Antenatal detection of transposition of the great arteries has improved significantly over the past two decades. In Yorkshire, national audit data suggest around 75% of neonates with simple transposition of the great arteries are diagnosed antenatally. 1 This has improved significantly over the last decade with teaching and training to introduce outflow tract and three vessel views into routine screening. 1,2 Antenatal diagnosis of transposition of the great arteries confers a significant survival benefit, in addition to reduced rates of pre-operative mechanical ventilation, earlier balloon atrial septostomy, and earlier arterial switch operation. Reference Nagata, Glick and Lougheed3,Reference Bonnet, Coltri and Butera4
Circulatory changes after delivery can lead to rapid haemodynamic compromise due to parallel pulmonary and systemic circulations in transposition of the great arteries. Prompt infusion of prostaglandin to maintain ductal patency and balloon atrial septostomy to aid atrial mixing in this situation are often life-saving. Delivery out-of-hours may lead to delays due to reduced on-site staffing and non-resident senior cardiology support. Any delay in balloon atrial septostomy for neonates with a restrictive atrial septum (rASD) will lead to prolonged hypoxia and haemodynamic compromise, possibly resulting in poorer outcomes. The severity and duration of hypoxaemia has been previously linked to higher rates of pre-operative brain injury. Reference Petit, Rome and Wernovsky5 The fatigue of staff working out-of-hours also plays an important role. Reference Gaba and Howard6 One study of neonates undergoing balloon atrial septostomy out-of-hours demonstrated a higher procedure-related complication rate and overall mortality compared to in-hours balloon atrial septostomy. Reference Vimalesvaran, Ayis and Krasemann7
In this single-centre retrospective review, we aim to assess the impact of timing of delivery on outcomes for neonates with antenatally diagnosed simple transposition of the great arteries. We hypothesise that out-of-hours delivery can give rise to treatment delays and prolonged hypoxaemia, resulting in worse outcomes.
Methods
Design and subjects
We conducted a single-centre retrospective evaluation of the outcomes of all patients with simple transposition of the great arteries that were antenatally diagnosed between January 2015 and December 2020. Cases were identified from a local database of all fetal cardiac diagnoses at our tertiary cardiac centre in Yorkshire, United Kingdom. Antenatal diagnosis of transposition of the great arteries was made by an experienced consultant fetal cardiologist according to best practice guidance. 2,Reference Donofrio, Moon-Grady and Hornberger8 Follow-up fetal echocardiograms were performed for the duration of pregnancy to monitor for signs of blood flow restriction through the atrial septum, with the last echocardiogram at around 35 weeks gestation.
All cases identified through the database then underwent a further review of clinic letters and fetal echocardiogram reports to ensure they met the inclusion criteria. Patients were excluded if there was an additional cardiac diagnosis other than ventricular septal defect or coarctation of the aorta (CoA). All postnatal diagnoses of transposition of the great arteries during this period were excluded.
Included patients were categorised by time of delivery into in-hours (Monday to Friday 08:00–17:00 excluding weekends) and out-of-hours groups. All pregnancies were planned for delivery at the tertiary centre, with co-located tertiary neonatal unit and tertiary paediatric cardiology service. Induction of labour was recommended at 39-week gestation; however, no recommendations were made regarding mode of delivery. The decision to perform balloon atrial septostomy was made on a case-by-case basis by the responsible cardiologist and based on the echocardiographic appearances, oxygen saturations, and haemodynamic stability.
Outcomes
The primary outcome was survival to hospital discharge. Secondary outcomes included survival at 90 days, time to balloon atrial septostomy, time to arterial switch operation, pre-ductal oxygen saturation at neonatal ICU admission, highest recorded lactate prior to balloon atrial septostomy, need for unplanned invasive ventilation, neurological morbidity, and length of stay. Pre-ductal oxygen saturations were recorded at admission together with the lowest and mean pre-ductal saturations before balloon atrial septostomy (or in the first 24 hours if balloon atrial septostomy was not performed). Neurological morbidity was defined as abnormal neurological examination, seizures, documented abnormal neuroimaging (cranial ultrasound, CT or MRI), or abnormal electroencephalogram/cerebral function monitor at any time during the admission, or neurological impairment at follow-up. Length of stay was assessed from delivery to neonatal ICU, neonatal unit, and hospital discharge. Data were collected from electronic health records and detailed review of paper notes for each patient.
