Bicuspid aortic valve is the most common form of congenital heart disease (CHD), with an estimated prevalence between 0.5% and 1.4% and a significant burden of disease. Reference Roberts1–Reference Vedel, Rode and Bundgaard6 Aberrations in aortic valve morphogenesis are poorly understood and have been theorised to include abnormalities in genetics, cell migration, and/or fetal blood flow. Reference Siu and Silversides5,Reference Mordi and Tzemos7 The result is a valve composed typically of two unevenly sized leaflets, the larger of which has a central raphe from commissural fusion. Reference Siu and Silversides5,Reference Mordi and Tzemos7 Less commonly, a pure bicuspid valve has two equally sized leaflets and no raphe. Reference Siu and Silversides5,Reference Verma and Siu8
Bicuspid aortic valve without significant stenosis or regurgitation may go unrecognised for decades, but early diagnosis is important to enable patients and families to prepare for lifelong cardiac care. Associated anomalies and complications, which may be detected earlier if a diagnosis of bicuspid aortic valve is known, include aortic coarctation, thoracic aortic dilation, aortic dissection, and endocarditis. Reference Siu and Silversides5,Reference Mordi and Tzemos7,Reference Kiyota, Della Corte and Montiero Vieira9,10 In addition, the presence of bicuspid aortic valve may prompt genetic testing and encourage family screening. Reference Mordi and Tzemos7,Reference Kerstjens-Frederikse, Du Marchie Sarvaas and Ruiter11
A prenatal diagnosis of bicuspid aortic valve is possible, although technical limitations may preclude visualisation of individual aortic valve leaflets in the fetus. Reference Paladini, Russo and Vassallo12 Even if leaflets are inadequately visualised, associated ultrasound findings such as thoracic aortic dilation may raise the index of suspicion of the obstetrician or fetal cardiologist. Reference Vedel, Rode and Bundgaard6,Reference Dumitrascu-Biris, Zidere and Vigneswaran13 As thoracic aortic dilation tends to progress over time and may not yet be present in a fetus, a relatively larger aorta compared to aortic valve annulus size may suggest pathology. Other aortic valve features such as leaflet “doming” are associated with bicuspid aortic valve in adults, Reference Fowles, Martin, Abrams, Schapira, French and Popp14 but have not been assessed by fetal echocardiography.
We hypothesised that in fetuses without complex CHD, certain echocardiographic findings would be associated with a postnatally confirmed bicuspid aortic valve. These include larger ratios of the aortic root, aortic sinotubular junction, ascending aorta, and transverse aorta to the size of the aortic valve annulus, as well as qualitative leaflet features such as doming and thickening.
Materials and methods
This study included fetal echocardiograms performed between June 2011 and January 2020 in the Cohen Children’s Medical Center – Northwell Health system, where over 4000 fetal echocardiograms are performed each year. Cases were initially identified by searching for keywords “bicuspid aortic valve” in a transthoracic echocardiogram database. Complex CHDs such as hypoplastic left heart syndrome, atrioventricular canal defects, transposition of the great arteries, and double outlet right ventricle were excluded, but simple lesions such as ventricular septal defects and aortic coarctation were included. Cases were examined to determine if a fetal echocardiogram had been previously performed, and those were included in the study. Controls were identified by searching the transthoracic echocardiogram database for patients with normal cardiac anatomy and aortic valve morphology, on whom a fetal echocardiogram had been previously performed. Included controls were those that could be matched with a case by gestational age (within 2 weeks) at the time of the fetal echocardiogram.
