Middle aortic syndrome is an uncommon condition defined as diffuse narrowing of the abdominal or distal thoracic aorta, which often involves the renal and splanchnic arterial branches. It may be associated with genetic syndromes, but in 60% of cases, it occurs without an identifiable cause. Although middle aortic syndrome is uncommon, 0.5–2% of all aortic narrowing, it is one of the important causes of renovascular hypertension in children and adolescents.Reference Sethna, Kaplan and Cahill1 Medical treatment of renovascular hypertension caused by middle aortic syndrome has mostly failed, and invasive intervention is often needed to achieve sufficient blood pressure regulation.Reference Rumman, Nickel and Matsuda-Abedini2 Surgical repair has different limitations such as recurrent operations due to graft inability to growth. Although percutaneous intervention offered an alternative treatment option in recent years, data are still limited regarding percutaneous interventions of middle aortic syndrome.Reference Tummolo, Marks and Stadermann3 In this manuscript, we present a case of a 12-year-old girl, whose severe middle aortic syndrome was treated successfully with percutaneous aortic endovascular stent implantation.
Case report
A 12-year-old girl was admitted to our hospital with headache and refractory hypertension, despite taking 2 different antihypertensive agents (captopril and carvedilol). In her previous history, the patient was applied balloon dilatation due to aortic coarctation in the neonatal period. Afterwards, at the age of 7, recoarctation was developed and repaired by surgical revascularisation procedure with a graft anastomosis.
On physical examination, the patient was in good condition with a body weight and height in the 25–50th percentile. There was 2/6 systolic murmur best heard at the left upper sternal border. Her right and left arm office blood pressures were higher than the 95th percentile. The bilateral femoral pulses were weak, and blood pressures could not be measured on his lower limbs. The remainder of the examination was unremarkable. There was no sign of primary hypertension during the clinical and laboratory evaluations.
On chest X-ray, the mediastinum was normal, and the cardiothoracic index was within normal limits. Twelve-lead resting ECG revealed left ventricular hypertrophy.
Renal ultrasonography revealed increased grade-1 echogenicity in both kidneys. Doppler USG revealed markedly low perfusion in the renal artery intrarenal segments, and resistive index values were measured in the range of 0.4–0.6. However, peak systolic velocity was found to be increased in the renal artery (peak systolic velocity: 55–56 cm/s) and abdominal aorta (peak systolic velocity: 400 cm/s).
On echocardiographic examination, the left ventricle size and functions were normal, there was no stenosis in the aortic valve, but the structure was bicuspid. Aortic arch was unobstructed and laminar flow was observed. A 10-mmHg gradient without extension to diastole was obtained with Doppler.
Ambulatory blood pressure was measured for 24 hours and presented high blood pressure values during the day (151/70/93 mmHg) and night (154/70/94 mmHg), despite using antihypertensive treatment. To determine the aetiology of hypertension and to evaluate the operated coarctation area, CT angiography was performed as a next step. The graft and the native aorta were observed in the coarctation area. Lumen was patent. In this process, the diameter of the native aorta was measured as 5 mm. CT angiography also showed a diffuse severe narrowing of the distal thoracic and proximal abdominal aorta up to the infrarenal level (Fig 1a). A narrowing was observed at the proximal level of the right renal artery.
