. Many participants reported feeling like poor oral health was an inevitable consequence of psychosis despite attempts to maintain a healthy routine.
Table 3 Additional supporting extracts for all themes
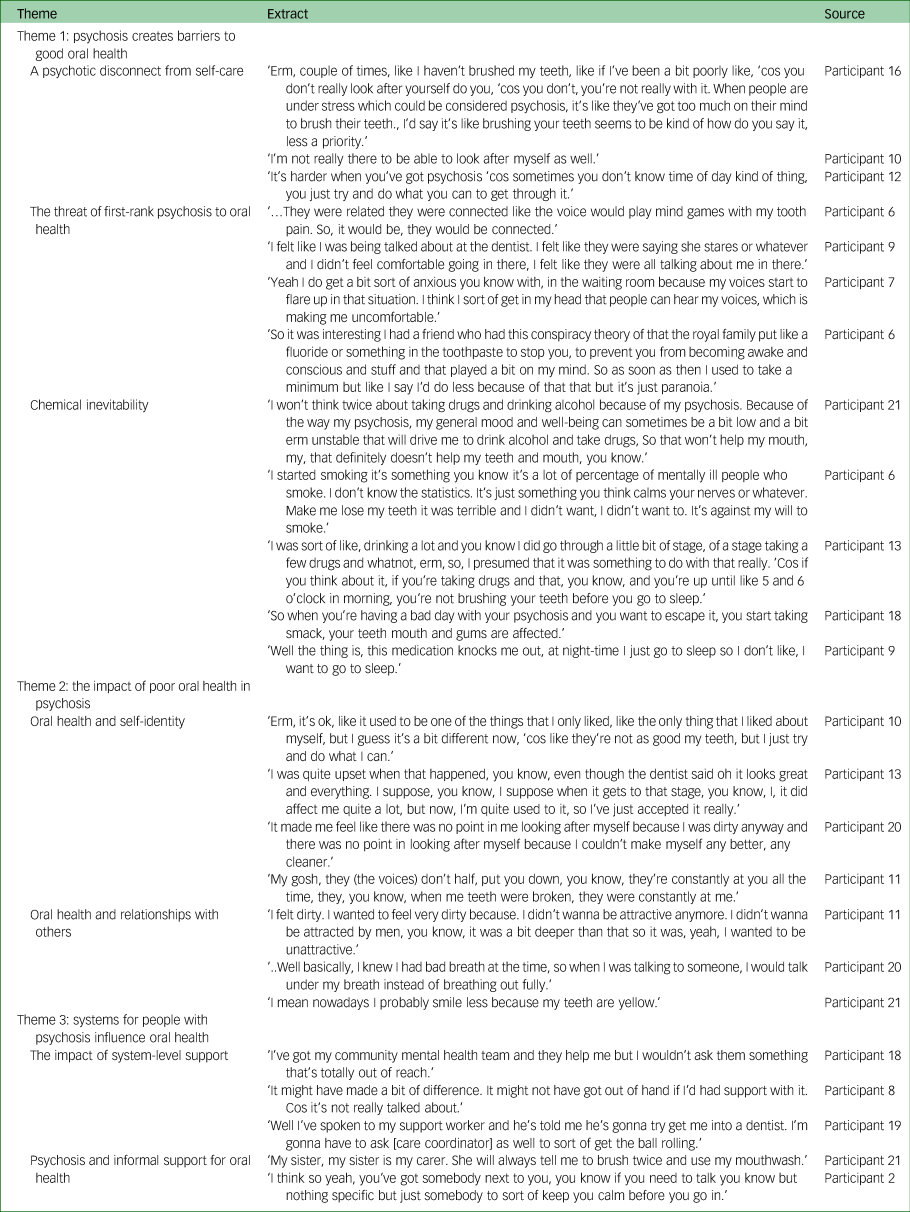
A psychotic disconnect from self-care
This subtheme refers to the all-encompassing nature of a psychotic episode that led to a disconnect with everyday activities, including oral health care. Participants talked about how psychosis brought about a temporary detached or dissociative state, which meant that self-care, like tooth brushing, felt distant and unobtainable. There was a complete preoccupation with their psychotic experiences, which made it impossible to maintain an oral health routine.
