Introduction
Vasovagal syncope is one of the common hemodynamic types of neurally mediated syncope, Reference Wang, Li and Liao1,Reference Kenny, Bhangu and King-Kallimanis2 accounting for 60–70% of syncope in children, Reference Chen, Wang and Wang3 and its neuroreflex-mediated bradycardia and hypotension may cause transient cerebral underperfusion followed by falls and even accidental bodily injury. Reference Cannom4,Reference Sheldon, Grubb and Olshansky5 Most pediatric vasovagal syncope have self-limiting syncopal symptoms without sequelae after anesis, and the prognosis is mostly good in the medium term. Reference Díaz, Tercedor and Moreno6 Some children have recurrent syncopal symptoms, which may be accompanied by cardiac arrest lasting more than 3 s or severe hypotension and bradycardia, and then proceed to malignant vasovagal syncope. Reference Xu, Jin and Du7 In total, 33% of vasovagal syncope patients suffer from somatic injuries due to syncope. Reference Jorge, Raj, Teixeira and et al8 Recurrent syncope episodes lower the health-related quality of life of vasovagal syncope patients and predispose them to anxiety and depression. Reference Choi, Han and Lee9
The pathogenesis of vasovagal syncope is associated with hypovolemia, Reference Tao, Tang, Jin and et al10,Reference Song, Tao and Chen11 autonomic dysfunction, Reference Song, Li and Wang12 vasoconstriction dysfunction, Reference Xu, Du and Jin13 increased pressure reflex sensitivity, Reference Tao, Li, Tang and et al14 and increased plasma human growth factor. Reference Liao, Xu and Li15,Reference Wang, Wang and He16 Patients with head-up stress-induced pre-syncope would present with cerebral hypoperfusion secondary to reduced diastolic cerebral blood flow velocity. Reference Sung, Du, Yu and et al17 Thus, clinical intervention strategies for vasovagal syncope are to strengthen health education, avoid syncope triggers, Reference Xu, Du and Jin13 increase water and salt intake, Reference Wang, Wang and Li18 and emphasise standing training Reference Tao, Tang, Chen and et al19 ; medications are available as α-agonists, β-blockers, and 5-hydroxytryptamine reuptake inhibitors. Reference Shen, Sheldon and Benditt20,Reference Brignole, Moya and de Lange21 Head-up tilt test (HUTT) reproduces syncope or pre-syncope episodes with hemodynamic alterations by passively changing the subject’s position to stimulate autonomic dysfunction and is the primary methodology for diagnosing vasovagal syncope. Reference Wang, Li and Liao1
HUTT is divided into two modes: basic head-up tilt test (BHUT) and sublingual nitroglycerine head-up tilt test (SNHUT). The operation duration of BHUT is 45 minutes, while that of SNHUT is an additional 20 minutes on top of BHUT. The time of HUTT is selected according to the circadian rhythm characteristic of the syncope symptom episodes, Reference Liao, Xu and Zou22 and it is usually scheduled to be performed from 08:00 a.m. to 11:00 a.m. Some hospitals have a large number of syncope patients, resulting in longer waiting time for test appointments, which prevents syncope patients from receiving timely diagnosis and treatment. Russo et al. Reference Russo, Parente and Comune23 reported a correlation between clinical syncope presentation and the rate of positive HUTT and type of syncopal response in adult vasovagal syncope patients. Therefore, we wanted to know if there is an association between syncopal symptoms and HUTT modes in pediatric vasovagal syncope? In addition, due to the time required for HUTT, a limited number of children can be examined during working hours, which may result in children cannot be identified timely, and the number of children to be examined by appointment needs to be rationally optimized. Reference Haynes and Sweeney24
In this research, we retrospectively analysed the HUTT data of pediatric vasovagal syncope in a single centre for the past 20 years to explore the possible relationship between syncopal symptoms and HUTT modes, and to provide the HUTT laboratory technicians with a rational HUTT appointment for the number of children to be examined based on previous syncopal symptoms, to shorten the waiting time for as many tests as possible for the children and identify the cause of syncope episodes early.
