Introduction
Major depressive disorder (MDD) is a major global public health problem. It is a common mental disorder in the general population, characterised by depressed mood, loss of interest or pleasure, feelings of guilt or low self-worth, disturbed sleep or appetite, feelings of tiredness and poor concentration (World Health Organization, 2018). It is estimated that depression affects more than 300 million individuals, with a point prevalence of about 5% and a lifetime prevalence of 15% worldwide, making it one of the leading causes of disability (Friedrich, Reference Friedrich2017). Depression is a complex disorder which occurrence is explained by the interplay between genetic and environmental factors (Lohoff, Reference Lohoff2010; Tafet and Nemeroff, Reference Tafet and Nemeroff2016), with multiple small-effect genes involved in complex relationships with psychosocial environmental factors (Whalley et al., Reference Whalley, Hall, Romaniuk, Macdonald, Lawrie, Sussmann and McIntosh2015). While genetic studies suggest that genetic factors can account for about 30% of the variance in depression (Henn and Vollmayr, Reference Henn and Vollmayr2005), actual genome-wide analyses of multiple candidate genetic polymorphisms - polygenic risk score, only explained 1.9% of the variance in the risk for MDD (Wray et al., Reference Wray, Ripke, Mattheisen, Trzaskowski, Byrne, Abdellaoui, Adams, Agerbo, Air and Andlauer2018). In contrast, psychosocial environmental factors appear to play a much larger role in the development of MDD (Cohen et al., Reference Cohen, Janicki-Deverts and Miller2007). Psychosocial stressors, especially early traumatic events and stressful life events have been shown to play an important role in the aetiology of MDD (Tennant, Reference Tennant2002; Su et al., Reference Su, D'Arcy and Meng2021). These stressors can interact with a genetic vulnerability to modify brain chemistry and impact mental health (Loman and Gunnar, Reference Loman and Gunnar2010).
Lifetime stressors refer to a total sum of various types of early and later-on stressors that a person has experienced over the lifespan, with each form having potentially different consequences for health (Slavich, Reference Slavich2016; Shields and Slavich, Reference Shields and Slavich2017). Of note, early life stress (ELS) has a powerful impact on the growth and development of an individual (Seng et al., Reference Seng, Sperlich, Low, Ronis, Muzik and Liberzon2013; Su et al., Reference Su, D'Arcy and Meng2021). ELS was defined as the exposure to events that happened in early life, a sensitive and vulnerable period and such stressors may exceed a child's ability to cope (Pechtel and Pizzagalli, Reference Pechtel and Pizzagalli2011). Commonly studied early life stressors include physical, sexual, emotional abuse, neglect, poor child–parent bonding, social deprivation and household dysfunctions, etc. (Brown et al., Reference Brown, Anda, Tiemeier, Felitti, Edwards, Croft and Giles2009). The stress sensitisation model hypothesises that early adverse events can enhance later-on stress responsiveness in adulthood and lower the threshold for adverse stress reactions later in life. The relationship of later life adult stressors and adverse health outcomes is, in part, determined by earlier exposure to childhood adversity (Keyes et al., Reference Keyes, Hatzenbuehler and Hasin2011; Keyes et al., Reference Keyes, McLaughlin, Koenen, Goldmann, Uddin and Galea2012). Life events in adulthood, which are commonly distinguished into early life events to which a role of predisposing factors is assigned, also contribute to the likelihood of mental disorders (Heim et al., Reference Heim, Newport, Wagner, Wilcox, Miller and Nemeroff2002; Faravelli et al., Reference Faravelli, Catena, Scarpato and Ricca2007). Although psychosocial stress is a strong risk factor for disease, not all people with stressful experiences are affected negatively and develop psychiatric disorders. The diathesis-stress model proposed that stressful experiences across the lifespan trigger illnesses with varying degrees of vulnerability in biological and psychosocial characteristics and circumstances (National Research Council, 2009; Smoller, Reference Smoller2016).
Based on the life course perspective and stress process theory, early-life stressful circumstances (i.e. childhood maltreatment, poor child–parent bonding) are seen to lead to non-normative adverse depression trajectories (Wickrama et al., Reference Wickrama, Conger and Todd Abraham2008). Additionally, exposure to stressors during later adult life is also significantly associated with increased mental health problems (Romanov et al., Reference Romanov, Varjonen, Kaprio and Koskenvuo2003). Accumulation of risks across the lifespan can act as a cumulative, aetiologic threat to persistent health problems (Kuh et al., Reference Kuh, Ben-Shlomo, Lynch, Hallqvist and Power2003). A growing body of research has documented that psychosocial stressors can have a cumulative effect thus increasing the likelihood of mental illnesses (Raviv et al., Reference Raviv, Taussig, Culhane and Garrido2010; Björkenstam et al., Reference Björkenstam, Burström, Brännström, Vinnerljung, Björkenstam and Pebley2015). Extension to the cumulative risk model specifies that such effects will depend on sub-population categories and the diverse patterns of risk factors (Roberts et al., Reference Roberts, English, Thompson and White2018). In the chain of risk model, stressful events may co-occur and exposure to multiple stressors may reflect an interrelated pattern as stressors across lifespan tend to occur in clusters, rather than as single events or experiences (Steel et al., Reference Steel, Silove, Bird, McGorry and Mohan1999; Rees et al., Reference Rees, Silove, Chey, Ivancic, Steel, Creamer, Teesson, Bryant, McFarlane and Mills2011). Unfortunately, most studies are limited in examining the co-occurrence of environmental stressors throughout the life course, this points to the importance of parcelling out different patterns of stress that occur. Investigations taking the timing of stressors or specific differences by sub-population into account are needed to capture the complexity of the association between lifetime psychosocial stressors and MDD.
Given the increasing recognition of such limitations in stress research, an alternative approach of operationalising lifetime psychosocial stressors clusters them with regard to stressful exposures. This approach may be more informative in examining their associations with depression. Person-centred methods [e.g. latent profile analysis (LPA)] overcome the limitations of the variable-centred approaches. Variable-centred approaches assume that the population to be homogeneous and overlook diversity within studied populations, whereas person-centred approaches provide multifaceted information about stress sorting individuals into mutually exclusive classes that maximise between-group variance and minimise within-group variance (Adams et al., Reference Adams, Ding, Sallis, Bowles, Ainsworth, Bergman, Bull, Carr, Craig and De Bourdeaudhuij2013). It thus reveals the heterogeneity in the within-person configuration with multiple forms of stress. It also reveals how adult psychopathology varied across groups with distinctive patterns emerging (Howard and Hoffman, Reference Howard and Hoffman2018). This person-centred approach adds to the literature by identifying naturally occurring clusters of individuals with similar patterns of stressors.