Fetal echocardiograms were independently reviewed by two investigators (DH and MG), blinded to the echocardiogram results and subject status as case or control. Measurements performed as per standard guidelines included dimensions of the fetal aortic valve annulus, aortic root, and sinotubular junction from a standard transverse left ventricular outflow tract view, as well as the ascending aorta (at the level of the right pulmonary artery) and distal transverse aorta (between the left common carotid and left subclavian arteries) from a sagittal aortic arch view. Gestational age-based z-scores were calculated using the Boston Children’s Hospital z-score calculator. 15 An assessment of aortic valve appearance, including the number of leaflets as well as the presence of doming and thickened leaflets, was performed. “Doming” was defined as a relatively narrowed distance between aortic valve leaflet tips in systole, rather than leaflets opening flush against the aortic wall. Given the use of these unvalidated, qualitative descriptions of aortic valve appearance, interobserver agreement analysis for these values was performed on the first 20 subjects. For the quantitative fetal cardiac dimensions, intraobserver and interobserver variability has been previously reported at 1.7–3.0% and 1.7–7.0%, respectively. Reference Firpo, Hoffman and Silverman16
Descriptive statistics were reported for each variable stratified by group (bicuspid aortic valve versus normal control). Continuous variables were reported as medians and interquartile ranges (25th–75th percentile) for each group and for differences between matched pairs. Categorical variables were reported as frequencies and percentages. Wilcoxon signed rank tests were used for continuous variables to examine differences between cases and controls. Mean values obtained from the observers were analysed as continuous variables. For categorical variables, exact McNemar’s tests were used to investigate differences in marginal proportions in cases compared with controls.
Subgroup analysis was performed on the matched pairs of cases without significant additional defects that increase suspicion of aortic valve pathology. In this subgroup, cases with perimembranous ventricular septal defects, aortic valve annular or aortic arch hypoplasia (defined as a reported z-score ≤ -2.0), or aortic coarctation were excluded. A p-value < 0.05 was considered statistically significant. As this study was exploratory, no adjustments for multiple testing were used in assessing significance. All analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
We identified a total of 56 subjects with both a postnatally confirmed bicuspid aortic valve and a prior fetal echocardiogram available for review. Twenty-nine subjects were excluded for associated complex CHD, leaving 27 cases matched with 27 normal controls. Demographic and clinical characteristics at the time of the fetal echocardiogram are presented in Table 1. Estimated fetal weight percentile, as measured on obstetrical scan within 3 weeks of the fetal echocardiogram, was significantly lower in cases compared to controls. Of note, in the subgroup without significant associated CHD, the smaller estimated fetal weight percentile in cases approached but no longer reached statistical significance (median 38.0% [33.0–54.0] in cases versus 51% [47.3–58.5] in controls, p = 0.058).
Table 1. Fetal demographic and clinical characteristics.

Data presented as median (interquartile range) and n (%).
a Non-congenital cardiac findings included isolated premature atrial contractions, pericardial effusion, and echogenic foci.
b Other indications included multiple gestation, limited views on obstetrical ultrasound, and maternal medication use.
c Excluded in subgroup analysis. CHD = congenital heart disease; VSD = ventricular septal defect; SCV = superior caval vein.
The most common indication for fetal echocardiogram in cases was suspected CHD on obstetrical ultrasound. Only one of the 27 cases (3.7%) had a diagnosis of bicuspid aortic valve mentioned in the fetal echocardiogram report. Fifteen cases (55.6%) with postnatally confirmed bicuspid aortic valve had no congenital cardiac anomalies reported on the fetal echocardiogram, and 11 (40.7%) had simple associated cardiac lesions. Seven of these were abnormalities known to raise suspicion of aortic valve pathology, including perimembranous ventricular septal defects, aortic valve annular hypoplasia, and/or aortic arch hypoplasia/coarctation. Two additional subjects had small, insignificant muscular ventricular septal defects, and two had persistent left superior caval veins.
Aortic valve function was normal in most subjects. Only two cases were noted to have accelerated flow across the aortic valve, with peak systolic velocities of 1.0 and 1.5 m/sec by pulsed wave Doppler. All other subjects had peak systolic velocities that were normal for gestational age, and there was no significant difference in these velocities between cases and controls. Two cases had aortic valve insufficiency (one trivial, one mild). The fetus with mild insufficiency was the one with bicuspid aortic valve diagnosed prenatally, and there were no other cardiac anomalies in this fetus.