Materials and methods
Study population
In total, 2513 children with unexplained syncope or pre-syncope (e.g., dizziness, headache, chest tightness, chest pain, palpitations, sighing, blurred vision, etc.) who attended the Pediatric Syncope Specialist Outpatient Clinic, The Second Xiangya Hospital, Central South University, and first diagnosed with vasovagal syncope, aged 3–18 years, mean 11.76 ± 2.83 years, 1124 males and 1389 females. The participants of the research were divided into BHUT group (596 patients) and SNHUT group (1917 patients) according to different HUTT positive modes (Fig 1).

Figure 1. Flow chat.
The research involving human participants was reviewed and approved by the Medical Ethical Committee, The Second Xiangya Hospital, Central South University. Written informed consent to participate in this research was provided by the participants’ legal guardian/next of kin.
Inclusion and exclusion criteria
From Jan. 2001 to Dec. 2021, 6364 children aged 3–18 years with unexplained syncope or pre-syncope underwent HUTT in The Second Xiangya Hospital, Central South University. Inclusion criteria: There were 2513 cases of pediatric vasovagal syncope, 1124 in males and 1389 in females. Exclusion criteria: 3851 cases did not meet the diagnostic criteria for vasovagal syncope (Fig 1).
HUTT
HUTT is performed after detailed medical history, physical examination, electrocardiogram, Holter electrocardiogram, echocardiography, electroencephalogram, cranial MRI/CT, fasting glucose, cardiac enzymes, liver, and kidney function tests to exclude syncope or pre-syncope caused by organic diseases such as heart, kidney and brain, immune diseases, and metabolic diseases before HUTT.
Subjects discontinued cardiovascular active drugs for more than five half-lives prior to the test Reference Chen, Wang and Wang3 and discontinued foods that may affect autonomic function. Fasting and abstaining from drinking 4h before the test. Subjects or guardians were briefed on pre-test precautions and possible risks during the test, and written informed consent was signed by the subjects themselves or their legal guardians. HUTT modes were divided BHUT and SNHUT.
BHUT
Tilt device adopts ST-711 HUTT System (Beijing Juchi Medicine Technology Co., Ltd) and HUTT Monitoring System (SHUT-100) of Jiangsu Standard Medical Technology Co. Monitoring System (SHUT-100, Jiangsu Standard Medical Technology Co., Ltd). From 8:00 a.m. to 11:00 a.m., room temperature was 20–24°C, in a quiet environment, the subjects emptied their bladders, rested supine on a tilted diagnostic bed for 10 min, knee joints were fixed with a girdle to avoid flexion, basal heart rate (HR), right upper limb blood pressure (BP) and electrocardiogram were recorded, and within 15 s, they were converted to a 60° head-up tilt position, and HR, BP, and electrocardiogram were continuously monitored and recorded until a positive response was observed, the test was terminated, and the patient returned to the horizontal position within 10 s. If there is discomfort monitor at any time until a positive response occurs or until 45 min of the procedure is reached. Reference Wang, Li and Liao1
SNHUT
BHUT negative subjects continued to maintain the same tilt angle position, Reference Wang, Li and Liao1 and subjects were given sublingual nitroglycerine tablets (4–6 μg/kg, maximum amount ≤ 300 μg), and HR, BP, and electrocardiogram were continuously monitored until a positive response appeared or until a positive response did not appear for 20 min, then the test was terminated, and the tilt bed was quickly placed in the horizontal position, and HR, BP, and electrocardiogram were continued to be monitored after the horizontal position until the above indicators returned to normal.
Diagnostic criteria for vasovagal syncope
A positive response is considered when a subject experiences syncope or pre-syncope during HUTT with one of the following conditions Reference Wang, Li and Liao1 : (i) a decrease in BP; (ii) a decrease in HR; (iii) the presence of sinus arrest, junctional escape rhythm; and (iv) a transient second-degree or higher atrioventricular block and cardiac arrest of up to 3 s. BP decrease is defined as a systolic blood pressure (SBP) ≤ 80 mmHg (1 mmHg = 0.133 kPa) or a diastolic blood pressure (DBP) ≤ 50 mmHg or a decrease in mean BP ≥ 25%. HR decrease refers to bradycardia: HR < 75 bpm at age 3–6 years, < 65 bpm at age 6–8 years, and < 60 bpm at age 8 years or older.