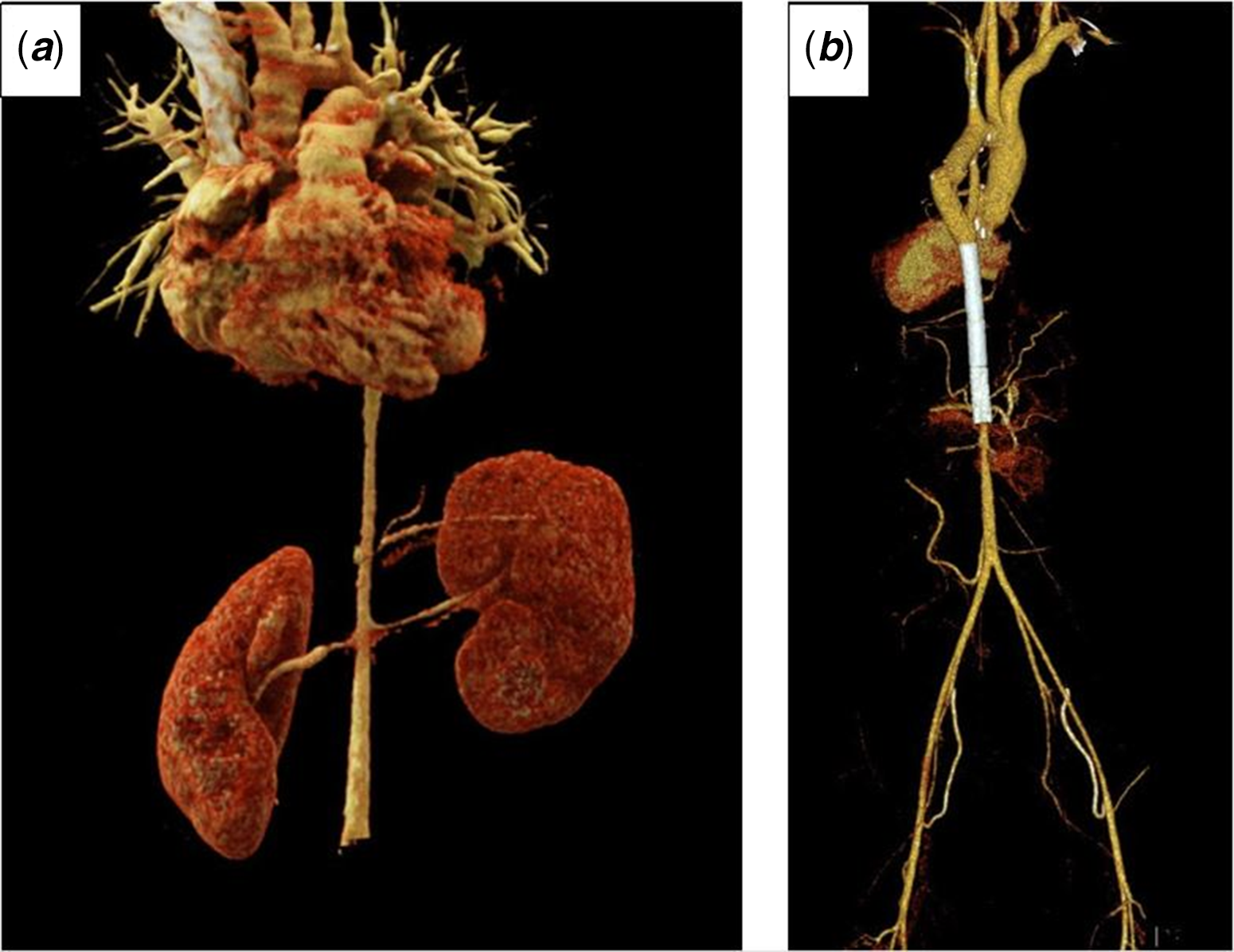
Figure 1. CT angiography with 3D reconstruction images of the patient before ( a ) and after ( b ) stent implantation.
These findings were diagnostic for midaortic syndrome. Because of her uncontrollable hypertension despite maximum medical therapy, invasive intervention was advised.
Procedure
Cardiac catheterisation was performed under general anaesthesia. The angiographic study revealed that the descending aorta in the middle aortic segment was hypoplastic with a calibration of 5.5–6 mm (Fig 2a). Besides, hypoplasia was observed in the proximal part of the right renal artery. Before stent implantation, to safely advance the long sheath, a predilatation was performed using a 5 × 2 cm Tyshak II balloon. After then, a 40x9 mm Cook Formula stent was gradually inflated. Later, a 40 × 9 mm second Cook Formula stent was partially overlapped with the first and gradually inflated. As it was noticed that there was a pressure gradient in the distal part of the stents, a 7 × 58 mm stent was inflated gradually in overlap. Control angiography demonstrated good position of the stents with aortic final diameter of 9 mm, and maximum gradient of 15 mmHg remained between the ascending and descending aorta.