‘Yeah, it's like listening to the voices and the hallucinations and you're wrapped up in that world. That's a complete delusional fantasy and you're not in the real world to brush your teeth.’ Participant 19.
These feelings of disconnect from reality resulted in an inability to attend to oral health self-care behaviours (e.g. tooth brushing, flossing, dental visiting), which could trigger periods of overcompensating by overbrushing once acute psychosis subsided. Fluctuating patterns of behaviour suggested that people had an intrinsic sense of the importance of maintaining oral health, but that this was disrupted during periods of psychosis.
‘There's two sides to it really. You can either be, sort of, like obsessed about it and try and keep your mouth and your teeth as clean as possible, or when you're in a psychosis where time just goes without you realising, you know, hours and hours might pass, and you're not brushing your teeth.’ Participant 13.
The threat of first-rank psychosis to oral health
Participants talked about the direct impact that hallucinations and unusual beliefs had on their oral health, often operating through fear and anxiety. Such experiences prevented people taking care of their mouth, teeth and gums, and made them worried about accessing treatment. For example, threatening command hallucinations sometimes directly warned of possible negative consequences if a person engaged in dental treatments, which affected future dental attendance.
‘One of the voices said if you take your wisdom tooth out, we're gonna bring more voices in your head and then they took my wisdom tooth out and three more voices came.’ Participant 1.
Conversely, psychotic beliefs did not always impact adversely on dental health care. One participant expressed that their self-reported unusual beliefs, which appeared to be more grandiose in nature, enhanced their visits to the dentist. This suggests that it was also possible for psychotic symptoms to have a positive impact on oral health and potentially increase the likelihood of visiting the dentist.
‘I think because I'm important, they [dental staff] like seeing me and they're very polite to me and they like seeing me ‘cos I'm a bit of a VIP.’ Participant 15.
Chemical inevitability
This subtheme concerns the perceived impact that illicit and non-illicit substances have on oral health. People considered side-effects from antipsychotic medication to be damaging to oral health, and described finding it difficult to maintain a regular oral health routine because of the side-effects of tiredness and fatigue, with night-time routines being particularly challenging. Direct damage was thought to be caused by other side-effects, including dry mouth and cravings for sugary food. There was also some recognition that antipsychotic medication could positively affect oral health routines by minimising preoccupation with psychotic experiences.
‘I think it's a really bad side effect. You need saliva and that to keep your teeth in good order, good working order sort of thing, it's a really bad side effect.’ Participant 8.
The loss of routine and perceived direct damage from medication was mirrored by the perceived effects of other substances. This included illegal drugs, alcohol, caffeine and tobacco. Participants described these substances going ‘hand in hand’ (participant 18) with psychosis. They attributed their use of substances to escapism and distress management. There was some overlap with the subtheme ‘a psychotic disconnect from self-care’, as participants voiced a detachment from the real world when intoxicated, which affected their ability to attend to oral health self-care behaviours. Typically, participants recognised that substances negatively affected their oral health either by hindering their routine or directly causing damage. Despite this, participants stated that using illegal substances had often taken priority over self-care, because of the power of addiction and beliefs about substances reducing distress.
‘To be honest it was probably the same time when I was smoking crack, so probably drugs over dentist.’ Participant 4.
Theme 2: the impact of poor oral health in psychosis
The second theme relates to the ways in which participants’ thought that their oral health affected self-identity and their ability and desire to connect with others. The theme encompasses the impact that poor oral health has on psychological constructs that are central to mental health, such as self-esteem and sense of identity. Participants felt that social relationships were also affected by dental deterioration. Participants conceptualised the interplay between oral health and mental health in a destructive cycle. Poor mental health led to a worsening state of oral health that, in turn, further affected mental health.
Oral health and self-identity
This subtheme refers to the ways in which oral health affects peoples’ sense of self and identity, in the context of psychosis. Participants believed that the appearance of their mouth, teeth and gums were fundamental to their value as a person. Those who had experienced dental deterioration commonly described themselves as ‘dirty’. Existing concerns about the appearance of the oral cavity sometimes manifested as critical auditory hallucinations, which affected self-esteem.
‘The voices might call you a tramp or things like that and you know, threaten to knock out you know the rest of your teeth and things like that.’ Participant 19.
