Platypnea–orthodeoxia syndrome is distinguished by a combination of dyspnoea and arterial desaturation in the upright position.Reference Seward, Hayes and Smith1 It is usually caused by intra-cardiac right-to-left shunting through a patent foramen ovale or atrial septal defect, but may also occur due to ventilation-perfusion mismatch in severe pulmonary disorders and chronic liver disease.Reference Mojadidi, Christia and Salamon2,Reference Yoshida, Nambu and Matsubara3 There are several reports of platypnea–orthodeoxia syndrome resulting from patent foramen ovale and of therapeutic outcomes in adults. We describe a child diagnosed with platypnea–orthodeoxia syndrome undergoing successful transcatheter closure of a patent foramen ovale.
Case report
A 12-year-old girl was admitted to our clinic with headache, tremor, dyspnoea and oxygen desaturation in the upright position. She had a medical history of postural hypotension with inappropriate sinus tachycardia treated with beta blocker therapy. She had been diagnosed with hypermelatoninemia as a cause of hypothermia during infancy. Abdominal pain attacks had commenced at 4 years of age, and she had been using colchicine with a diagnosis of Familial Mediterranean Fever. Glaucoma was diagnosed at 7 years because of relapsing headaches. She had also been using betaxolol HCL eye drops to control increased intraocular pressure. Low oxygen saturation was detected by the family when checking her heartbeat using portable pulse oximetry during her symptoms. She was unable to remain standing for more than a few minutes and described symptoms of headache, tremors and dizziness, which were relieved by assuming the prone position.
Physical examination and blood chemistry findings were unremarkable. Oxygen saturation values measured in the prone and upright positions in the hospital were 99% and 75%, respectively. Partial pressure of arterial oxygen values in the prone and upright positions were 124 and 102 mmHg, respectively. Diagnosis of platypnea–orthodeoxia syndrome was considered. Transthoracic echocardiography with bubble contrast was normal. Thoracic CT, ventilation/perfusion scintigraphy and portal venous Doppler were also normal.
Transesophageal echocardiography and cardiac catheterisation were performed under general anaesthesia. Transesophageal echocardiography revealed a patent foramen ovale tunnel and floppy atrial septum, but without obvious right-to-left shunting in the supine position (Fig 1). Right and left atrium mean pressures were 9 and 11 mmHg, respectively, and pulmonary artery pressure was 25/13, with a mean value of 18 mmHg. No shunt was observed at pulse oximetry. A 0.035-inch guidewire was passed easily through a 5 F vertebral catheter into the left atrium. Patent foramen ovale width via a balloon sizing catheter was 7.5 mm (Fig 2a). The defect was successfully closed using a 9 mm Amplatzer septal occluder (Fig 2b). Control transesophageal echocardiography and contrast injection showed no residual shunt (Fig 2c). The day after transcatheter patent foramen ovale closure, oxygen saturation and partial pressure of arterial oxygen were normal in the upright position and the symptoms disappeared completely. A 6-minute walking test revealed normal oxygen saturation (pre- and post-test saturations were 99% and 98%, respectively). The patient was discharged after 72 hours with 5 mg/kg aspirin therapy. She remains asymptomatic at 6 weeks of follow-up and can perform all daily activities and work without signs of desaturation.

Figure 1. Transesophageal echocardiography revealed a patent foramen ovale (PFO) tunnel and floppy atrial septum (arrow PFO tunnel and * floppy atrial septum).
