The first 3 years of life are very important in terms of child development, since during this period, the typical developmental milestones are of greatest interest to be able to intervene with therapies if required. Reference Dosman, Andrews and Goulden1,Reference Long and K.2 The physical activities of a newborn are important to give the impulse for activating neurons, which is the base for building a neuronal network in the brain. Reference Flügel und Wurzeln3 The more frequently and diversely these neurons are used, the better and faster the connection via synaptic junctions will be established. Reference Long and K.2 Therefore, physical activity is important for development, especially in the first year of life because during this time the brain is particularly malleable and easily changeable. Reference Goddard Blythe4 Some of the motor abilities that are not experienced during this age period are hard to recover or reinforce later. Reference Goddard Blythe4 Children with CHDs need open heart surgery precisely at this elementary developmental period. The procedure under sedation, with the use of cardiopulmonary bypass, the subsequent hospitalisation time, and further treatment in the hospital are in themselves an interruption of early childhood development. Especially in children with CHD, from newborns to infancy, numerous studies have shown impairments in the development of speech, motor skills, and cognitive function or executive function. Reference Latal5–Reference Ferentzi, Pfitzer, Rosenthal, Berger, Schmitt and Kramer12 Thanks to advances in paediatric cardiology, cardiac surgery, or catheter interventions, and aftercare during the last decades, mortality has dramatically decreased. Reference Kaltman, Burns and Pearson13–Reference Voss and Harris15 Today more than 95% of children with CHD reach adulthood in Western civilisation. Reference Mandalenakis, Giang and Eriksson16 This growing adult CHD population is often assumed to have impairments regarding their cognitive function and decreased health-related quality of life. Reference Kovacs, Bandyopadhyay and Grace17,Reference Perrotta, Saha and Zawadzki18 In particular, it seems reasonable to assume that cyanosis may have a potential impact on cognitive function as well as surgical or drug treatment into adulthood. To our best knowledge, less is known about neuromental health aspects in an ACHD population including all CHD diagnoses who underwent open heart surgery during childhood. The term neuromental health aspects serve as an overarching term that stands for a wide range of influencing factors, and, in the context of this work, it includes cognitive function and health-related quality of life. In this study, we investigated adults with congenital heart defect (ACHD) with all types of CHD after open heart surgery during their childhood regarding their cognitive function and health-related quality of life. We hypothesised that (I) the age at first surgery earlier or beyond the age of 3 years is associated with cognitive function as well as (II) associations of cyanosis duration, the number of surgeries, and catheter interventional treatments with cognitive function and Reference Franklin, Jacobs and Krogmann19 potential associations between cognitive function and health-related quality of life representing neuromental health aspects in ACHD.
Patients and methods
Study subjects
During 2018, seventy-eight ACHD patients (female n = 39 (50.0%); mean age at assessment 34.1 ± 12.9 years) with all types of CHD were routinely asked to complete intelligence quotient tests and fill in the Short Form 36 questionnaire during routine follow-up for this cross-sectional study. Inclusion criteria were legal age (>18 years), no interventional treatment or surgery during the past six months, and surgical treatment of the CHD; exclusion was catheter interventional treatment only in this analysis. Out of 100 ACHD patients, 2 patients were not interested and 4 reported time problems, 94 were willing to participate. Additionally, 16 patients were excluded due to they have had no surgery but catheter interventional repair. The severity class of CHD was categorised into simple, moderate, and complex based on the American College of Cardiology definition by Warnes et al. Reference Warnes, Williams and Bashore20 The ACHD were divided into two categories; firstly, patients with one or more open heart surgery between newborn time and 3 years of age, secondly patients who underwent open heart surgery after the age of 3 years. At this age, the highest density of synapses to be achieved in life is reached, which is established in further development or reduced if not used. Reference Goddard Blythe4 The term cyanosis duration was defined from the date of birth until definitive or palliative repair, additionally for still cyanotic ACHD patients from the date of birth until the date of the test, in the case of Eisenmenger syndrome from the date of diagnosis until the date of the test. All patients gave written informed consent to participate voluntarily and agreed to the anonymous publication of their data. The study was following the Declaration of Helsinki (revision 2013). Approval from the local ethics board was obtained (Project Number 350/18 S).