Statistical analysis
The continuous variables were characterised by mean ± standard deviation or as median and interquartile range, as appropriate. The categorical variables were presented as a number (n) and percentages (%). The Student’s t test, Chi-square test, Fisher’s exact test, or Mann-Whitney U test were conducted to compare factors between two groups, as appropriate. We used multiple Logistic regression to analyse the possible association between syncopal symptoms and HUTT positive modes and constructed two models to illustrate the stability of this relationship. All the analyses were performed with the statistical software packages R (version 3.6.1) (http://www.R-project.org, The R Foundation) and EmpowerStats (http://www.empowerstats.com, X & Y Solutions, Inc., Boston, MA). P-values < 0.05 (two-sided) were considered statistically significant.
Results
Comparison of basic characteristics between BHUT group and SNHUT group in pediatric vasovagal syncope
A total of 2513 pediatric vasovagal syncope, 1124 males (44.73%), were enrolled in this research. At baseline status, age, height, weight, HR, SBP, and DBP were higher in the BHUT group than in the SNHUT group, and the composition ratio of syncope was higher in the BHUT group than in the SNHUT group (all P < 0.05) (Table 1).
Table 1. Comparison of basic characteristics between BHUT group and SNHUT group in pediatric VVS [Mean ± SD, n (%)]
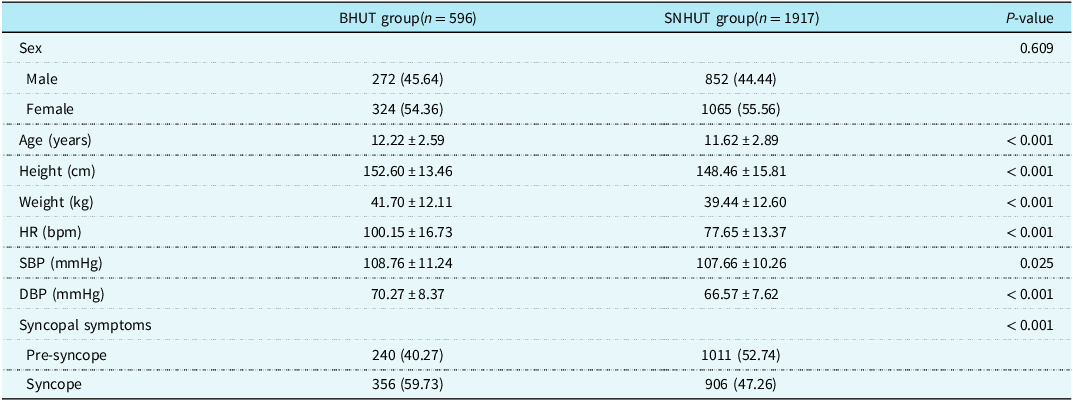
VVS = vasovagal syncope; BHUT = basic head-up tilt test; SNHUT = sublingual nitroglycerin head-up tilt test.
Univariate analysis for BHUT positive
Univariate analysis showed that female, age, height, weight, SBP, DBP, and syncope were potential risk factors for BHUT positive, and syncope was 66% higher than pre-syncope for BHUT positive (all P < 0.05) (Table 2).
Table 2. Univariate analysis for BHUT positive [Mean ± SD, n (%)]
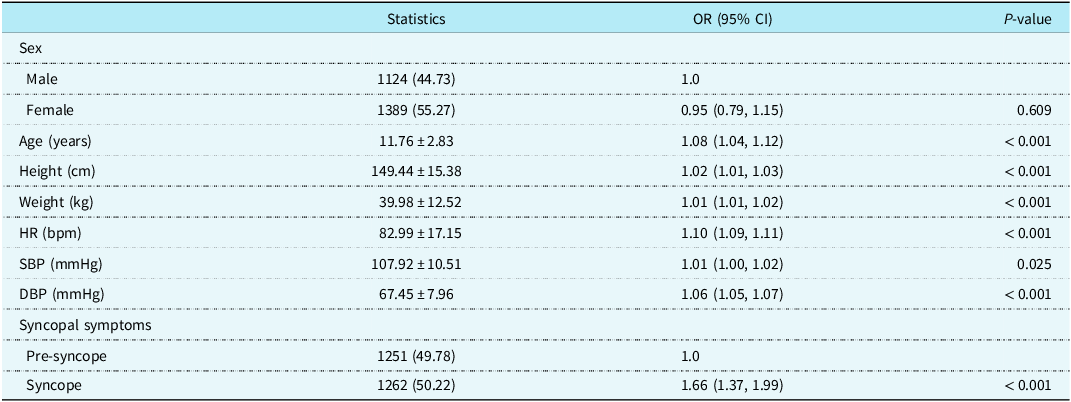
HUTT = Head-up tilt test; BHUT = basic head-up tilt test; HR = Heart rate; SBP = systolic blood pressure; DBP = diastolic blood pressure.