Statistical Analyses
Baseline characteristics were summarised for the included cohort of patients. Data for the pre-specified outcome variables were analysed for the subjects born in-hours and out-of-hours. Continuous parametric data were compared between groups using t-tests, with a 95% confidence interval and significance level of p < 0.05. Non-parametric variables were compared using the Mann–Whitney U-test, and categorical variables were analysed using the Fishers’ exact test. Univariable and multivariable linear regression was used for continuous outcomes. Single-level logistic regression was calculated for mortality and neurological morbidity, and adjusted odds ratios (OR) with 95% confidence intervals reported. Potential confounding variables and competing exposures were adjusted for, including gestational age, weight, mode of delivery (elective or emergency), and presence of antenatal rASD. Time to balloon atrial septostomy was analysed for all balloon atrial septostomy procedures performed within 12 hours of delivery. Secondary analyses were performed using data for subjects who were antenatally suspected to have a rASD. Statistical analysis was performed using SPSS Version 28.0.1.0 (IBM SPSS Statistics).
Ethical approval
This study was a review of local service performance using routinely collected patient data and was granted approval by the local clinical governance department. All patients are informed that data are routinely collected for audit purposes and can opt-out at any time. Research Ethics Committee approval was not required according to NHS Health Research Authority guidance.
Results
During the study period, we identified 76 cases of antenatally diagnosed transposition of the great arteries in our fetal database. From these, 54 patients had postnatally confirmed transposition of the great arteries and were included in the analysis. Three neonates were planned for delivery in the tertiary centre, but were unexpectedly delivered in surrounding hospitals without an on-site paediatric cardiology service. Data for several variables, including time of delivery, were unavailable for these cases. Details of the excluded cases can be found in Figure 1. Most neonates born out-of-hours were delivered by vaginal delivery (87% versus 62%, p = 0.10), and Caesarean section was more common in-hours (38% versus 13%, p = 0.10). Baseline characteristics for the included patients are displayed in Table 1.
Table 1. Patient demographics for out-of-hours and in-hours delivery groups at baseline.
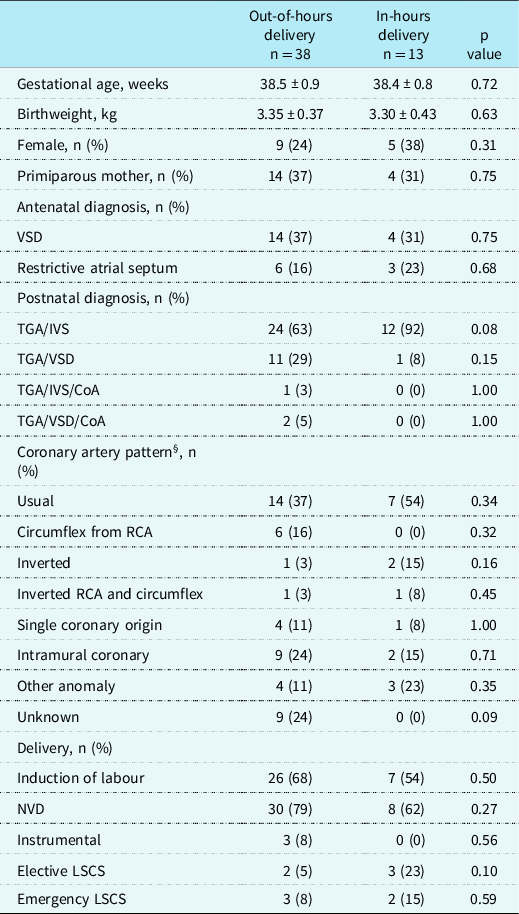
Values are stated as mean ± standard deviation or total (percentage). VSD, Ventricular Septal Defect; TGA, Transposition of the Great Arteries; IVS, Intact Ventricular Septum; CoA, Coarctation of the Aorta; RCA, Right Coronary Artery; NVD, Normal Vaginal Delivery; LSCS, Lower Segment Caesarean Section.
Out-of-hours delivery is defined as Monday to Friday 17:00–08:00 and weekends.