Cognitive function
The current Wechsler Adult Intelligence Scale-Fourth Edition Reference Wechsler21 represents the gold standard in the assessment of cognitive function in adolescents and adults from 16 to 90 years. Reference Hartman22 The current Wechsler Adult Intelligence Scale-Fourth Edition provides information about the intelligence quotient, once as the Full-Scale intelligence quotient with four specific domains of intelligence; verbal comprehension, perceptual reasoning, processing speed and working memory. The intelligence quotient scores are calculated out of 10 different core tests with different weights and adjusted for age by using the Wechsler Adult Intelligence Scale-Fourth Edition software. Cognitive impairment is defined as an achieved intelligence quotient that deviates negatively by more than one standard deviation from the norm (average intelligence quotient = 100, deviation-intelligence quotient = ± 1SD; intelligence quotient normal range = 85-115 intelligence quotient points). Reference Wechsler21
Additionally, the Wechsler Intelligence Scales for children are widely used in paediatric cardiology to identify impairments or changes in cognitive function Reference Newburger, Wypij and Bellinger6,Reference Marino, Lipkin and Newburger9,Reference Feldmann, Ullrich and Bataillard23,Reference Gaynor, Ittenbach and Gerdes24 and therefore provide good opportunities for comparisons. The globally established test battery of the Wechsler Adult Intelligence Scale-Fourth Edition was validated and updated in 2013 for the German normal population with a norming sample of 1664 participants. Reference Daseking and Petermann25
Health-related quality of life
The Medical Outcomes Study Questionnaire Short Form 36 Health Survey is based on patient self-report within the last 4 weeks and has been proven in various healthcare settings to assess or monitor health-related quality of life outcomes in adult patients. Reference Bullinger26 The Short Form 36 asks for information from patients on eight different dimensions of health-health-related quality of life (vitality, physical function, physical pain, general health perception, physical role function, emotional role function, social role function, and mental health). The questionnaire consists of Likert scale questions as well as dichotomous questions; scaled values from 0 to 100 (poor to best health) are calculated for each dimension. The German version was validated by Bullinger and Kirchberger Reference Bullinger and Kirchberger27 and was implemented in this study. Based on Ellert and Kurth 2013, the ACHD were assigned the sex and age-specific norm data of the German population of the Short Form 36 for comparison. Reference Ellert and Kurth28
Data analyses
Descriptive statistics were calculated in absolute and relative frequencies (%) for categorical variables, and means and standard deviation for numerical variables. After testing normal distribution using Kolmogorov-Smirnov test, Reference Jurgen Janssen and Laatz29 Student’s t-test was used for comparisons of means as well as paired Student’s t-test. Linear regression model, general linear model, and Pearson’s correlation were used to determine relationships between measurements and patient data.
All analyses were performed using the software SPSS V.27 (SPSS Inc., Chicago, Illinois, USA) or R software V. 3.3.1. Pirate plots were used for visualisation of the data which represent the mean, confidence interval, raw data, and density distribution. The level of statistical significance was determined as two-sided and with a p-value < 0.05.
Results
In total, the ACHD group is perfectly balanced in terms of sex but not in subgroups; the early operation/surgery group shows more male patients at 53.3% and the late operation/surgery group more females at 54.5%. The huge majority showed complex CHD followed by moderate CHD and the minority with simple CHD. Additionally, differences between the groups in terms of “Age at first surgery” or cyanosis duration were analysed (Table1).
Table 1. Anthropometric data and group characteristics
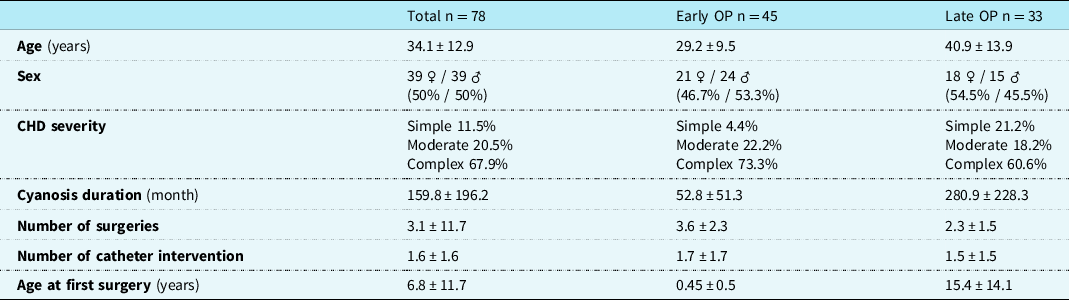
n = number; OP = operation/surgery.
The cognitive function of the whole ACHD cohort showed a mean of 97.1 ± 12.0 FSintelligence quotient. In a direct comparison between early operation/surgery and late operation/surgery groups, there was no significant difference found either in Full-Scale intelligence quotient or in subscales of the Wechsler Adult Intelligence Scale-Fourth Edition (Fig 1).