Overall, deterioration in oral health was an emotive topic for participants. The perceived loss of good oral health seemed to lead to a sense of loss in identity. It was as if the deterioration stripped away remaining positive attributes, such as their smile.
‘I've always had a big smile, you know. People used to comment that I had a nice smile, so it was upsetting.’ Participant 8.
Oral health and relationships with others
The cumulative impact of psychosis and poor oral health made social and romantic relationships challenging. People expressed feeling vulnerable and in danger from others because of their paranoia, and this was further exacerbated by their poor oral health.
‘It's like I say, when I'm going out and things like that as well because I'm paranoid anyway about going out just in case, I mean if I'm thinking of going out, you know, what if someone sees my teeth and wants to start trouble with me, they think I'm an easy target or something like that.’ Participant 19.
Fears of negative judgement from others about their oral health seemed to perpetuate social avoidance. This related to the subtheme ‘oral health and self-identity’, suggesting that people experienced a reduction in self-esteem because of deteriorating oral health, which affected the way they viewed themselves and how they expected others to perceive them.
To mitigate the effects of poor oral health in social situations, participants attempted to mask their oral health when smiling or talking to others, to avoid embarrassment or shame. This affected their ability to have authentic connections with others. Masking included hiding their teeth when smiling and talking to people under their breath to disguise halitosis (bad breath). Poor oral health was also conceptualised as a strategy to keep people away in the context of experiences of early trauma, suggesting that this can sometimes be an active process to protect the self from further danger.
‘I find it quite difficult to smile because I think me teeth are that bad, even though, no one can tell, erm, I know, you know, so, you know, I, sort of like maybe cover my mouth with my hand or, try and smile without actually opening my mouth.’ Participant 13.
Theme 3: systems for people with psychosis influence oral health
This theme relates to the ways in which the presence of a psychotic disorder can influence how formal and informal systems interact with oral health. The lack of prioritisation of oral health in some mental health services was juxtaposed with the holistic care provided by others. Informal support from family and friends was a central factor in maintaining good oral health in this population.
The impact of system-level support
This subtheme relates to the way in which the presence of a psychotic disorder can influence professional support systems. Participants talked about having support around them because of their psychosis, but that this support was designed to treat their mental health and that there was little consideration of wider physical health needs, including their oral health. In general, mental health professionals seldom asked about patients’ oral health because their psychotic experiences were considered to be the priority. This passivity of healthcare professionals in relation to dental health mirrored patient perceptions that poor oral health was inevitable and may have contributed to a lack of prioritisation of oral health behaviours.
‘So I guess in that sense, like they (mental health professionals) never, I don't think they ever think of that as a, sort of, thing that they need to address, like the mental health team.’ Participant 10.
A neglect of oral health needs was not always the case. Practical support from mental health teams to access the dentist (e.g. making the appointment or providing transportation) sometimes positively affected dental visits. More specialised psychological support to reduce dental fear also enabled access to the dentist by reducing psychological barriers. Support workers, nurses and psychological therapy staff provided oral health support to participants at times, which was warmly received. People who received tailored and holistic support spoke positively of their care team.
‘Me and [healthcare professional's name] done some work on it to like, to think about safe place when I'm in dentist chair and that's worked, that's been really helpful.’ Participant 12.
Psychosis and informal support for oral health
Support from family and friends in people with psychosis was instrumental in maintaining oral health. The presence of a key family member or trusted friend made it easier to attend dental appointments and provided support following treatment. Informal support networks advocated for better dental treatment for people with psychosis. However, potential difficulties in connecting with others when oral health was poor (as identified in the ‘oral health and relationships with others’ subtheme) may have affected the availability of this important source of support for some participants.
‘A friend, he's gone he's asked after my visit to do a better denture for me because they've done a bridge but they can't do it.’ Participant 2.
Participants recognised that sometimes intervention from close family or friends was needed, particularly in the form of reminders if self-care was low as a consequence of psychosis or associated difficulties (e.g. substance misuse). However, the heightened focus on tangible difficulties like oral health was sometimes perceived by participants as uncaring and neglectful of emotional needs.
‘Yeah, cos sometimes I need it but sometimes I want her to say what's wrong with you? Are you okay? But sometimes she's just like, you've not brushed your teeth.’ Participant 18.