§Coronary patterns as defined by Wernovsky and Sanders. Reference Wernovsky and Sanders9
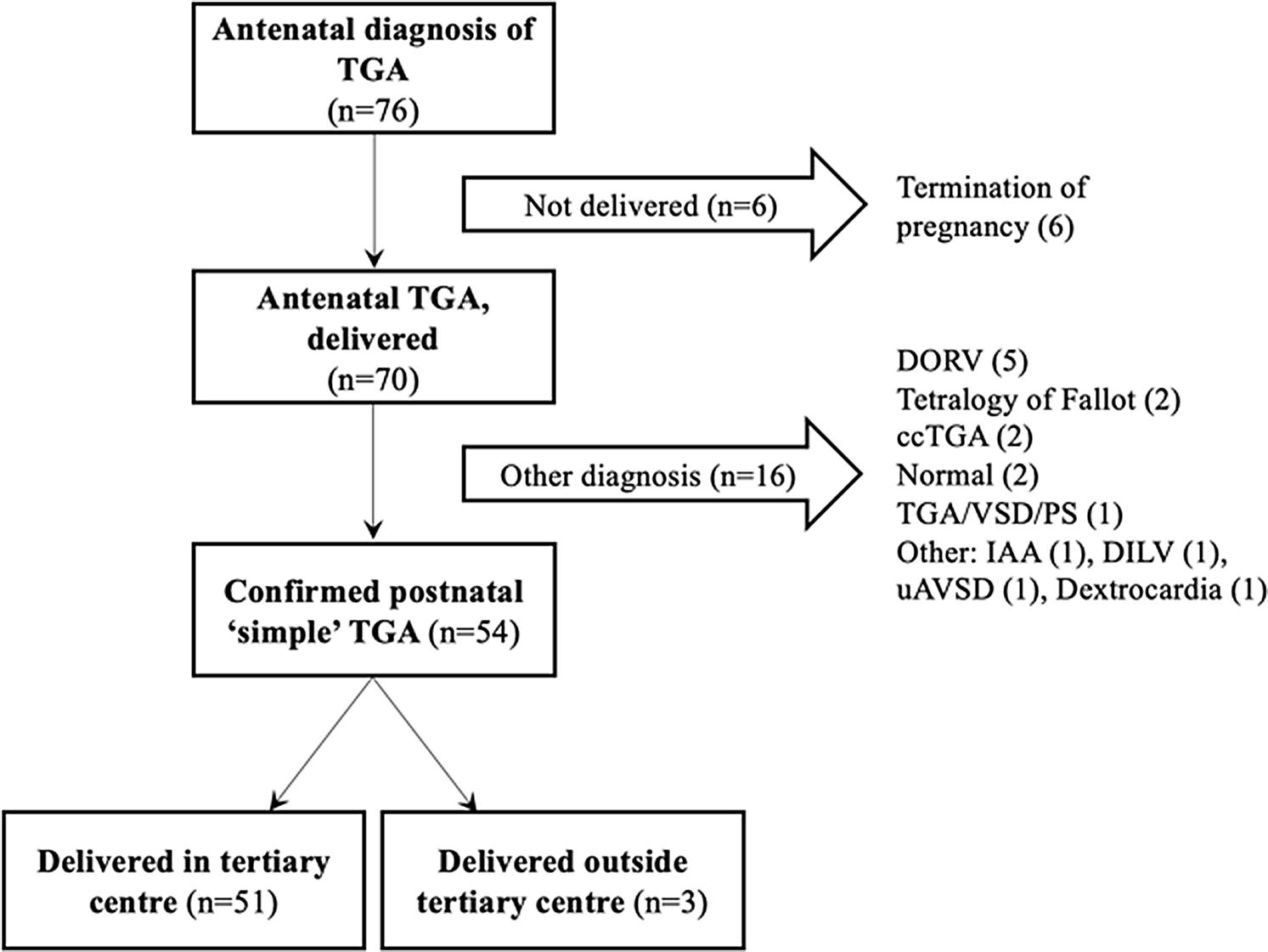
Figure 1. Selection of the study cohort. TGA, transposition of the great arteries; DORV, double outlet right ventricle; ccTGA, congenitally corrected transposition of the great arteries; VSD, ventricular septal defect; PS, pulmonary stenosis; IAA, interrupted aortic arch; DILV, double inlet left ventricle; uAVSD, unbalanced atrioventricular septal defect.