Figure 1. Student’s t-test for group comparison of IQ scores. IQ: Intelligence quotient; SD: standard deviation; level of significance p < 0.05.
The duration of cyanosis showed no significant association with all intelligence quotient scales in a linear regression model, but a significant difference was found in verbal comprehension by comparing patients with a cyanotic phase or never been cyanotic (p = 0.013). Furthermore, a general linear model showed no statistically significant association with CHD severity, the number of surgeries, and the number of catheter interventions for all intelligence quotient scales.
The early operation/surgery group showed significantly better results in the health-related quality of life domain of physical function and better results without statistical significance in most of the health-related quality of life domains (Table 2).
Table 2. HrQoL in total and in comparison between both groups with Student’s t-test
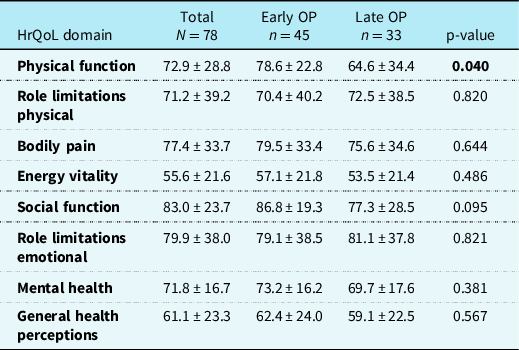
HrQoL = health-related quality of life; n = number; OP = operation/surgery.
Level of significance p < 0.05.
By comparing both groups with their sex and age-specific reference values, using a paired sample t-test significant impairments occurred except in the dimensions of bodily pain and mental health in both groups as well as social function in the early operation/surgery group and role limitations emotional in the late operation/surgery group (Fig. 2).
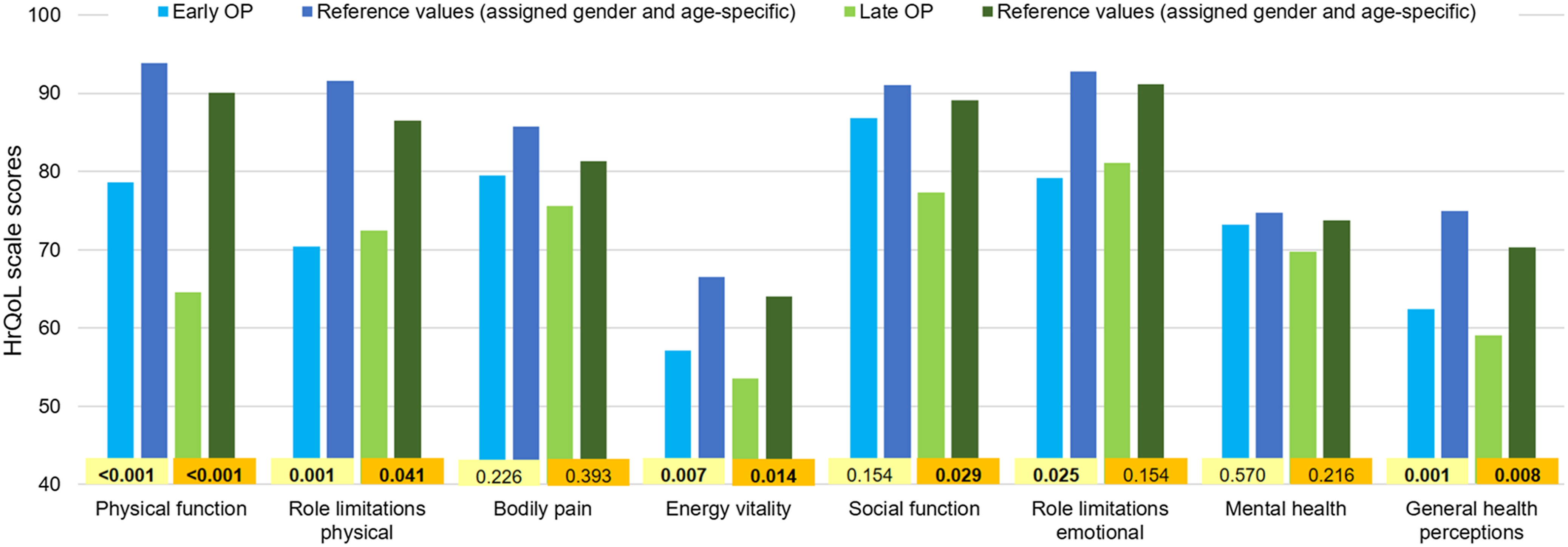
Figure 2. Group comparison with reference values of HrQoL by paired sample t-test. HrQoL: Health-related quality of life; OP: operation/surgery; level of significance p < 0.05.