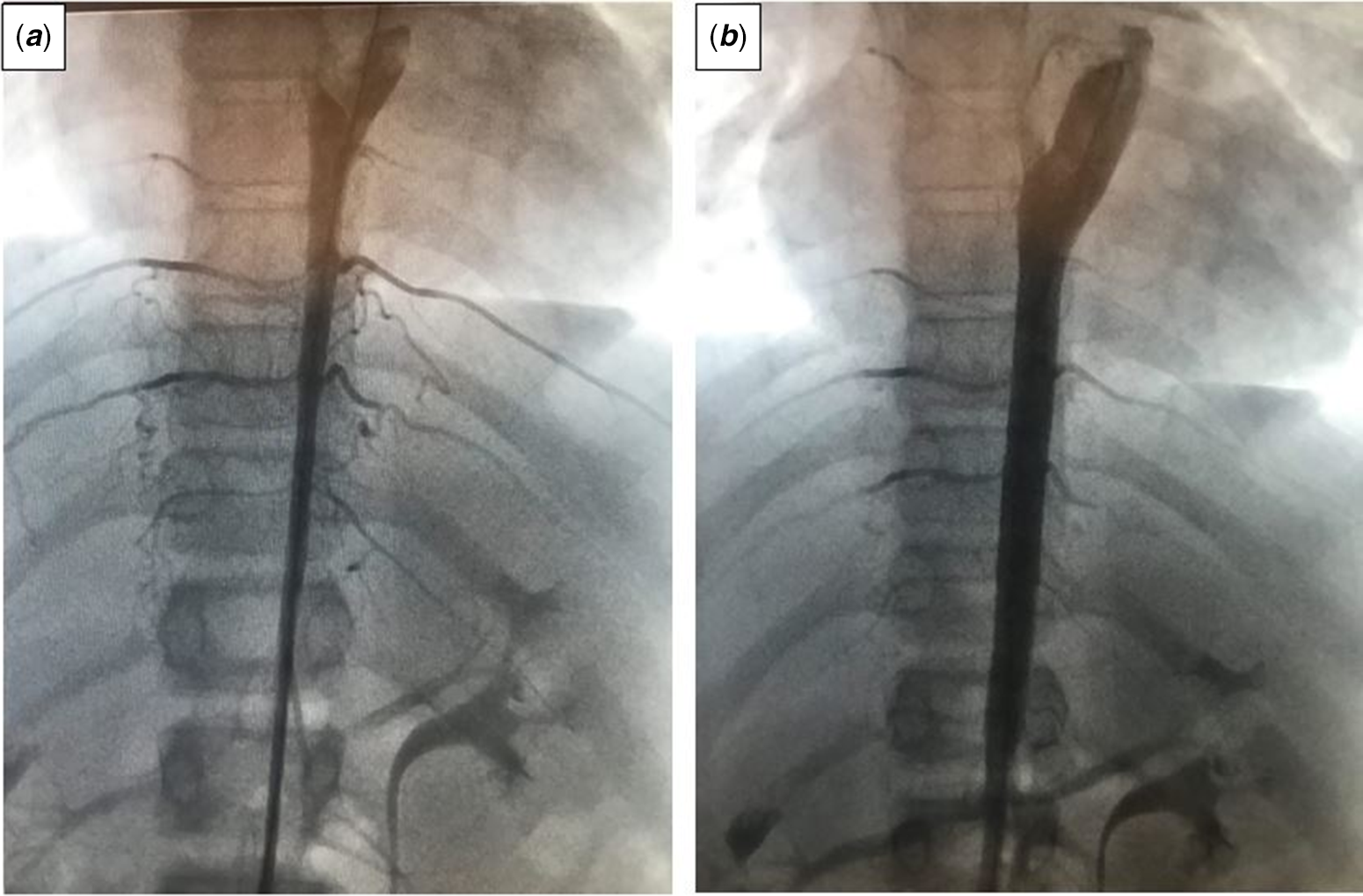
Figure 2. Catheter angiography images of the patient before ( a ) and after ( b ) stent implantation.
After the procedure, the patient’s hypertension regressed. CT scan revealed (Fig 1b and b) a short part of the distal abdominal aorta still hypoplastic. One year after the procedure, the patient did not complain of any symptoms, and her blood pressure remained normal.
Discussion
Narrowing of the abdominal aorta was first identified by Quain in 1848, but the term “middle aortic syndrome” was created by Sen et al.Reference Sen, Kinare, Engineer and Parulkar4 in 1963 after observing 16 patients with Takayasu’s arteritis and active tuberculosis. Now, the term “midaortic syndrome” refers to all obstructive lesions of the midaorta, regardless of their cause.