Discussion
Main findings
This is the first qualitative study to explore patient perspectives on the perceived relationship between oral health and psychosis. Our analysis suggests that people with psychosis perceive a relationship between psychosis and oral health, whereby both factors affect each other to some degree. Symptoms and behaviours associated with psychosis inhibit oral health behaviours and cause direct damage to teeth and gums. Poor oral health can then disrupt self-identity and the ability to form relationships with others. The interplay between oral health and psychosis was conceptualised in this paper as a negative feedback loop, whereby poor mental health reduced oral health behaviours, leading to deteriorating oral health, which then negatively affected mental health. The presence of formal and informal support for dental needs was important in breaking this vicious cycle by increasing access to the dentist for dental treatment. In addition, informal networks provided everyday support, which increased the likelihood of participants performing key oral health self-care behaviours.
Comparison with wider literature
The current study in a small sample of people living with psychosis potentially elucidates the reasons for low uptake of oral health behaviours in people with psychosis.Reference Turner, Berry, Aggarwal, Quinlivan, Villanueva and Palmier-Claus20 This includes a sense of inevitability that people felt, resulting from a disconnection from reality, the fear caused by psychotic experiences, and the use of prescribed medication and illicit and non-illicit substances. Past research has suggested that feelings of detachment can negatively affect general functioning,Reference Černis, Freeman and Ehlers28 and the present study indicates that this may extend to oral healthcare. Our analysis also suggests that fear and anxiety caused by hallucinations and delusions may prevent people from engaging in oral hygiene practices, adding to the burden of these experiences. In the absence of active psychotic symptoms, participants reported finding it difficult to attend the dentist and perform oral health behaviours. Therefore, support may be required even when the individual is mentally more able to prioritise oral health.
Participants perceived substances to be closely associated with psychosis and recognised that these were contributors to poor oral health, which is consistent with the wider literature.Reference Gregg, Barrowclough and Haddock29 This is consistent with research indicating that lifestyle factors such as smoking can double the risk of periodontal disease.Reference Kang, Palmier-Claus, Wu, Shiers, Larvin and Doran15 A recent review suggested that antipsychotic medication affects functioning because it causes feelings of lethargy and reduced motivation,Reference Thompson, Stansfeld, Cooper, Morant, Crellin and Moncrieff30 which could affect self-care behaviours like tooth brushing. The present findings also highlight the impact of other medication side-effects such as xerostomia (dry mouth) and an increased desire for sugary foods, which are risk factors for dental caries.Reference Aggarwal, Javidi, Joughin, Crawford and Sharif24 A recent qualitative study also suggested parallels between the use of substances (illicit and non-illicit) and antipsychotic medication and its effect on oral health.Reference Denis, Siu-Paredes, Maitre, Amador and Rude31
Recent research has suggested that many people with psychosis experience appearance-related voice content, particularly around weight gain which can negatively affect self-esteem and lead to social withdrawal.Reference Waite, Langman, Mulhall, Glogowska, Hartmann-Boyce and Aveyard32,Reference Waite, Diamond, Collett, Chadwick, Bold and Teale33 This is supported by our data, as participants disclosed auditory hallucinations that focused on the health of their mouth, teeth and gums, and often contributed to social distancing.
The current study found formal and informal support systems to be an integral factor in maintaining oral health. Previous findings have indicated that carers often bridge the gaps in support for patients with psychosis.Reference Onwumere, Howes, Shiers and Gaughran34 Our analysis points to the value of informal support networks for people with psychosis and comorbid with dental health needs. However, some participants did not have access to this type of support. The data also showed that the level of support provided by mental health teams is inconsistent. Some services did not routinely prioritise needs that were not within the mental health remit. A move toward more holistic care in mental health services has sometimes been endorsed,Reference Kisely2,Reference Moore, Shiers, Daly, Mitchell and Gaughran35 and advances have been made to incorporate physical health needs into mental healthcare.Reference Firth, Siddiqi, Koyanagi, Siskind, Rosenbaum and Galletly36
Strengths and limitations
In terms of strengths, the study involved exploring perspectives in people with lived experience of psychosis, which provides personal context to the issue of psychosis and oral health. Having an interdisciplinary team enabled trustworthiness and triangulation of the analysis.Reference Peters37 The research had strong patient and public involvement, resulting in a coproduced topic guide that was acceptable to participants and produced a wealth of relevant information. There are also limitations to the research, which include a lack of diversity in a sample that was predominantly White British. The study ran during the UK COVID-19 lockdown period, which restricted recruitment and made it difficult to adhere to the a priori sampling frame. Furthermore, only a minority of participants were experiencing early first-episode psychosis, and there is a need to explore this relationship between psychosis and oral health across a broader continuum of recovery. The study did, however, recruit from two NHS Trusts, which widened the geographical spread of the sample.