Even though studies suggest that cumulative lifetime stress is associated with the increased risk of adverse mental health outcomes, there are inconsistent findings in terms of dose–response relationships between stressors and mental health and wellbeing (Seery et al., Reference Seery, Holman and Silver2010; Toussaint et al., Reference Toussaint, Shields, Dorn and Slavich2016; Hubbard et al., Reference Hubbard, Reohr, Tolcher and Downs2018). For instance, exposure to a moderate level of stress can predict better mental health and well-being than either exposure to a high level of stress or no stress (Seery et al., Reference Seery, Holman and Silver2010). This inconsistency may be explained by stressful events across the lifespan that may foster subsequent resilience promoting positive mental health and wellbeing (Seery et al., Reference Seery, Holman and Silver2010). The amount and kinds of stressors that pose mental problems have not been clearly established and are currently insufficient to inform specific public health policy. To the best of our knowledge, no study has been published to explore a life course perspective of different patterns and cumulative effects of life stressors in the development of MDD based on a comprehensive model of biological and psychological attributes. The biopsychosocial model proposed by Engel acts as a guiding theoretical framework identifying the importance of biological and psychosocial attributes in the development of depression (Schotte et al., Reference Schotte, Van Den Bossche, De Doncker, Claes and Cosyns2006). However, there is a paucity of research that estimates the associations between lifetime psychosocial stressors and MDD while taking biological (genetic) factors into account. A comprehensive examination of biopsychosocial factors can contribute substantially to our understanding of the pathogenesis of MDD.
A life-course perspective of stressors in the context of a biopsychosocial model could help illustrate stressors as chains of risks in which the early life origins of cumulative stress patterns have an aggregated impact on health outcomes. Building on these frameworks and expanding this literature by studying various profiles of lifetime stressors, the aims of our present study are to (1) examine the individual roles of specific stressors (i.e. childhood maltreatment, parent–child relationship and stressful life events) in the development of subsequent MDD; (2) test the cumulative effects of different trajectories of the lifetime stressors across the lifespan in the development of MDD; (3) explore whether latent profiles of psychosocial stressors are associated with subsequent MDD. In testing these stress hypotheses, we take into account genetic predispositions, sociodemographic characteristics (age, sex, marital status, ethnicity, education and income) and health-related characteristics (type of drinkers, self-perceived mental health and family history of mental disorders) in the analysis. A schematic diagram of a biopsychosocial model of the stress-depression process used in the study is shown in Fig. 1.
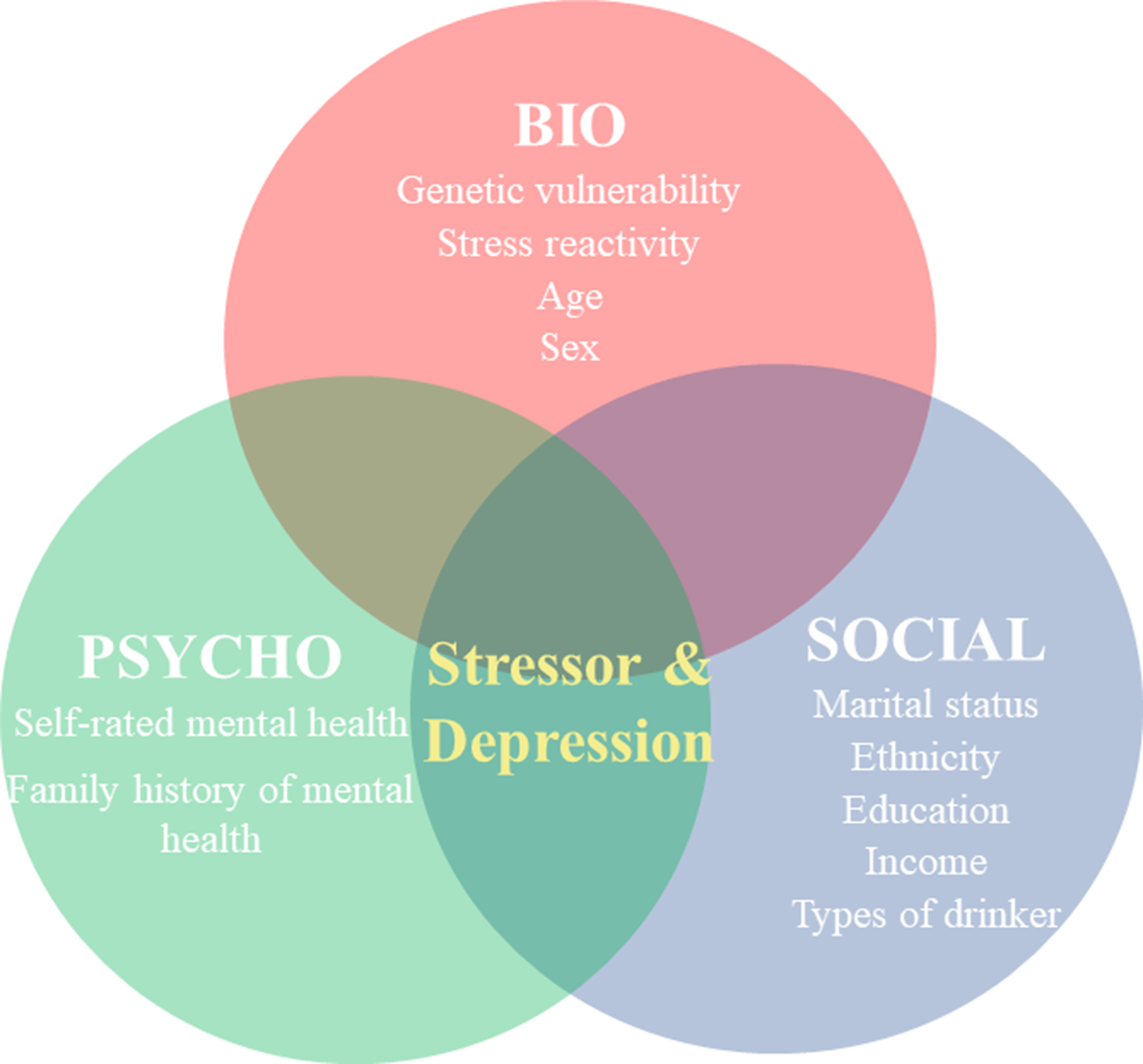
Fig. 1. Biopsychosocial model of stress and depression.