Indications for postnatal transthoracic echocardiography in cases included follow-up of prenatally diagnosed CHD (n = 11), re-evaluation of inadequately visualised structures on the fetal echocardiogram (n = 5), heart murmurs (n = 4), follow-up of non-congenital prenatal cardiac concerns such as a trivial pericardial effusion or premature atrial contractions (n = 3), family history of CHD (n = 2), and genetic or non-cardiac anomalies (n = 2). Postnatally, the majority (n = 22, 81.5%) of cases were confirmed to have a tricommissural but functionally bicuspid aortic valve, with fusion between the right and left coronary leaflets (n = 17, 63.0%) or the right and noncoronary leaflets (n = 5, 18.5%). Five cases (18.5%) had a “pure” bicuspid aortic valve, with no raphe of commissural fusion. No cases had aortic valve stenosis on the first postnatal echocardiogram, including the two with mildly accelerated aortic valve flow prenatally. Five cases had trivial aortic valve insufficiency on the first postnatal echocardiogram, including both cases with prenatal regurgitation. Genetic abnormalities of cases included Turner (n = 2), Beckwith–Wiedemann (n = 1), and Down (n = 1) syndromes, and one complex chromosomal translocation.
Average fetal aortic z-scores and aortic measurement ratios are presented in Table 2. Compared to controls, fetuses with bicuspid aortic valve had significantly smaller median z-scores of the aortic annulus and root. Only one case had aortic root dilation (z-score 3.03), and in this case aortic valve leaflets were also noted to be doming. Overall distributions of ascending and transverse aortic z-scores were not significantly different between groups, but three cases had ascending aortic dilation (z-scores 2.25–2.41). All cases with ascending aortic dilation were also noted to have thickened and doming leaflets. Fetuses with bicuspid aortic valve had significantly larger ratios of root to annulus, sinotubular junction to annulus, ascending aorta to annulus, and transverse aorta to annulus (Fig 1).

Figure 1. Transverse left ventricular outflow tract and sagittal aortic arch views demonstrate aortic annular and ascending aortic dimensions in a normal control (a and b) and an isolated bicuspid aortic valve case without aortic coarctation (c and d). The ratio between the ascending aorta (AAo) and aortic annulus (*) is notably higher in the subject with a bicuspid aortic valve (ratio = 1.74) compared to the control (ratio = 1.12).
Table 2. Fetal echocardiogram results.
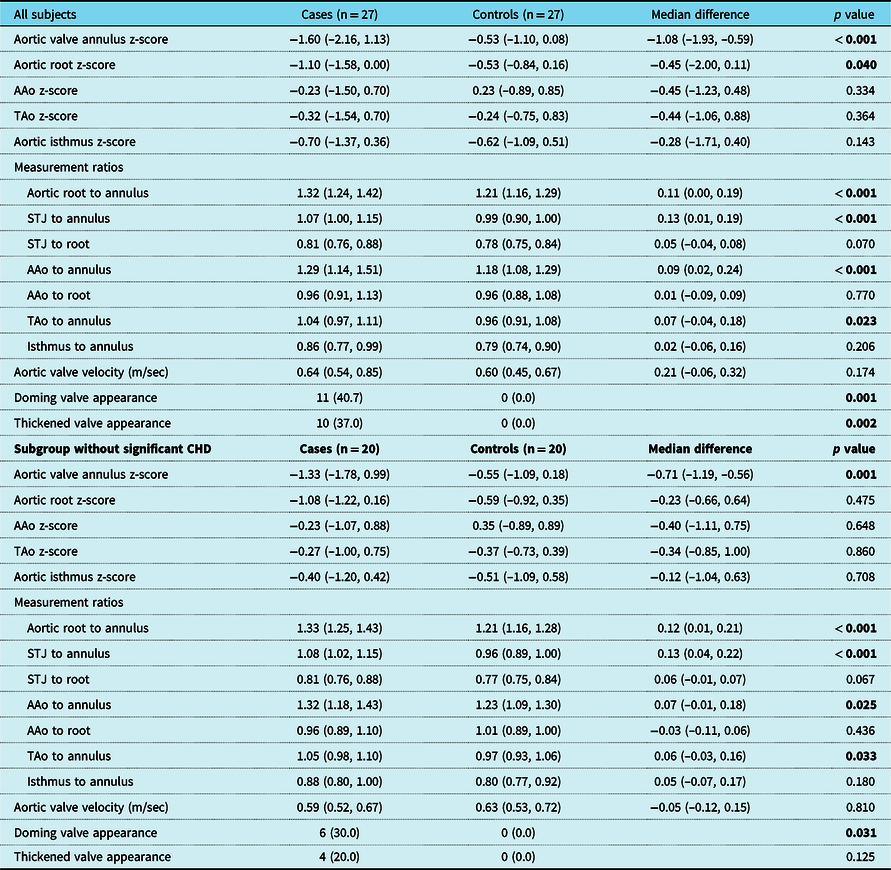
Data presented as median (interquartile range) and n (%). Results obtained by Wilcoxon signed rank tests (continuous variables) or exact McNemar’s tests (categorical variables). AAo = ascending aorta; STJ = sinotubular junction; TAo = transverse aorta.