As with aortic coarctation, high upper extremity blood pressure, low lower extremity blood pressure, and weak femoral pulses are common clinical findings. Hypertension has been detected in nearly every case. In our patient, on physical examination, blood pressure was high in the upper extremities and both femoral pulses were weak.
Severe middle aortic syndrome causes major morbidity and mortality. Approximately half of untreated middle aortic syndrome cases lead to hypertensive encephalopathy, congestive heart failure, and stroke, which have less than 20% survival after age 40. The management of middle aortic syndrome is challenging, and it necessitates a multidisciplinary approach. Medical management of hypertension has been generally ineffective.Reference D’Souza, Tsai and Silver5 In order to achieve sufficient blood pressure management and reverse or avoid end-organ damage, invasive intervention is often required. In addition, studies have shown that symptoms such as intestinal ischemia and claudication develop more frequently in patients who received only antihypertensive treatment than those who undergo invasive treatment, but medical treatment is recommended for the stabilisation of the patient before intervention.Reference D’Souza, Tsai and Silver5
Surgical and endovascular procedures are the two forms of invasive interventions. Surgical treatment is the oldest, most common, and well-known technique. Thoracoabdominal aortic bypass, interposition aortic graft, and patch angioplasty are the most using surgical options for middle aortic syndrome. Even though many surgical studies report excellent clinical outcomes, surgery is technically difficult with more potential risks as opposed to percutaneous interventional approaches. Surgical bypass using conduits is hard and complicated, and the tube graft will need to be replaced later, particularly if the patient has not reached full growth at the time of the initial surgical treatment.Reference Kim, Vakili and Ramos-Gonzalez6 For this reason, the surgical procedure requires frequent repetitions in children.
Interventional endovascular therapy consists of balloon dilatation or stent implantation. Balloon angioplasty seemed initially as an acceptable alternative treatment to surgery because it was less invasive and required short hospitalisation, but it is limited by unsatisfactory results due to significant vessel recoil, especially in hypoplastic and fibrotic stenoses.Reference Bush, Hoffman, Del Rosario, Eiriksson and Rome7 To get over these limitations, endovascular stents, including different types of balloon-expandable and self-expanding stents, were applied by and by in the management of middle aortic syndrome.Reference O’Laughlin, Perry, Lock and Mullins8
The optimum stent to be used in middle aortic syndrome should be able to be delivered through small sheaths, be flexible, redilatable up to 15–18 mm maximum size, have little shortening, and have good radial strength, among other characteristics.Reference Quandt, Ramchandani and Bhole9 Due to their limited radial strength, self-expanding stents cannot be overdilated and hence do not meet the criteria.Reference Redington, Weil, Somerville and Br Heart10 Balloon-expandable stents are commonly used stents in paediatric cardiology. Coronary balloon-expandable stents are extremely flexible and may be inserted using 4F sheaths or 6F guide catheters, but they cannot be extended beyond 6 or 7 mm in diameter. These limitations have resulted in the creation of novel stent designs.
The Cook Formula stent family is a relatively new hybrid cell design that has been approved for use in biliary, renal, and peripheral vascular procedures. The major advantage of Cook stent is that while other Balloon-expandable stents length can vary by up to 53% during dilatation, Cook stent’s length changes minimally even as its diameter increases.Reference Quandt, Ramchandani and Bhole9 This provides the opportunity to perform stent redilatation over time, especially in children who have not completed their development.
In our patient, no intervention was performed on the narrowing at the proximal level of the right renal artery. We decided against it because of the significant risk of restenosis, which has been reported in approximately 20–26% of childrenReference Srinivasan, Krishnamurthy and Fontalvo-Herazo11, as well as other problems. Because the patient’s blood pressure can be regulated, a surgical treatment may be performed after the patient’s growth and development is complete.
In conclusion, middle aortic syndrome is utterly a severe form of aortic coarctation and leads intractable hypertension and end-organ failure. Because surgical approach has several limitations and risks of reoperation, transcatheter endovascular stent implantation should be kept in mind as a feasible alternative treatment. This could be anyway a good example of effective stenting implantation with a relatively new hybrid stent family that provides the opportunity to perform stent redilatation over time. Because of well-known high incidence of restenosis and reintervention after percutaneous intervention, follow-up is needed with this new type of stent.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.