Result Variable: BHUT positive.
Exposure variables: sex, age, height, weight, HR, SBP, DBP, and syncopal symptoms.
Adjust variables: none.
Comparison of multiple multi-factor Logistic regressions
In this research, three models were constructed to demonstrate whether the effect of different syncopal symptoms on the HUTT positive modes existed independently in the univariate analysis. Table 3 shows that after adjusting for demographic factors (Model 2), the risk effect of syncope compared with pre-syncope on BHUT positive was stable (1% reduction in OR in Model 2 compared with Model 1) and the effect was significant (P < 0.001). After further adjustment for other factors (Model 3), the risk effect of syncope compared to pre-syncope on BHUT positive was enhanced (Model 3 compared to Model 2, OR increased by 56% and the effect was mainly from HR, SBP, and DBP at baseline) and remained significant (P < 0.001). That is, after accounting for the effects of all the above confounding factors, the probability of BHUT positive for syncope compared with pre-syncope was increased by 121% (Table 3).
Table 3. Multivariate analysis for BHUT positive
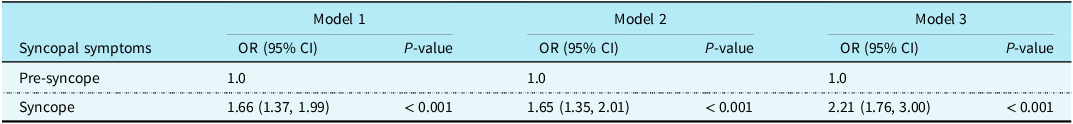
Result Variable: BHUT positive.
Exposure variables: syncopal symptoms.
Model 1 adjust for: none.
Model 2 adjust for: sex, age, height, weight.
Model 3 adjust for: sex, age, height, weight, HR, SBP, DBP.
Discussion
There are various clinical manifestations of pediatric vasovagal syncope, and in addition to the typical syncopal symptoms, Reference Chen, Wang and Wang3 there can be different forms of pre-syncope, such as unexplained dizziness, Reference Wang, Mao and Li25 headache, chest tightness, chest pain, Reference Wang, Wang and Zou26 palpitations, sighing, Reference Zou, Wang and Li27 abdominal pain, Reference Yan, Zhang, Du and et al28 and amaurosis fugax. The correlation between syncopal symptoms and HUTT modes has not been reported yet in pediatric vasovagal syncope. The present research retrospectively analysed the clinical data of children diagnosed with vasovagal syncope in a single centre for 20 years and investigated the relationship between syncopal symptoms and HUTT modes, and a significantly higher positive rate of BHUT group than SNHUT group was found in children with previous syncopal episodes. This effect remained stable after accounting for confounders such as HR, SBP, and DBP in the initial state, suggesting that a prior history of syncopal episodes is an independent risk factor for positive BHUT.