The qualitative descriptions of aortic valve leaflets differed significantly between groups, with doming and thickened leaflets (Fig 2) found only in cases and not in controls. Leaflet thickening and doming were often noted together, with 8 of the 13 cases (61.5%) with one feature also having the other. These descriptive abnormalities were noted more commonly in the seven cases with significant associated CHD (85.7% thickened, 71.4% doming) than in those cases without (20.0% thickened, 30.0% doming). Only 1 case (3.7%) was deemed to have sufficient visualisation to definitively quantify the number of valve leaflets; this was the sole subject whose fetal echocardiogram report had remarked on a bicuspid aortic valve.

Figure 2. Transverse left ventricular outflow tract view demonstrates the qualitative appearance of aortic valve leaflets (*) in a normal control (a), systolic “doming” of a bicuspid aortic valve case (b), and thickening of a bicuspid aortic valve case (c).
In the subgroup refined to minimise the risk of investigator bias in fetal echocardiogram interpretation, the seven cases with significant additional defects that increase suspicion of aortic valve pathology were removed. Only one of the removed subjects had a genetic abnormality (Turner syndrome and severe aortic arch hypoplasia with coarctation). In this subgroup (n = 20), aortic valve pathology had only been mentioned in the fetal echocardiogram report of one subject (the case with a definitive fetal diagnosis of bicuspid aortic valve). Subgroup cases no longer had smaller aortic roots than controls, but continued to demonstrate smaller aortic annulus z-scores and larger ratios of root to annulus, sinotubular junction to annulus, ascending aorta to annulus, and transverse aorta to annulus. Leaflet doming remained significantly associated with bicuspid aortic valve.
Interobserver variability analysis revealed perfect agreement between observers in the qualitative assessment of valve appearance, with 100% agreement for both leaflet thickening and doming.
Discussion
Early diagnosis of bicuspid aortic valve prepares patients for complications that occur most commonly in adulthood. Reference Kiyota, Della Corte and Montiero Vieira9,10,Reference Michelena, Desjardins and Avierinos17 When diagnosis is made as early as the prenatal period, it can be of added benefit by prompting testing for genetic conditions and non-cardiac congenital anomalies. Reference Kerstjens-Frederikse, Du Marchie Sarvaas and Ruiter11,Reference Niaz, Fernandes, Sanders, Michelena and Hagler18 It may also encourage family screening, as first-degree relatives of non-syndromic patients with bicuspid aortic valve have an increased risk of CHD. Reference Kerstjens-Frederikse, Du Marchie Sarvaas and Ruiter11 However, fetal echocardiographic visualisation of aortic valve morphology is challenging, and even in ideal imaging conditions the raphe resulting from commissural fusion may make a bicuspid aortic valve appear trileaflet. Reference Mordi and Tzemos7
Prenatal bicuspid aortic valve diagnosis may also be important because of its relationship to aortic coarctation, one of the most frequently missed critical CHDs. Reference Contro, Cattani and Balducci19,Reference Garne, Stoll and Clementi20,Reference Niaz, Poterucha and Johnson21 While the increased incidence of bicuspid aortic valve in patients with coarctation is well-described, conflicting data exist regarding the risk of coarctation in those with bicuspid aortic valve. Reference Familiari, Morlando and Khalil22,Reference Anuwutnavin, Satou, Chang, DeVore, Abuel and Sklansky23 In our study, it was not the prenatal suspicion of bicuspid aortic valve that led to the four diagnoses of coarctation, but rather, it was fetal aortic dimensions or associated CHD.