Methods
Study sample
The current study used data from the Social and Psychiatric Epidemiology Catchment Area Study of Southwest Montreal (ZEPSOM). The ZEPSOM cohort is a longitudinal, community-based cohort. The cohort is a random sample of area residents between 15 and 65 years of age representing a total of 269 720 inhabitants across five neighbourhoods in southwest Montreal in 2007. At baseline data collection (Wave 1), the sample consisted of 2433 randomly selected participants. More details about the study can be found in the previous research (Caron et al., Reference Caron, Fleury, Perreault, Crocker, Tremblay, Tousignant, Kestens, Cargo and Daniel2012). The present study sample (N = 1351) is restricted to those respondents who completed their interviews at Wave 3, Wave 4 and Wave 5 of the study and had information on depression status at Wave 4, stressful events at Wave 3, early life experiences at Wave 5 and genetic sequencing data at Wave 5. Online Supplementary Fig. S1 illustrates the selection process of the present study.
Measurements
Lifetime stress measurements
Childhood maltreatment. Childhood maltreatment was assessed using the Childhood Trauma Questionnaire-short form (Bernstein and Fink, Reference Bernstein and Fink1998). It has 28 self-reported items assessing childhood abuse and neglect and can be administered to anyone 12 years or older. The Cronbach's alpha value for this study was 0.98.
Parental bonding. Parental bonding was assessed using the Parental Bonding Instrument (PBI), which is a 50-item questionnaire designed to measure perceptions of parental behaviours before the age of 16 (Parker et al., Reference Parker, Tupling and Brown1979). The questionnaire has two subscales including 12 items assessing the dimension of care and 13 items assessing control and overprotection for maternal and paternal bonding, respectively. To be consistent for both the care and control/overprotection subscales of the PBI, we reversed the scores of scale items in the care dimension, thus, a high score on the care subscale indicates more perceived parental neglect and rejection. Similarly, a high score on the overprotection subscale indicates perceived excessive control and intrusive parenting. The Cronbach's alpha value was 0.89 for the maternal care scale and 0.93 for the paternal care scale and 0.84 for both maternal and paternal protection subscale.
Stressful life events. The Life's Events Questionnaire was used to measure the stressful life events (Laurin, Reference Laurin1998). The instrument includes a total of 22 life events that can be grouped into five major themes, including work and financial issues, romantic relationships, family and friend relationships, housing and experiences of aggression. Responses were measured on a 4-point Likert scale (1 = ‘not stressful’, 2 = ‘a little stressful’, 3 = ‘quite stressful’, 4 = ‘very stressful’). The Cronbach's alpha for the scale was 0.58.
Lifetime major depression
Major depression was assessed based on the modified version of the World Mental Health (WMH) 2000 project, an international initiative responsible for the development of a newer version of the Composite International Diagnostic Interview (CIDI). The WMH-CIDI is a fully structured diagnostic interview assessing major depression using the definitions and criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) and the International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10) (World Health Organization, 1992; American Psychiatric Association, 2000). This modified WMH-CIDI was previously used in the Canadian Community Health Survey (CCHS cycle 1.2) (Gravel and Béland, Reference Gravel and Béland2005). These modifications of the WMH-CIDI were applied to reduce response burden and to clarify concepts (Kessler et al., Reference Kessler, Andrews, Mroczek, Ustun and Wittchen1998). Respondents were assessed for their lifetime depressive episodes prior to the diagnostic interview that occurred at Wave 4.
Covariates
Genetic predisposition-polygenic risk score
Genetic data were collected for each survey respondent at Wave 5. Polygenic risk score (PRS) is a method of aggregation conceptualised as an indicator of the diathesis used to test the predictive power of multiple genetic variants simultaneously (The International Schizophrenia Consortium, 2009). Genetic liability is captured and characterised in a GWAS or meta-analysis by creating a summary score of weighted effect sizes across all single-nucleotide polymorphisms (SNPs) associated with psychiatric disorders at a pre-specified significance threshold (The International Schizophrenia Consortium, 2009). For the present study, the polygenic risk score for major depression was produced using the GWAS summary statistics of per SNPs from the Psychiatric Genomics Consortium (PGC) with the p-value threshold of 0.001. PRSDEP was calculated for each participant.
Sociodemographic characteristics
Data on socio-demographic attributes were collected using standard Statistics Canada question items. Information on participants' sex (Male v. Female), marital status (Single, Married/Common-law and Separated/Divorced/Widowed), ethnicity (White v. Non-White), level of education (Less than secondary, Secondary education and Post-secondary education), and income which was treated as a continuous variable, was collected at Wave 3. Age was categorised into four groups: 18–30 years, 30–45 years, 45–60 years and 60 years and above.
Health-related characteristics
Health-related characteristics were also collected at Wave 3, including the type of drinker (Regular drinker, Occasional drinker, Former drinker and Abstainer), self-perceived mental health (Excellent, Very Good, Good, Fair and Poor) and family history of mental disorders (Yes v. No). A family history of mental disorders was asked if a biological parent, or both, had been diagnosed by a psychiatrist, or hospitalised for mental health problems, or experienced any of the following problems, including depression, delirium or hallucination, anxiety disorders, substance abuse or suicide (Sobel, Reference Sobel1985).