Clinical implications
The findings have key implications for mental health services. The analysis suggests that the maintenance of oral health care may be contingent on mental wellness. Professional and informal support systems may be central to supporting patients’ mental health, enabling access to dental treatment and promoting good oral hygiene behaviours through practical and emotional support. Mental health teams can provide valuable support to patients with co-occurring dental and mental health needs. Our analysis indicates that consideration should be given to the iatrogenic effects of antipsychotic medication, which have relevance to oral health. This could include informed and collaborative decision-making about the potential impact of medication side-effects on people's teeth and gums (e.g. xerostomia/dry mouth). Services could support patients to discuss prescribed medication with their dentist, to ensure that relevant advice and guidance is provided by dental professionals to mitigate possible side-effects. It is well-documented that this population commonly engage in high-risk behaviours such as illicit drug, tobacco and alcohol use.Reference Kisely, Quek, Pais, Lalloo, Johnson and Lawrence10 Modifiable behaviours like smoking should be targets for intervention.Reference Kang, Palmier-Claus, Wu, Shiers, Larvin and Doran15 However, the current results indicate that these are often used as a form of distress management, and therefore it is prudent that mental health and dental professionals use a non-judgemental approach (e.g. motivational interviewing) to explore the function and any resistance to reducing these behaviours, despite the negative impact on their oral health.
Our analysis suggests a negative feedback loop between oral and mental health. Interventions should target the avoidance of oral health behaviours (e.g. visiting the dentist, tooth brushing, flossing) to break negative and perpetuating cycles of behaviour. A recent consensus statement38 has advocated that poor oral health should not be an inevitable consequence of severe mental illness, and has set targets for addressing current inequalities. In line with the present study findings, one of the targets is to ensure that training is provided to relevant professionals (e.g. dental and mental healthcare workers) to facilitate understanding and management of oral health difficulties in people with experiences of psychosis. Our data indicate that practical support from mental health teams and informal networks can help to facilitate access to dental care and treatment (e.g. support to book dental appointments, transportation, prompting patients to bring a supportive friend or family member if this is helpful). Therefore, such practical support must be encouraged to promote timely dental care. Based on the current findings, specific interventions may include formulating the origins of avoidance, utilising motivational strategies to improve adherence to oral health routines, and psychological strategies to reduce dental anxiety. There is also a need for services to foster hope and promote optimism for change.
In conclusion, patients perceived a bidirectional relationship between psychosis and oral health. Psychosis affected people's ability to attend to oral health needs and difficulties with oral health then perpetuated worsening mental health. Mental health services and informal support networks play a key role in supporting oral health needs and facilitating access to dental treatment. People experiencing psychosis often viewed poor oral health as an inevitable consequence of their situation. However, oral health problems are preventable and treatable. Clinical services must do more to break the vicious cycle between oral health and psychosis.
Supplementary material
Supplementary material is available online at https://doi.org/10.1192/bjo.2023.33
Data availability
The data that support the findings of this study are available on request from the corresponding author, E.T. The data are not publicly available due to restrictions to protect the confidentiality of research participants.
Acknowledgements
The authors would like to thank the experts by experience who contributed to development of the study.
Author contributions
All authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors. All authors were involved in designing the study. L.Q. provided guidance on the qualitative methodology. E.T. conducted the interviews. All authors were involved in the analysis and findings were refined with E.T., J.P.-C. and K.B. The manuscript was written by E.T. All authors contributed to the preparation of the final manuscript.
Funding
This study was completed as a part of a doctoral thesis and was not funded.
Declaration of interest
D.S. is an expert advisor to the National Institute for Health and Care Excellence (NICE) Centre for Guidelines; the views expressed are the authors, and are not those of the NICE.







eLetters
No eLetters have been published for this article.