Of the 51 cases born in the tertiary centre, 38 (75%) were delivered out-of-hours. All neonates survived hospital discharge; however, one death before 90 days occurred in the out-of-hours group (OR 1.08 versus in-hours; 95% CI: 0.04–28.1, p = 0.96). Neurological morbidity occurred in 9 (24%) neonates born out-of-hours and 1 (8%) born in-hours (adjusted OR 5.31, 95% CI: 0.49–57.30, p = 0.17) (Table 2). For the neonates delivered in surrounding hospitals, two (67%) died shortly after delivery, before they could be transferred to the cardiac centre. One of these had a rASD antenatally. Therefore, mortality at discharge was significantly higher for deliveries outside the cardiac centre (OR 172; 95% CI: 5–5371, p = 0.003).
Table 2. Univariable and multivariable analyses of binary outcomes.
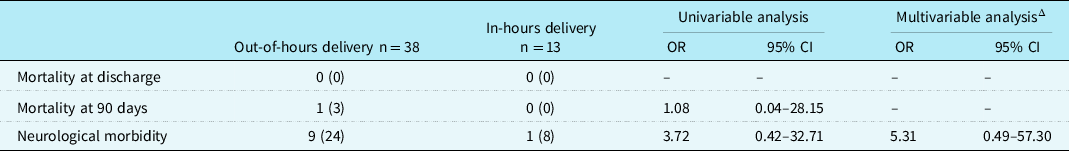
Values are stated as total (percentage). OR, Odds Ratio; CI, Confidence Interval.
Δ The model was adjusted for gestational age, birthweight, delivery type (emergency versus non-emergency). Out-of-hours delivery is defined as Monday to Friday 17:00–08:00 and weekends.
Balloon atrial septostomy was performed in 42 of 51 (82%) patients, with 9 (18%) having evidence of a rASD antenatally. The median time to balloon atrial septostomy was slightly longer for out-of-hours deliveries (130 mins versus 93 mins; p = 0.27). On multivariable analysis, time to balloon atrial septostomy was not significantly different between groups (β 82, 95% CI: −87–251, p = 0.33) when adjusted for gestational age, birthweight, and emergency delivery (Table 3). The median length of hospital stay was slightly longer for the out-of-hours group (18.5 days out-of-hours versus 17.3 days in-hours); however, this was not statistically significant on univariable or multivariable analysis.
Table 3. Univariable and multivariable analyses of continuous outcomes.
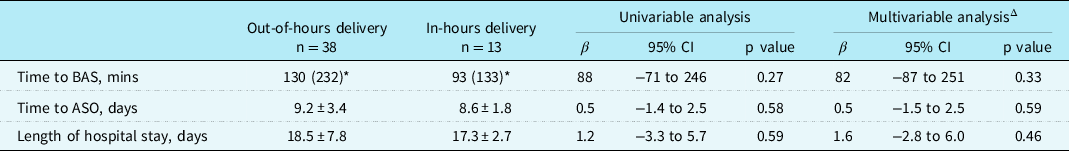
Group values are stated as mean ± standard deviation or median (interquartile range) (*). CI, Confidence Interval; BAS, Balloon Atrial Septostomy; ASO, Arterial Switch Operation. Out-of-hours delivery is defined as Monday to Friday 17:00–08:00 and weekends.
Δ The model was adjusted for gestational age, birthweight, delivery type (emergency versus non-emergency).
After delivery, all neonates were stabilised and commenced on a prostaglandin infusion. Median APGAR scores were similar at 1, 5, and 10 minutes for neonates delivered out-of-hours and in-hours. On admission to neonatal unit, both groups had similar pre-ductal oxygen saturations, pH, and lactate (Table 4). There was a trend towards a higher incidence of unplanned invasive ventilation (68% versus 38%, p = 0.10) for out-of-hours deliveries. Length of neonatal ICU stay was similar for both groups.
Table 4. Secondary outcomes for out-of-hours and in-hours delivery.