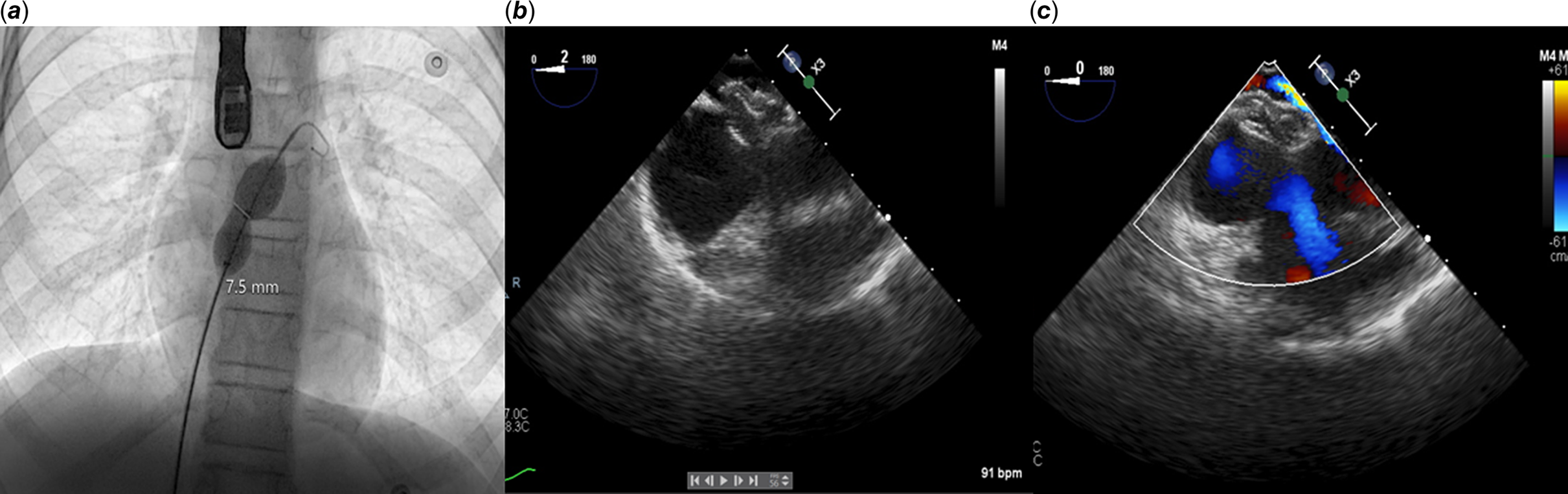
Figure 2. ( a ) The width of the patent foramen ovale (PFO) was measured at 7.5 mm using a balloon sizing catheter. ( b and c ) Control transesophageal echocardiography revealed no residual shunt on the 9 mm Amplatzer septal occluder.
Discussion
The hypoxia in platypnea–orthodeoxia syndrome has been attributed to the mixing of deoxygenated venous blood with the oxygenated arterial blood via a shunt. The primary mechanisms of platypnea–orthodeoxia syndrome in these patients can be broadly classified based under intra-cardiac abnormalities, extracardiac abnormalities and miscellaneous aetiologies. Patent foramen ovale is the most commonly reported site of intra-cardiac shunt.Reference Seward, Hayes and Smith1,Reference Sorrentino and Resnekov4,Reference Springer, Gheorghiade and Chakko5 It has been suggested that blood shunt occurs across the inter-atrial communication in the presence of right atrial pressure elevation. Interestingly, even in the absence of right atrial hypertension, deoxygenated blood shunt occurs from the right to the left atrium across patent foramen ovale in the presence of a concomitant secondary cardiac or pulmonary functional aberration.Reference Sorrentino and Resnekov4
The present case is interesting because of the presentation age, absence of right atrial hypertension and normal right ventricle function and pressure. The linkage between the platypnea–orthodeoxia syndrome and the patient’s previous illnesses, such as hypermelatoninemia, Familial Mediterranean Fever and glaucoma, is unclear. To the best of our knowledge, the literature contains only adult case reports of platypnea–orthodeoxia syndrome secondary to patent foramen ovale. Some patients with congenital inter-atrial communication such as patent foramen ovale, atrial septal defect or atrial septal aneurysm only develop symptoms of platypnea–orthodeoxia syndrome in late adulthood because of degenerative aortic root dilatation.Reference Eicher, Bonniaud and Baudouin6
Definitive treatment of platypnea–orthodeoxia syndrome due to intra-cardiac shunt involves correction of the primary cardiac anomaly. This may involve closure of the patent foramen ovale or surgical repair of the atrial septal defect. While surgery was for years the mainstay for the closure of patent foramen ovale and atrial septal defect, percutaneous intervention has recently supplanted surgery due to decreased morbidity rates and lower costs.Reference Cheng7 Symptom improvement with percutaneous closure is observed in more than 95% of patients. A 10–20% increase in upright oxygen saturation has been reported after corrective surgery.Reference Toffart, Bouvaist, Feral, Blin and Pison8 Guerin et al performed a retrospective multi-centre study of 78 patients (mean age 67 ± 11 years) presenting with platypnea–orthodeoxia syndrome of all types and undergoing percutaneous patent foramen ovale closure. The procedure was successful in 76 cases, with immediate improvement of oxygen saturation and dyspnoea.Reference Guerin, Lambert and Godart9 Our case exhibited a very good immediate post-procedural response to transcatheter closure of the atrial septal shunt and restoration of normal daily life during follow-up.
Conclusion
The presentation of platypnea–orthodeoxia syndrome can be subtle, and diagnosis of platypnea–orthodeoxia syndrome requires a high degree of suspicion. Measurement of oxygen saturation in the standing position can be diagnostic in the presence of symptoms mimicking neurological and autonomic diseases. Right-to-left intra-cardiac shunt can be successfully treated by cardiac catheterisation.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, or from commercial or not-for-profit sectors.
Conflict of interest
None.
Ethical standards
All procedures performed in this case were in accordance with the ethical standards of the institutional and national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patient’s parents.