The dimensions of “physical function” and “role limitations physical” significantly correlated with Full-Scale intelligence quotient in the early operation/surgery group but no correlation in the group of late operation/surgery (Table 3).
Table 3. Pearson’s correlation of FSIQ with all dimensions of HrQoL
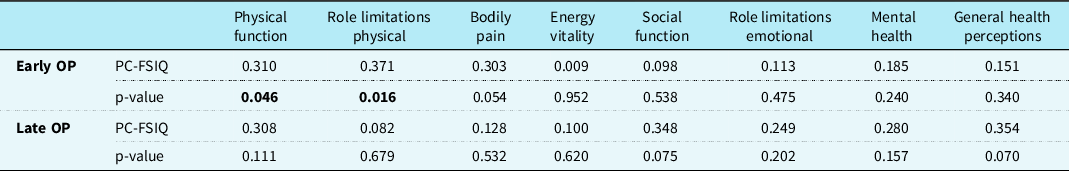
HrQoL = health-related quality of life; OP = operation/surgery; PC-FSIQ = Pearson’s correlation coefficient with Full-Scale intelligence quotient.
Level of significance p < 0.05.
Discussion
This study investigated neuromental health aspects in ACHD to gain an impression of cognitive function and health-related quality of life when patients after open heart surgery reached adulthood. Especially in older ACHD patients, the duration of cyanotic conditions was often longer, due to limited diagnostic possibilities and a later surgical correction. Thus, the question can be asked which constellation has the greater influence on neuromental health aspects, the first surgery in the vulnerable first three years of life, which are so crucial for development, or the duration of cyanosis. Based on this, the focus is on the two groups of early operation/surgery (first surgery between 0 and 3 years) and the group of late operation/surgery (first surgery beyond the age of 3 years).
The majority showed complex CHD followed by moderate than simple CHD; this is due to inclusion criteria. Based on the literature on children and adolescents with CHD, the included ACHD with predominantly complex CHD should therefore have reduced intelligence quotient scores. Reference Wray and Sensky30–Reference Cassidy, White, DeMaso, Newburger and Bellinger34 However, this was not the case, as a general linear model did not show significant associations of CHD severity with all domains of the Wechsler Adult Intelligence Scale-Fourth Edition which is contractionary with the results of children and adolescents. Reference Karsdorp, Everaerd, Kindt and Mulder33,Reference Kessler, Feldmann and Schlosser35–Reference Bolduc, Lambert, Ganeshamoorthy and Brossard-Racine37 Also, in the model, the number of surgeries and the number of catheter interventional treatments had no association with cognitive function. Kessler et al. 2020 described structural brain abnormalities (e.g. multifocal microhaemorrhages) which were significantly associated with complex CHD but they reported no association with the intelligence quotient outcomes using the Wechsler Adult Intelligence Scale-Fourth Edition short form Reference Kessler, Feldmann and Schlosser35 and in line with Schaefer et al. 2013 CHD complexity was not associated with neurodevelopmental outcome. Reference Schaefer, von Rhein and Knirsch38 That means they do not have a structural explanation only differences in the severity of CHD but as Kessler et al. 2020 mentioned in their limitations, 15 young ACHD cases have to be interpreted with caution. Reference Kessler, Feldmann and Schlosser35 Additionally, they reported an overall mean intelligence quotient of 98.51 ± 11.21 (n = 65) which is quite similar to our overall results of Full-Scale intelligence quotient 97.1 ± 12.0 (n = 78), the approximately ten years difference between these study populations can be left out of consideration, as age is taken into calculation in the evaluation of the Wechsler Adult Intelligence Scale-Fourth Edition from the outset. Reference Wechsler21
Regarding differences between early operation/surgery and late operation/surgery, both groups showed almost the same results from the Full-Scale intelligence quotient across all subscales. This means that despite the early interruption of development by open heart surgery, the consequences are not transferred to adult age in ACHD or there is some catch-up development over time. Interestingly separating both groups into had a period of cyanosis and never had been cyanotic significant differences in intelligence quotient scale verbal comprehension occurred with better results in never had been cyanotic. There was no association between intelligence quotient scores and cyanosis duration. Even though no significance was shown in the regression model, a slight tendency occurred in terms of processing speed with the longer ACHD suffer from cyanotic conditions the slower they are in processing speed (p = 0.053). Klouda et al. also reported on difficulties respectively impairments in information processing speed, psychomotor speed, and reaction time in ACHD with complex CHD Reference Klouda, Franklin, Saraf, Parekh and Schwartz39 but our study results must be compared cautiously since different measurements came to use. Overall, ACHD patients needed to be intensively included in larger studies to better understand brain-related changes since they, for example, are at higher risk for neurocognitive decline or early onset of dementia Reference Verrall, Blue and Loughran-Fowlds40–Reference de la Torre42 .