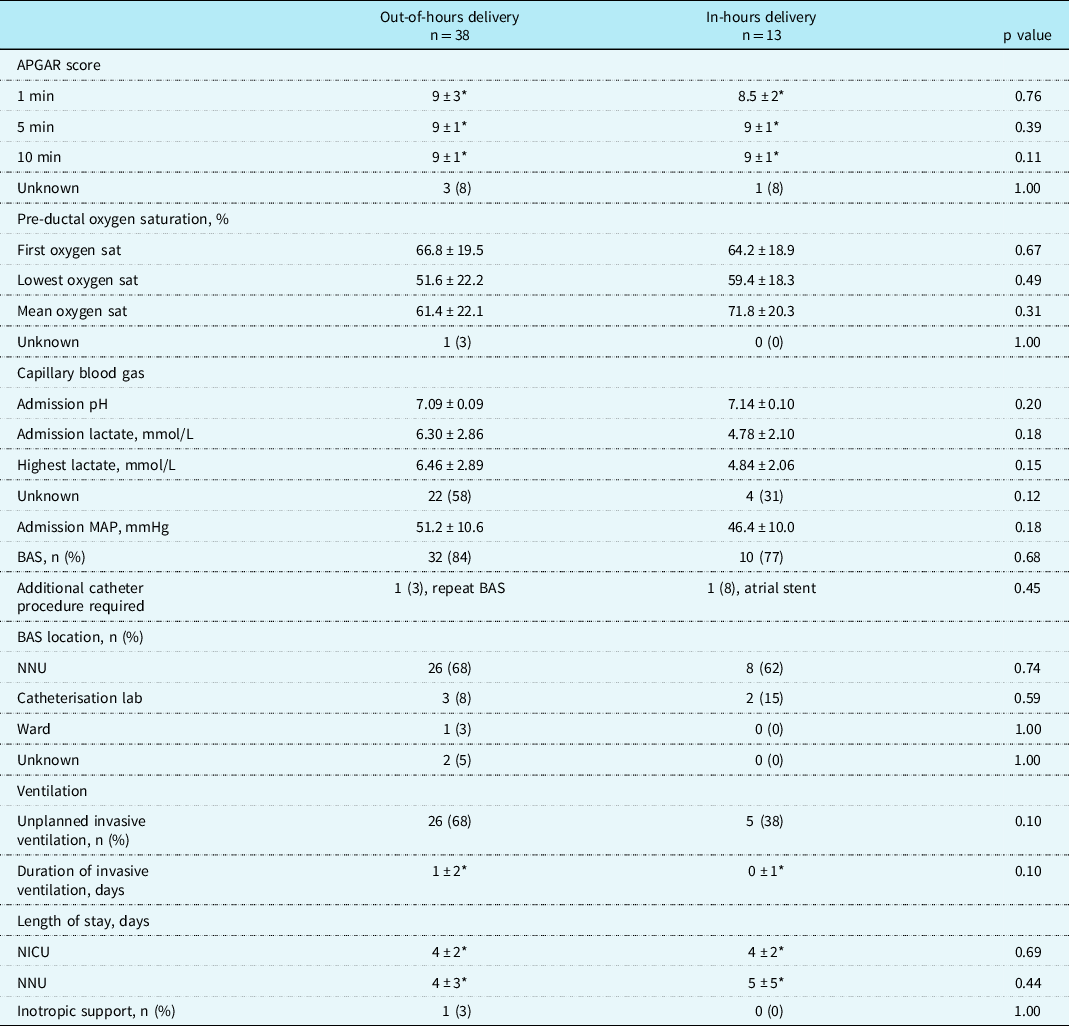
Values are stated as mean ± standard deviation, median ± interquartile range (*) or total (percentage). MAP, Mean Arterial Pressure; BAS, Balloon Atrial Septostomy; NNU, Neonatal Unit; NICU; Neonatal ICU. Out-of-hours delivery is defined as Monday to Friday 17:00–08:00 and weekends.
A secondary analysis was performed for neonates who were antenatally diagnosed to have a rASD. In this cohort, neonates with a rASD were more acidotic on admission (pH 7.03 ± 0.05 versus 7.13 ± 0.10, p = 0.01), and there was a trend towards higher peak lactate (8.01 ± 3.30 versus 5.47 ± 2.45 mmol/L, p = 0.08) and lower mean oxygen saturations (51.8 ± 32.9% versus 66.5 ± 20.8%, p = 0.37). All nine patients required emergency balloon atrial septostomy shortly after birth. The overall length of hospital stay was significantly longer for subjects with rASD antenatally (22.6 ± 12.7 versus 17.3 ± 4.6 days, p = 0.04). Four (44%) patients with rASD suffered neurological morbidity, compared to 6 (14%) without rASD (OR 4.80, 95% CI: 1.00–23.15, p = 0.05).