For this research, age, height, weight, HR, SBP, and DBP were higher in the BHUT group than in the SNHUT group at baseline status. Children with a history of previous syncopal episodes are more likely to evoke a positive response in BHUT mode, which may be related to the enlarged inferior vena cava in children with syncope and the resulting excess venous volume pooling in the inferior part of the body. Reference Shivaram, Angtuaco and Ahmed29 Although pediatric vasovagal syncope with BHUT positive had relatively increased SBP and DBP at baseline status, they were consistently below the 10th percentile and there was no change in baseline HR, which provides a basis for adding salt to food when developing interventions for pediatric vasovagal syncope. Reference Adlakha, Gupta, Hassan and et al30 In addition, plasma norepinephrine and epinephrine levels were significantly increased during HUTT in vasovagal syncope patients from baseline to just before syncope recurrence and decreased when syncope recurrence. Reference Hackel, Linzer, Anderson and et al31,Reference Kohno, Detloff, Chen and et al32 High levels of plasma epinephrine in children with syncope may mediate increased cardiac contractility, increase the sensitivity of the Bezold-Jarisch reflex, and may lead to an impaired vasoconstrictor response, Reference Leonelli, Wang and Evans33 increasing susceptibility to vasovagal syncope. Pediatric vasovagal syncope with elevated total peripheral resistance and reduced cardiac output during the transition from the supine position to the emergence of a positive response also tend to reduce cerebral blood supply in HUTT, Reference Li, Liao and Han34 Increased SBP levels and reduced RR interval high-frequency power during childhood compared to adolescence suggest the presence of reduced vagal activity in children. Reference Tanaka, Borres and Thulesius35 The dysregulation of cardiovascular autonomic function after puberty is associated with increased BP levels caused by increased regulation of cardiac vagal activity. Additionally, pediatric vasovagal syncope with BHUT positive, increased baseline state height and hydrostatic pressure, and relatively reduced cerebral blood supply are also prone to cerebral hypoperfusion, but they are able to prevent abrupt changes in cerebral blood supply through hypertrophy of the heart and small arterial walls and adaptive changes with the circulatory system. Reference Liu, Gao and Cui36 Weight increases are supposed to enhance the action of the muscle pump of the lower limbs, providing the necessary energy for venous blood return to the lower limbs, but also to increase relatively more blood return to the heart through the squeezing effect, which enhances venous contraction and diastole Reference Spáčil37 and provides blood supply to the brain. In supine and tilt positions, raised sympathetic activity is associated with increased adipose tissue composition in young healthy people, Reference Smoljo, Stanić and Sila38 and increased weight in children is instead detrimental to the maturation of cardiac autonomic function, Reference Eyre, Duncan and Birch39 but the increased body surface area that accompanies weight gain spreads the blood volume distribution relatively sparsely and thus is detrimental to increased overall return blood volume, which can also lead to inadequate cerebral blood supply. Therefore, weight gain in the BHUT group at baseline may increase autonomic dysfunction.
Children with a history of previous syncopal episodes and who require the aid of sublingual nitroglycerine to elicit a positive result when exhibiting a negative BHUT during HUTT suggest that they are already better tolerated to syncopal symptoms at baseline and that these populations are at reduced risk of syncope in daily life. This is related to their relatively low height, weight, HR, SBP, and DBP at baseline, suggesting relatively low sympathetic activity and relatively high vagal function activity, which is less likely to trigger the Bezold-Jarisch reflex.
Clarifying the effect of different syncopal symptoms on the HUTT modes is a guidance for laboratory staff to rationally appoint the children to undergo the examination. Reference Taylor, Bottrell and Lawler40,Reference Parikh, Gupta and Wilson41 At the same time, since the examination time of BHUT is shorter than that of SNHUT, it can be considered to increase the number of appointments for children with a history of previous syncopal episodes, so that the diagnosis can be clarified early.
Conclusion
Children with a history of previous syncopal episodes have a significantly higher probability of being BHUT positive, which is an independent risk factor for BHUT positivity. At the same time, different syncope symptoms can provide a reference for HUTT laboratory technicians to rationalise the number of children to be examined during working hours, and to clarify the aetiology of other children as soon as possible.
Acknowledgements
We thank the study participants for volunteering to participate in this research.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
CW conceived the study. SW, YP, YW, FL, YX, HZ, HY, CH, DL, HC, JZ, WL, YD, WZ, XX, XL, LZ, DL, MK, LL, WC, XL, XL, and RZ collected and reviewed patient data. SW performed statistical analysis and drafted the manuscript, and all authors contributed to its revision. The author(s) read and approved the final manuscript.
Financial support
National High Level Hospital Clinical Research Funding (Multi-center Clinical Research Project of Peking University First Hospital) (2022CR59) and Natural Science Foundation of Hunan Province (2023JJ30812) and Department of Science and Technology of Hunan Province (2023SK4018) and Health Commission of Hunan Province (202106011637).
Competing interests
The authors declare that they have no competing interests.
Ethics standards
The research was conducted according to the guidelines of the Declaration of Helsinki, and approved by The Second Xiangya Hospital, Central South University [Ethical Audit No. Study 249(2022)]. All participants or their responsible guardians were asked for and gave their written consent after being informed about the nature of the study.