Statistical analysis
Operationalisation of lifetime stressors
Three approaches were used to measure lifetime stressors: (1) treating stressors as separate events, (2) aggregating stressful exposures by a composite score and (3) delineating different profiles of stressful experiences. To test and compare the strengths of associations between three different approaches of lifetime stressors and subsequent depression, we conducted separate analyses for all three approaches. First, each specific stressor (including childhood maltreatment, parent–child bonding and stressful life events) was considered individually. Second, a composite score of cumulative stress index was created by combining three stress domain measures. Childhood maltreatment, parent–child bonding and stressful life events were standardised to a z-score. A continuous cumulative stress score was then calculated by adding the standardised scores of these three domains. Higher scores of the cumulative stress index indicate more cumulative stressors experienced. Third, LPA was used to create a more comprehensive measurement of the lifetime stressors by combining individual stressors into mutually exclusive latent profiles. LPA is a robust statistical technique, commonly employed to identify subtypes of homogeneous latent classes or subgroups based on data from continuous indicator variables (Garrett and Zeger, Reference Garrett and Zeger2000). LPA is analogous to latent class analysis (LCA) but can be used for continuous and ordinal predictors with several values. Additionally, LPA is a superior mixture-model technique compared to the traditional methods of cluster analysis (DiStefano and Kamphaus, Reference DiStefano and Kamphaus2006). Maximum likelihood estimation procedure was used with 95% CI, calculated via 1000 non-parametric bootstrap. The analysis started with the most parsimonious 1-profile model, additional profiles were added. A different number of profiles were tested subsequently to identify the optimal profile solution. The optimal number of profiles was determined by Bayesian information criterion (BIC), Akaike information criterion (AIC) and the sample size adjusted BIC (ssaBIC) (Schwarz, Reference Schwarz1978; Akaike, Reference Akaike1987; Sclove, Reference Sclove1987). Lower values indicate a better model fit. The entropy criterion was also examined, which indicates how accurate participants are classified into respective profiles, with higher values indicating a better fit (Aldridge and Roesch, Reference Aldridge and Roesch2008). The bootstrap likelihood-ratio (BLR) test was performed to compare a K class model with a K-1 class model, a significant BLR test indicates that the model with K class is optimal (Arminger et al., Reference Arminger, Stein and Wittenberg1999). Hence, the best class solution should have lower BIC, AIC, ssaBIC values, but a higher entropy value and a significant BLR p-value. In addition, the complete case analysis was conducted as a sensitivity analysis to assess to what extent the missing values would influence the result findings. We conducted the LPA analysis for those participants who completed information on stress measurements.
Associations between psychosocial stressors and depression
Firstly, to test hypotheses assessing basic relationships between studied variables, we conducted Pearson correlation analyses between predictor and outcome variables. Then, multivariate logistic regression was conducted to determine whether there were significant associations between the three methods of assessing lifetime stressors and subsequent depression. Two sets of models were fitted for each stress approach: (a) a crude or unadjusted model and (b) adjusted for genetic factors (PRSDEP), sociodemographic covariates (age, sex, marital status, ethnicity, education and income) and health-related characteristics (type of drinker, self-perceived mental health and family history of mental disorders). These variables were controlled to exclude their potential confounding effects in the associations between lifetime stressors and MDD.
Overall, the missing rate for each variable was less than 15%. We conducted multiple imputations by chained equations using the fully conditional specification method under the missing-at-random assumption (Royston, Reference Royston2009). Ten imputed datasets were generated from multivariate linear and logistic regression models using age and sex as potential predictors. Then one single pooled parameter estimate for each analysis was obtained based on Rubin's (Reference Rubin1987) rule which took into consideration the variance within and between imputations. Statistical significance for all analyses was set at p < 0.05 (by two-tailed test). In addition, we used maximisation likelihood estimation in the LPA to deal with the missing values. Descriptive statistics, Cronbach's alphas, Pearson's correlation coefficients between all variables, and regression analyses were conducted in Stata, version 15, and the LPA was conducted using Mplus, version 8.
Results
A summary of the study cohort
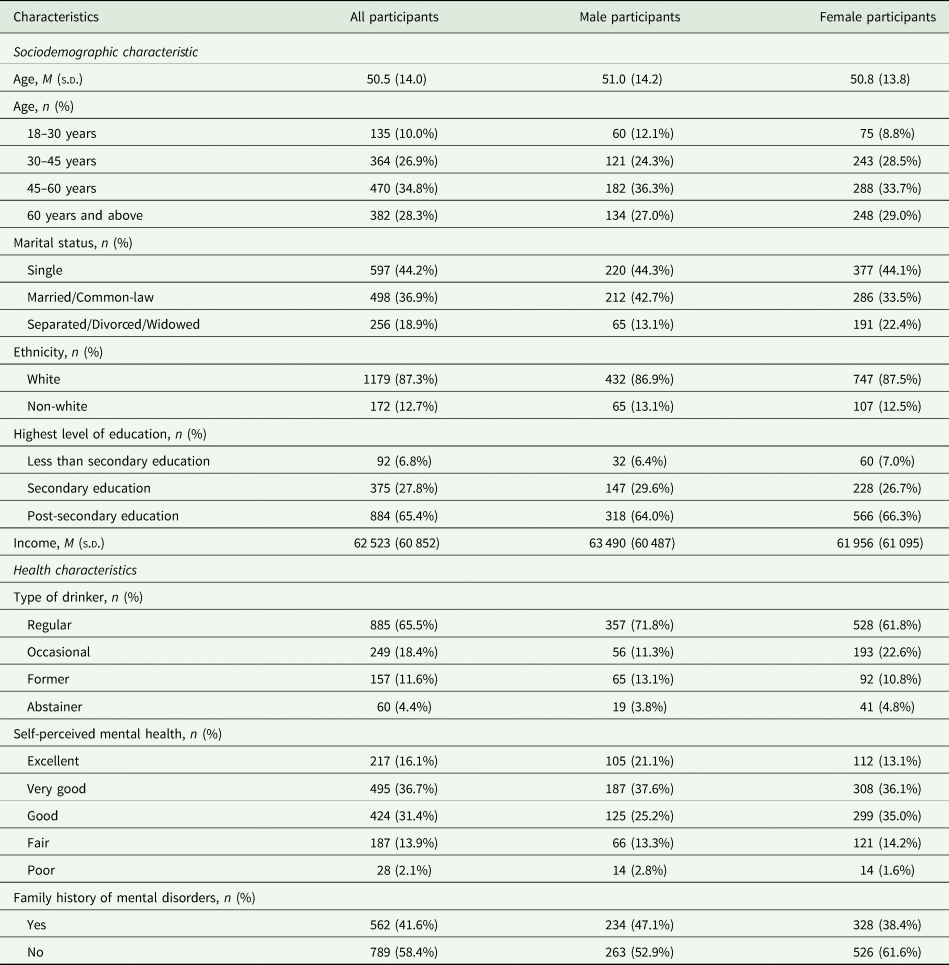
Table 1 shows a detailed description of the study cohort. The present study included a total of 1351 subjects who completed five data collections. The study sample included 36.8% males, 44.2% single, 87.3% White and 65.4% participants having a post-secondary education. The mean age of the sample was 50.5 years (s.d. 14.0). The mean annual family income was $ 62 523, and male participants earned more on average than female participants. About two-thirds of the study sample reported being a regular drinker with more males than females reporting regular drinking (71.8% v. 61.8%). Approximately one-third (36.7%) reported their self-perceived mental health as good. Male participants were slightly more likely to report having good self-perceived mental health than female participants (37.6% v. 36.1%). In addition, 47.1% of males and 38.4% of females reported a family history of mental disorders.