Discussion
In this study, we have retrospectively reviewed the outcomes of neonates antenatally diagnosed with simple transposition of the great arteries according to their time of delivery at our tertiary centre. For patients delivered at the tertiary cardiac centre, there was no significant difference in mortality at 90 days for neonates delivered out-of-hours. However, neonates delivered in surrounding hospitals had a significantly higher mortality. The out-of-hours group had a slightly longer median time to balloon atrial septostomy compared to in-hours (130 mins versus 93 mins), and neurological morbidity was more common (24% versus 8%); however, this was not statistically significant. There were no other significant differences for those born out-of-hours in length of stay or other neonatal parameters. Antenatal diagnosis of transposition of the great arteries with rASD is associated with more statistically significant acidosis postnatally and prolonged hospital admission, with a trend towards more severe hypoxaemia and increased neurological morbidity.
This is the first study examining the impact of timing of delivery for neonates with antenatally diagnosed transposition of the great arteries. Previously, Vimalesvaran et al. evaluated the outcomes of neonates undergoing balloon atrial septostomy out-of-hours compared to in-hours. Reference Vimalesvaran, Ayis and Krasemann7 This study included a United Kingdom cohort of 106 neonates, of which 83% had transposition of the great arteries. Authors found that balloon atrial septostomy performed out-of-hours resulted in significantly more complications (57% versus 30%), including femoral vein thrombosis and acute pericardial tamponade. Reference Vimalesvaran, Ayis and Krasemann7 A higher mortality in the out-of-hours group (29% versus 6%) was also observed. Whilst we did not see a mortality difference, there was a slightly longer time to balloon atrial septostomy for neonates delivered out-of-hours in our study. This supports our hypothesis that out-of-hours deliveries create pressure on staff and systems and may lead to delays. This is further evidenced by other studies of out-of-hours work in spinal surgery and intensive care. Reference Charest-Morin, Flexman and Bond10,Reference Morgan, Ho and Ong11
Multiple previous studies have demonstrated the advantages of antenatal diagnosis in ensuring optimal postnatal management and improved survival. Bonnet et al. reported on 318 neonates with transposition of the great arteries and observed significantly higher mortality for postnatally diagnosed neonates (14% versus 0% antenatally diagnosed). Reference Bonnet, Coltri and Butera4 This was associated with delays in admission to the paediatric cardiology unit compared with antenatal diagnosis (73 versus 2 hours). Two other recent studies found similar results, with significantly lower mortality after antenatal diagnosis. Reference Nagata, Glick and Lougheed3,Reference Van Velzen, Haak and Reijnders12 Delays to tertiary care admission, prostaglandin therapy, and balloon atrial septostomy as a result of postnatal diagnosis were closely linked to mortality. Reference Nagata, Glick and Lougheed3 Prolonged hypoxia has also been proven to predict pre-operative hypoxic brain injury. Reference Petit, Rome and Wernovsky5 Delivery out-of-hours may cause delays in treatment and balloon atrial septostomy, possibly due to reduced staffing and non-resident paediatric interventional cardiologists. The prolonged hypoxaemia experienced by neonates prior to undergoing balloon atrial septostomy may lead to longer term neurodevelopmental impairment. Long-term neurodevelopmental outcomes could not be assessed in our study.
We have observed 100% survival to discharge for our cohort. This is significantly higher than reported in previous literature. Reference Nagata, Glick and Lougheed3,Reference Mukherjee, Lindsay and Zhang13 There are several possible reasons to explain this. Firstly, we reviewed only antenatally diagnosed cases of transposition of the great arteries, where survival is known to be higher as described above. Secondly, 82% of neonates in our study underwent a balloon atrial septostomy procedure. Whilst this is a similar rate to several previous studies, Reference Nagata, Glick and Lougheed3,Reference Escobar-Diaz, Freud and Bueno14 there is some evidence of survival benefit for balloon atrial septostomy in transposition of the great arteries. Reference Mukherjee, Lindsay and Zhang13 Lastly, our centre benefits from co-located paediatric cardiology and tertiary neonatal units, which aids the rapid assessment and treatment of transposition of the great arteries cases. The higher survival in our cohort may have reduced our ability to detect any differences between the two groups.