In studies explicitly aimed at prenatal aortic leaflet visualisation, diagnosis of bicuspid aortic valve can be made reliably. Reference Paladini, Russo and Vassallo12 Paladini et al. showed that image quality was adequate to assess aortic valve morphology in approximately 85% of fetuses with and without CHD, with 96% of these receiving an accurate assessment. Reference Paladini, Russo and Vassallo12 However in studies not specifically designed to evaluate diagnostic accuracy, prenatal detection is much less common. In 8,371 fetuses without other CHD, none of the 55 with postnatally confirmed bicuspid aortic valve had the diagnosis made prenatally. Reference Vedel, Rode and Bundgaard6 As suggested by the low diagnosis rate in our cohort, clear aortic valve visualisation is not always possible but associated findings may raise the clinician’s index of suspicion enough to plan for postnatal evaluation.
A useful marker of bicuspid aortic valve may be the strongly associated thoracic aortic dilation (“bicuspid aortic valve aortopathy”). Patterns of aortopathy (occurring even in the absence of aortic stenosis or regurgitation) include dilation of the ascending aortic convexity with or without aortic root or transverse aortic involvement, and more rarely isolated root dilation. Reference Verma and Siu8 Aortopathy may begin prenatally and is progressive. Reference Verma and Siu8,10,Reference Dumitrascu-Biris, Zidere and Vigneswaran13,Reference Warren, Boyd, OʼConnell and Dodds24 Bicuspid aortic valve has been found in 37.5% of fetuses with ascending aortic dilation, Reference Dumitrascu-Biris, Zidere and Vigneswaran13 and larger root and ascending aortic dimensions have been noted in newborns with bicuspid valves. Reference Sillesen, Vøgg, Pihl and etal4 Interestingly, few of our cases had actual dilation of the aortic root and ascending aorta, but notably greater ratios of these dimensions to aortic annulus size compared to controls. Thus, smaller aortic annulus sizes in cases were not met with proportionally smaller aortic dimensions. These ratios obviate the need to consider the size of the fetus, a potential strength of these values.
Our finding of smaller aortic annulus in bicuspid aortic valve differs from the study by Vedel et al., in which an unselected cohort of fetuses with isolated bicuspid aortic valve had larger annulus sizes compared to controls. Reference Vedel, Rode and Bundgaard6 In our study, smaller estimated fetal weight in cases could account for this finding. Finally, qualitative descriptions of thickening and doming were associated with bicuspid aortic valve when all subjects were compared to controls, and doming remained significant in the subgroup without significant CHD. These often subtle findings should be considered in the prenatal assessment of aortic valves even when leaflet morphology cannot be readily distinguished.
Limitations include our study’s retrospective design and small sample size (which was not based on formal power calculations and may have benefited from a larger control cohort). Limitations also include the inherent bias of blinded investigators (who were aware of the study purpose and likely had heightened suspicion for bicuspid aortic valve), and the difficulty generalising our subjects to a population with less suspicion for CHD. We did not perform comparisons between aortic dimensions and other cardiac measurements, which may provide interesting additional information. Finally, the clinical utility of these ratios requires further investigation, as differences between groups were small.
In conclusion, bicuspid aortic valve should be suspected on fetal echocardiogram when leaflet doming and/or thickening are noted, or when increased ratios of aortic dimensions to valve annulus suggest a size discrepancy. Though prenatal diagnosis of bicuspid aortic valve can be challenging when aortic valve cusps and commissures are inadequately visualised, the present study suggests additional findings that may increase suspicion of bicuspid aortic valve and prompt postnatal confirmation.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.
Ethical standards
All applicable institutional guidelines for clinical research were followed. This project was approved by the Northwell Health Institutional Review Board.
Social media synopsis
Despite the challenges of diagnosing bicuspid aortic valve prenatally, certain features of the valve and aorta on fetal echocardiogram may suggest the diagnosis.