Table 1. Description of the study sample
We conducted correlation analyses for different stress exposures. Table 2 shows that strong zero-order correlations were observed within different subtypes of childhood maltreatment and correlations were more heterogeneous in magnitude between the other two assessed stressors (parental bonding and stressful events). All different approaches of stress assessments (including specific stressors, cumulative stressors and different patterns of stressors) were associated with the increased risk of subsequent depression.
Table 2. Correlations among individual psychosocial stressor, cumulative stressor, patterns of stressors, polygenetic risk factors and lifetime depression
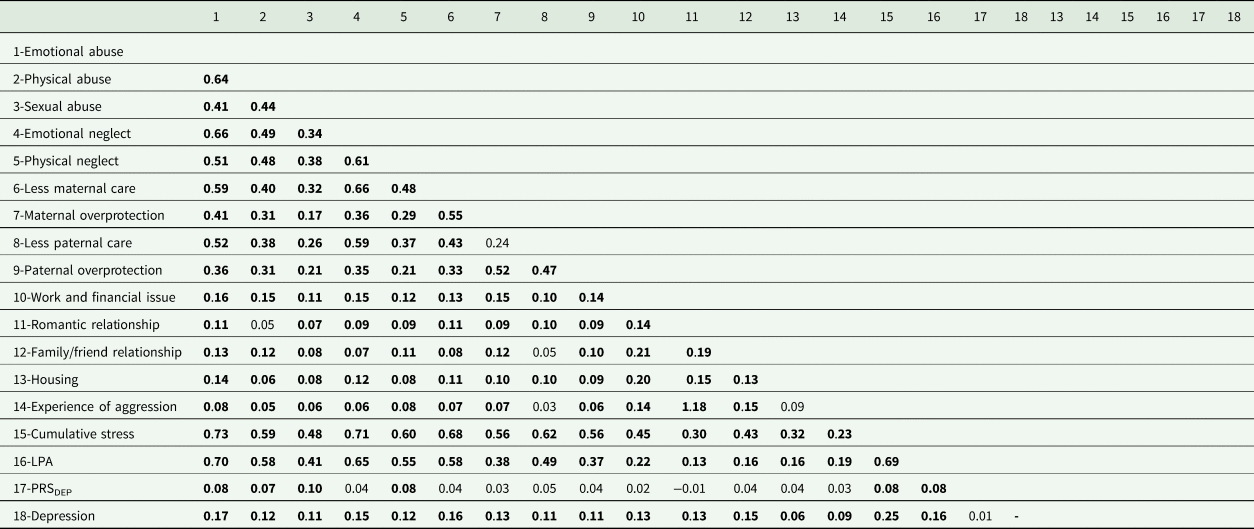
LPA, latent profile analysis; PRSDEP, polygenic risk score for depression.
Bold font indicates statistical significance, p < 0.05 (2-tailed).
Latent profile analysis
Table 3 presents the model fit indices for all the latent profile models examined. AIC, BIC and ssaBIC decreased as the number of profiles increased. Because the p-value of the log-likelihood test showed no statistical significance between the 3-profile model and the 4-profile model, the model specification did not improve from the 3- profile model to the 4- profile model. The 3-profile model had a higher entropy value than the 4-profile model and was easier to illustrate, therefore we decided to take the 3-profile model as the best fitting parsimonious model.
Table 3. LPA fit indices for a one-class, two-class, three-class and four-class solution for the childhood maltreatment, child–parent bonding and stressful life events dimensions
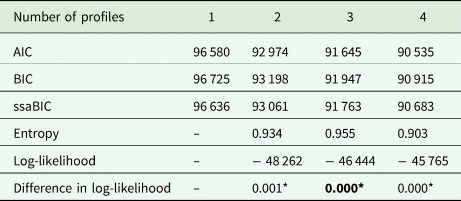
AIC, Akaike's information criteria; BIC, Bayesian information criteria; ssaBIC, the sample size adjusted Bayesian information criteria.
*indicates statistical significance, p < 0.05 (2-tailed).
Figure 2 provides visual illustrations of the mean scores for all of the selected lifetime stressors among the three identified stressor profiles. As shown in Fig. 2, profile 1 was the most prevalent profile (N = 1015, 75.1%). Participants in this profile reported a low level of stress across their lifespan and were labelled as the ‘low stress’ group. Individuals in profile 2 (N = 92, 6.8%) and profile 3 (N = 244, 18.1%) included those who had scores that fell within the moderate and high levels of childhood maltreatment, adverse child–parent bonding and stressful life events. Profiles 2 & 3 reported above-average stress levels thus were labelled as moderate- and high-stress groups, respectively.