Fetal diagnosis of transposition of the great arteries with rASD was associated with more severe acidosis, higher lactate, lower oxygen saturations, and longer length of stay in our cohort. There was also a trend towards higher neurological morbidity in this subgroup. It is recognised that antenatal diagnosis of rASD predicts acute haemodynamic instability and poorer outcome postnatally. Reference Maeno, Kamenir and Sinclair15–Reference Jouannic, Gavard and Fermont17 A study by Jouannic et al. investigated the effects of antenatally diagnosed atrial restriction in transposition of the great arteries. Reference Jouannic, Gavard and Fermont17 The prevalence of rASD was 19%, similar to the 18% we have reported. The authors reported similar findings, with rASD predicting profound hypoxaemia, metabolic acidosis, and need for emergency neonatal care after delivery. Reference Jouannic, Gavard and Fermont17 Antenatal rASD had a high specificity and low sensitivity for detecting high-risk fetuses. Our results support this, with 82% of all neonates in our cohort requiring balloon atrial septostomy for inadequate atrial mixing, and only the minority had known antenatal rASD. Atrial restriction is not always apparent in-utero and may manifest postnatally as pulmonary vascular resistance falls. Fetal echocardiography is therefore vital in identifying those that should have emergency care available immediately after delivery. However, the absence of rASD antenatally does not rule out the need for emergency treatment and balloon atrial septostomy, supporting our current practice of recommending delivery of all cases of antenatally diagnosed transposition of the great arteries in our tertiary centre so that rapid postnatal cardiac assessment can be made.
Limitations
The relatively small sample size may have impacted our results. This may explain the failure to reach statistical significance for some outcomes and a trend towards poorer outcome out-of-hours for multiple variables. The small and single-centre cohort also limits the generalisation of these results to other centres. However, this is a signal that further research with multi-centre collaboration is required into the effects of time of delivery in this patient population.
We conducted a retrospective review; therefore, there were inherent issues with incomplete data. To minimise the impact of this, we extensively reviewed paper and electronic records for every patient. Any remaining missing data affected both groups and therefore should not have biased results. The retrospective nature of our review of outcomes to discharge precluded additional assessment of neurological outcome. Neuroimaging was not routinely performed. Future work in this area may identify late-onset adverse neurodevelopmental consequences in children born with transposition of the great arteries that may be exacerbated by out-of-hours delivery.
Impact on current practice
In this study, we have shown that there is excellent survival of neonates with antenatally diagnosed transposition of the great arteries delivered at our tertiary centre. However, we have found that neonates delivered out-of-hours may experience delays in balloon atrial septostomy and are therefore at higher risk of prolonged hypoxaemia. We also found that neonates born outside the tertiary cardiac centre have a higher mortality. Previous evidence is clear that delays in receiving emergency neonatal care after delivery results in prolonged hypoxia, neurological injury, and reduced survival. Reference Nagata, Glick and Lougheed3–Reference Petit, Rome and Wernovsky5 Out-of-hours care has been previously associated with increased complications after balloon atrial septostomy. Reference Vimalesvaran, Ayis and Krasemann7 Our findings support our local aim to ensure that all cases of antenatally diagnosed transposition of the great arteries continue to be delivered at our tertiary centre with co-located paediatric cardiology service where possible. We have also shown that fetuses with rASD are at highest risk for poor neonatal outcome, in agreement with previous studies. Reference Maeno, Kamenir and Sinclair15–Reference Jouannic, Gavard and Fermont17 As a result of this, we now offer elective in-hours Caesarean section to mothers where transposition of the great arteries with rASD has been diagnosed.
Conclusion
Neonates with antenatally diagnosed transposition of the great arteries have similar outcomes when delivered out-of-hours versus in-hours. Antenatal diagnosis of rASD is a significant predictor of postnatal instability and worse neurological outcome. Given the challenges of predicting the need for balloon atrial septostomy, there may be benefits to planning for in-hours delivery. For the benefit of survival, we advocate all efforts be made to ensure delivery at a tertiary neonatal unit with cardiac experience and established rapid access pathways for paediatric cardiac intervention.
Acknowledgements
We would like to thank Stacey Boardman for her assistance with data collection.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.