The other part of neuromental health aspects is health-related quality of life, besides pure functioning of the brain self-reported health-related quality of life is an important tool to get insights into the patient’s needs and worries and is quite easy to assess for follow-up of the patients by using Short Form 36 questionnaire, for example, in the waiting room. Our study population showed significantly different results in the Short Form 36 domain physical function in the direct comparison of early operation/surgery and late operation/surgery, in addition, the early operation/surgery group showed better results in most of the health-related quality of life domains but without significance. Since the early operation/surgery group is approximately 10 years younger this may explain the difference in physical function in this comparison. On the other hand, it is quite interesting that both operation/surgery groups did not show more differences as it is well known that the health-related quality of life decreases with increasing age. Reference Ellert and Kurth28 Therefore the next step of comparing both operation/surgery groups with their sex and age-specific reference value revealed alarming results. As Figure 2 shows, ACHD performed significantly reduced in all areas of the health-related quality of life except mental health and bodily pain. Additionally, the early operation/surgery had no significant difference with their reference in case social function, this may be related to being at this age social contacts or interactions are more in the focus of activities than in older ages. And in terms of late operation/surgery, there was no significant difference in role limitations emotional in comparison with their assigned reference. Interestingly, the Full-Scale intelligence quotient correlates significantly with the dimension of physical function and role limitations physical and this is in the early operation/surgery group only. It is known that more physical activity is associated with increased health-related quality of life even in ACHD patients. Reference Muller, Amberger and Berg43 The contradictory results on health-related quality of life and physical activity in ACHD cause-effect constructs have already been discussed and various explanatory models were used. Reference Muller, Hess and Hager44–Reference Fteropoulli, Stygall, Cullen, Deanfield and Newman46 In addition, it is known that a higher level of education is associated with better physical activity, Reference Kessler, Feldmann and Schlosser35 which in turn may explain the significant correlation of the Full-Scale intelligence quotient with the physical function and role limitations physical dimensions in our ACHD. Since the contradictory results on health-related quality of life in patients with CHD were previously discussed in terms of lack of general definition of health-related quality of life, different measurements as well as different settings even with different explanations like the sense of coherence, changing expectations, and awareness of illness during ageing, Reference Moons, Apers and Kovacs47–Reference Quarta, Muir and Pantazis50 it is in need to identify the health-related quality of life status and changes to get the chance for early intervention, interdisciplinary but primarily adapted to the specific needs of the patients. If ACHD already deviates from the sex and age-specific reference in many domains, an earlier approach needs to be found, such as through continuous questionnaire analysis over the years, to be able to react to changes appropriately and on time. Indeed, the findings on cognitive function combined with health-related quality of life in ACHD should be confirmed in larger cohorts with a multicentre approach to provide a clear impression of cognitive function and health-related quality of life in ACHD.
Conclusion
Concerning the hypothesis, we found no association of cognitive function with cyanosis duration, number of surgery or catheter interventions, CHD severity, and the timeframe of the first surgery in ACHD and greatly normal intelligence quotient scores. Health-related quality of life was weak in comparison with the reference, and there is a need to improve the well-being of our ACHD with structured programmes, including physical activity programmes. This growing ACHD population should be focused in order of their needs and problems medical ones on one hand and the other hand psychosocial matters.
Limitations
The significant differences between both groups must be interpreted with caution since both groups showed normal results within the frame of normative data. The evaluation of the detailed surgery data is not feasible as complete data are not available for all patients, since not all of the surgeries were performed at the same hospital or in the same country. Additionally, it is known that health-related quality of life as well as cognitive function can be related to social and social-economic factors, which were not assessed in this study.
Acknowledgements
We would like to sincerely thank all the study participants and also the clinic staff who made this work possible.
Author contributions
Conception and design: JR, NN, and MP
Administrative support: ROF and PE
Provision of study materials or patients: JR, NN, and MP
Collection and assembly of data: JR, NN, and MP
Data analysis and interpretation: JR
The first draft of the manuscript: JR
Final approval of manuscript: All authors
Ethics and dissemination
Approval from the local ethics board of the Technical University of Munich was obtained (Project Number 350/18 S). The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors
Competing interests
The authors have no conflicts of interest to declare.