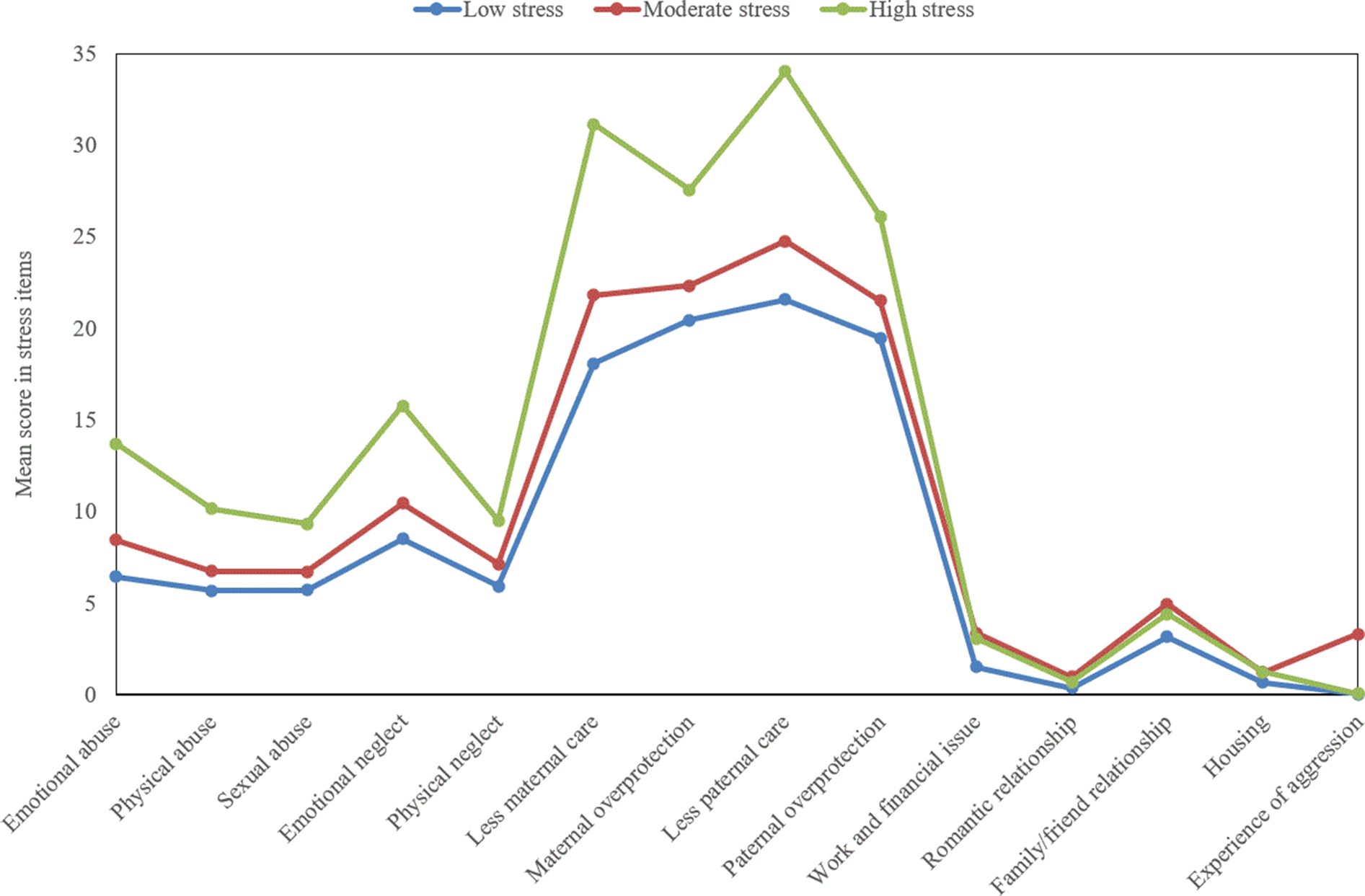
Fig. 2. The latent profiles based on childhood maltreatment, child–parent bonding and stressful events.
Exploring specific and cumulative stressors in associations with depression
Table 4 shows unadjusted and adjusted associations between stressors and the risk of depression. For specific stressors, we found that people with emotional abuse/neglect, the experience of lack of parental/maternal care and having the stress related to family/friend relationships, were more likely to report depression. After adjusting for genetic factors (PRSDEP), sociodemographic covariates (age, sex, marital status, ethnicity, education and income) and health-related characteristics (type of drinker, self-perceived mental health and family history of mental disorders), for the domain of childhood maltreatment, emotional abuse (OR = 1.25, 95% CI: 1.09–1.43), physical abuse (OR = 1.20, 95% CI: 1.05–1.38), sexual abuse (OR = 1.16, 95% CI: 1.02–1.33), emotional neglect (OR = 1.22, 95% CI: 1.06–1.41) and physical neglect (OR = 1.19, 95% CI: 1.04–1.37) were significantly associated with depression. Concerning child–parent bonding, parental over-control (ORMaternal = 1.21, 95% CI: 1.05–1.39; ORPaternal = 1.20, 95% CI: 1.04–1.39) and lack of parental care (ORMaternal = 1.24, 95% CI: 1.09–1.44; ORPaternal = 1.26, 95% CI: 1.10–1.45) were all associated with depression. Similarly, except for housing-related stress, other four constructs including stressful events related to work and financial issues (OR = 1.18, 95% CI: 1.03–1.36), romantic relationship (OR = 1.15, 95% CI: 1.01–1.32), family/friend relationship (OR = 1.30, 95% CI: 1.13–1.50) and experience of aggression (OR = 1.15, 95% CI: 1.00–1.31) were associated with depression.
Table 4. Associations between psychosocial stress measures and depression – individual psychosocial stress, cumulative psychosocial stress and LPA-derived psychosocial stress clusters
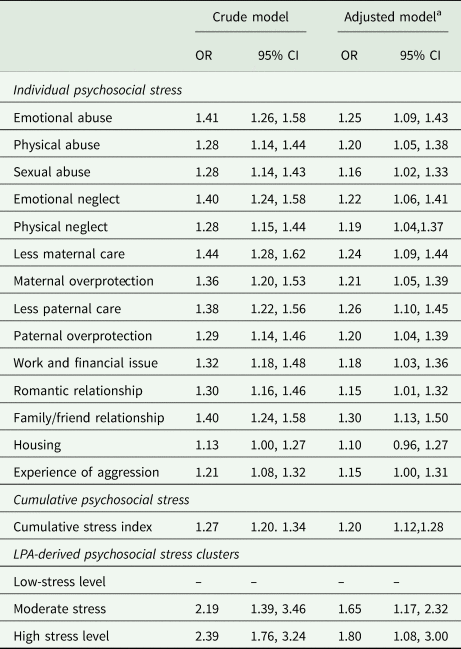
LPA, latent profile analysis; OR, odds ratio; 95% CI, 95% confidence interval.
Adjusted model a adjusted for PRS DEP, sociodemographic covariates (age, sex, marital status, ethnicity, education, income) and health-related characteristics (type of drinker, self-perceived mental health and family history of mental disorders).
For cumulative stress measurement, when controlling for genetic and sociodemographic as well as health-related characteristics, the cumulative lifetime stress index was a significant risk factor for subsequent depression (OR = 1.20, 95% CI: 1.12–1.28). For the stress patterns, while there was evidence of confounding towards the null, the statistical significance of estimates did not change between unadjusted and adjusted models. Compared to those in the low level of stress group, those in the moderate level of stress group were associated with an increased risk of depression (OR = 1.65, 95% CI: 1.17–2.32), and individuals with a high level of stress exposures were 1.80 times (95% CI: 1.08–3.00) more likely to have depression.
Sensitivity analysis
For the complete case analysis, a 3-profile solution outperformed other models, and the final three-profile solution included 77.0% of the sample with a low level of stress (N = 823), 6.6% of the sample with a moderate level of stress (N = 71) and 16.4% of the sample with a high level of stress (N = 175) (see online Supplementary Table S1). The results of complete case analysis reinforce the findings in the whole sample with the 3-profile model, which shows a dose–response relationship between lifetime stressors and the increased risk of subsequent depression.
Discussion
This study is the first study to use different approaches to articulate how lifetime stressors are associated with subsequent depression using a longitudinal community-based cohort. Our present study used both person-centred and variable-centred approaches to verify the association between lifetime stressors and subsequent depression. Lifetime stressors had a cumulative effect on the risk of subsequent depression after adjusting for genetic predispositions and other sociodemographic characteristics. Those with a high level of lifetime stressors were more likely to develop depression compared to those with a low level of lifetime stressors. The findings of the study provide additional evidence to support the diathesis-stress model in terms of the impact of lifetime stressful experiences in depression. The current study adds to the existing literature by examining both the individual effects and their collective impact. Our findings reinforce the complexity of lifetime stressful experiences in the development of depression and direct the research on individuals' heterogeneity of stress linking with different risks of depression.
There is ample evidence to explain how stress interferes with normal functioning and increases the risk of developing physical and mental health problems. Stress itself is not only caused by a specific experience happening to the individual but is also caused by a lack of resources for effectively dealing with the initial stressor that can have a cascade effect resulting in more stress (Lazarus and Folkman, Reference Lazarus and Folkman1984). Effective stress responses are integral to emotional well-being. Stress reactivity is coordinated by an interplay of the neuroendocrine system and the sympathetic nervous system. The hypothalamus–pituitary–adrenal (HPA) axis plays a key role in orchestrating bodily responses to stress, and axis activity can be modified by a wide range of experiential events. Exposures like early life adversity and adverse stressful events during life serve as general vulnerability factors that accelerate future HPA axis reactivity in ways that make individuals more sensitive to stress challenges, and therefore feed forward into the exacerbation of ongoing, or greater susceptibility towards, future stress-related disease states (Dannlowski et al., Reference Dannlowski, Stuhrmann, Beutelmann, Zwanzger, Lenzen, Grotegerd, Domschke, Hohoff, Ohrmann, Bauer, Lindner, Postert, Konrad, Arolt, Heindel, Suslow and Kugel2012; Ludwig et al., Reference Ludwig, Pasman, Nicholson, Aybek, David, Tuck, Kanaan, Roelofs, Carson and Stone2018). Epidemiological and clinical studies have provided compelling evidence for establishing the association between various early-life stressors and elevated risk of depressive disorders (Heim and Binder, Reference Heim and Binder2012; O'Mahen et al., Reference O'Mahen, Karl, Moberly and Fedock2015; Gallo et al., Reference Gallo, De Mola, Wehrmeister, Gonçalves, Kieling and Murray2017). Adverse parental bonding which captures dimensions of care and overprotection between parent and child bonding predicts the risk of depression in adulthood (Sato et al., Reference Sato, Uehara, Narita, Sakado and Fujii2000). Additionally, based on the stress sensitisation hypothesis, experiences of early adversities make people more susceptible to later-occurring stressors such as stressful life events (Hammen et al., Reference Hammen, Henry and Daley2000; Estrada-Martínez et al., Reference Estrada-Martínez, Caldwell, Bauermeister and Zimmerman2012; Hassanzadeh et al., Reference Hassanzadeh, Heidari, Feizi, Hassanzadeh Keshteli, Roohafza, Afshar and Adibi2017). Stressful life events include discrete quantifiable circumstances, such as work conflicts, financial issues and intense interpersonal relationships, which can impact psychological well-being thus increase the risk of depression (Hassanzadeh et al., Reference Hassanzadeh, Heidari, Feizi, Hassanzadeh Keshteli, Roohafza, Afshar and Adibi2017).
In the present study, we found that cumulative effects of lifetime psychosocial stressors are associated with the elevated risk of depression after controlling for genetic predispositions of depression and other psychosocial covariates. Our results are consistent with the existing literature on the relationship between cumulative psychosocial stressors and depression. An ongoing longitudinal study explored the cumulative effects of different stressors across early and middle childhood on internalising behaviours and suggested that the combined effect of multiple stressors could explain variations in internalising behaviours (Appleyard et al., Reference Appleyard, Egeland, van Dulmen and Alan Sroufe2005). Likewise, the Rochester Longitudinal Study also found that the experience of multiple stressors potentiated the development of psychopathology (Sameroff, Reference Sameroff2000). This research adds to the literature in terms of the dose–response relationship between various levels of stress and the risk of subsequent depression – those having low levels of stress across the lifespan had the lowest risk of depression. While those with moderate to high levels of childhood maltreatment, adverse child–parent bonding and stressful life events reported a higher risk of depression. Our results further support the stress sensitisation theory, which conceptualised stressors become increasingly capable of triggering depressive symptoms (Hammen et al., Reference Hammen, Henry and Daley2000). Similarly, prior research also showed that stress sensitisation of depressive disorders was found at high levels of adult stressful events (Kendler et al., Reference Kendler, Kuhn and Prescott2004; Espejo et al., Reference Espejo, Hammen, Connolly, Brennan, Najman and Bor2007; McLaughlin et al., Reference McLaughlin, Conron, Koenen and Gilman2010).
We also examined how specific stressors across lifetime influenced the risk of depression after controlling for genetic predispositions and other covariates. We found that different early-life stressors including childhood maltreatment and poor parental bonding were associated with an increased risk of depression after controlling for PRSDEP. Additionally, except for the major theme on housing, other subtypes of stressful events predicted a higher risk of depression. Although a wide range of stressors has demonstrated stress sensitisation with the risk of depression, stress-related to family, for instance, less parental care and childhood emotional maltreatment had a stronger independent impact on depression. Our study findings are consistent with a UK longitudinal cohort study which found that individuals with early adversity experience were more likely to report psychotic symptoms when controlling for genetic vulnerability to psychosis (Arseneault et al., Reference Arseneault, Cannon, Fisher, Polanczyk, Moffitt and Caspi2011). Similarly, Musliner et al. (Reference Musliner, Seifuddin, Judy, Pirooznia, Goes and Zandi2015) found that stressful life events were significantly and independently associated with depressive symptoms when disentangling the effects of polygenic risk.
The learned helplessness paradigms and chronic mild stress are two common depressive animal models used to delineate the pathogenesis of depression considering both genetic and psychosocial environmental factors (Yin et al., Reference Yin, Guven and Dietis2016). The learned helplessness paradigms, initially developed by Seligman and Overmier (Overmier and Seligman, Reference Overmier and Seligman1967), derived from a cognitive view of depression in which the behavioural condition is induced through the application of uncontrollable and unpredictable aversive stimuli leading to feelings of anxiety and helplessness. This model also has a genetic component since stress-evoked or genetically induced reductions of brain-derived neurotrophic factor (BDNF) increase learned helplessness (Vollmayr and Gass, Reference Vollmayr and Gass2013). The chronic mild stress model was first proposed by Katz et al. (Reference Katz, Roth and Schmaltz1981) and developed further by Willner (Reference Willner1997) focusing on relatively minor and unanticipated irritations of everyday life has been shown to increase depression-like behaviours and reduce hippocampal volume (Andrus et al., Reference Andrus, Blizinsky, Vedell, Dennis, Shukla, Schaffer, Radulovic, Churchill and Redei2012). It is important to note that it induced incoordination in prelimbic cortical GABAergic and glutamatergic neurons, which is dependent on their genetic background and maybe the pathological basis for depressive mood (Xu et al., Reference Xu, Cui and Wang2016). In addition to animal stress models, recent human stress studies hypothesise that activations of the sympathetic division of the autonomic nervous system and pathological alterations in the stress-responsive hypothalamic-pituitary-adrenal (HPA) axis relate to the aetiology of depression through the activation of neural and neuroendocrine cascades of molecular events responding to stress (Tafet and Nemeroff, Reference Tafet and Nemeroff2016). If such stress response continues in a prolonged and excessive manner it can turn maladaptive and contribute to the development of disease, such as depression, particularly in individuals with heightened genetic vulnerability (Tsigos et al., Reference Tsigos, Kyrou, Kassi and Chrousos2016). The presence of these genetic variations appears to be involved in the development of depression in response to stressful events, including adverse experiences during childhood and environmental stressors during adulthood (Tafet and Nemeroff, Reference Tafet and Nemeroff2016).
Strengths and limitations
The present study has originality in utilising and quantifying different measurements of psychosocial stressors across the lifespan while adjusting for the polygenetic risk factors and a wide range of psychosocial covariates. This is the first longitudinal study testing three different operationalisations of lifetime psychosocial stressors–specific stressors, cumulative stress index and stressors clusters–and their associations with depression.
Nevertheless, several limitations are to be noted. First, stressors were self-reported. Measurements of stressors are subject to information bias. Second, the Cronbach's alpha value of stressful life events was 0.58. This suggests that the items of stressful life events had relatively low internal consistency. Future research with the improved internal consistency of this assessment is needed. Third, stress has multiple aspects, including frequency, duration and severity. These aspects of stress collectively influence the aetiological trajectory of depression (Musliner et al., Reference Musliner, Seifuddin, Judy, Pirooznia, Goes and Zandi2015). However, we did not have information on frequency, duration, or severity. Lastly, this present study focused on the role of lifetime stressors in depression while taking into account genetic predispositions. The dynamic interplay between stressors and genetic predispositions was not analysed in this study.
Conclusions
Overall, the present study observed significant individual effects of specific stressors as well as the cumulative effects of psychosocial stressors across the lifespan on the subsequent depression. These effects persisted even after controlling genetic predispositions and sociodemographic characteristics. Exposures to these stressors predicted an elevated risk of subsequent depression. The current study adds to the stress theories about different operationalisations of lifetime stressors predicting different risks of subsequent depression. This is true for both specific and cumulative lifetime stressors. Future research articulating the roles of multiple aspects of stressors and depression is warranted. Future research could also further investigate the underlying neurobiological mechanisms linking stressors and depression. From a prevention perspective, our study underscores that early identification of stressors (including specific and cumulative stressors) could better direct effective prevention and intervention strategies focusing on minimising the negative consequences of stressors, reducing the onset of stressors and providing necessary support for those with various kinds of lifetime stressors to better cope with the stressful experiences.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S2045796021000779.
Acknowledgements
The authors would like to thank the participants, researchers and interviewers in the ZEPSOM study. Dr Su would like to acknowledge the support of a Chinese Council Doctoral Scholarship. Dr Meng also acknowledges the support of a career scholar award from the Fonds de recherche du Québec-Sante, Canada.
Financial support
This work was supported by the Canadian Institute of Health Research (CTP-79839; PJT-148845); and the Canada First Research Excellence Fund provided to McGill University for Healthy Brains for Healthy Lives. These funders had no role in study design, data collection and analysis, decision to publish.
Conflicts of interest
None declared.
Ethical standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
Availability of data and materials
The ZEPSOM data is not currently freely available to researchers in general due to ethical and data management requirements. Interested researchers can directly contact the Research Team at: Zepsom.Coordo@douglas.mcgill.ca








