Need for improved maternal nutrition for successful pregnancy outcome
Neonatal mortality rate in Africa is 42 %( 1 ). This is unacceptably high. Pregnancy outcomes rank among the pressing reproductive health problems in the world. Globally, an annual estimate of 600 000 women aged 15–49 die of pregnancy related causes, with 99 % coming from the developing world( 1 – Reference Addai 3 ) and Nigeria alone accounting for 10 % of this total( Reference Okolocha, Chiwuzie and Braimoh 4 ). The status of maternal and fetal mortality may be threatening and calls for serious attention. In some antenatal clinics, the focus is on check-ups and laboratory investigations whereas nutrition education, a key component of antenatal care still remains a neglected area. Nigeria has an extremely high maternal mortality rate with a ratio of 704 per 100 000 live births implying that with about 24 million live births annually, an alarming record of 170 000 Nigerian women die as a result of complications associated with pregnancy and childbirth. The maternal mortality ratio is about a hundred times worse than that in industrialised countries highlighting the widest disparities in international public health( 5 ).
Role of nutrition in pregnancy
Women's nutrition, before and during pregnancy, may play a key role in reproductive health and is recognised as being important for optimising pregnancy outcomes( Reference Chavarro, Rich-Edwards and Rosner 6 ). The availability and supply of nutrients to the developing foetus depends on maternal nutritional status which in turn depends on her nutrient stores, dietary intake and obligatory requirements. Most of the studies that have examined the importance of nutrition during pregnancy typically focus on the second and/or the third trimester by which time key processes such as organogenesis have been completed( Reference Cetin, Berti and Calabrese 7 ). Women's nutritional status just before conception and/or during early pregnancy (<12 weeks gestation), when women are typically unaware of their pregnancy status, may influence pregnancy outcomes by affecting critical developmental processes that begin early in pregnancy as well as the availability of nutrients. Animal studies suggest that periconceptional undernutrition may influence the hypothalamic–pituitary–adrenal axis which in turn influences outcomes such as pre-eclampsia and preterm delivery( Reference Bloomfield, Oliver and Hawkins 8 ). Ensuring an adequate supply of nutrients to the foetus throughout gestation also depends on placental function which is determined in early pregnancy and may be influenced by maternal nutrition during early pregnancy( Reference Cetin and Alvino 9 ). Maternal endocrine and metabolic responses that occur early in pregnancy in turn influence the supply and utilisation of available nutrients for the rapidly growing foetus later in pregnancy( Reference King 10 ). Maternal nutritional interventions have been shown to be efficacious in improving birth outcomes in low- and middle-income populations. Most of the evidence on efficacy is derived from experimental studies in relatively small populations, in which interventions are delivered under optimal, or at least ‘best practice’ conditions( Reference Victora, Habicht and Bryce 11 ). It is also important to demonstrate that interventions can be implemented successfully under routine conditions in large populations and thus achieve an impact on health and nutrition.
Some of the health problems that could be avoided by having adequate nutrition before, during and between pregnancies include: risk of fetal and infant mortality, intra-uterine growth retardation, low birth weight and premature births, decreased birth defects, cretinism, poor brain development and risk of infection. Successful pregnancy outcome results in well-developed babies that can actualise their potentials and make meaningful contribution to development. The babies would have solid foundation to come out of the intergenerational cycle of malnutrition (Fig. 1).

Fig. 1. (Colour online) Intergenerational cycle of malnutrition.
Strategies to improve maternal nutrition for better pregnancy outcome prior to pregnancy
Adequate nutrition for a woman throughout life cycle
Adequate nutrition to prevent stunting and promote proper growth of the mother to be from conception through infancy to adulthood is important. This is because stunted growth could result in a small pelvis to cause obstructed labour and possible death of the foetus. Undernutrition of future mothers during their growth and development is one factor influencing the reproductive life of women. One mechanism through which undernutrition acts is by delaying the age at which menstruation starts (menarche). For example, there is evidence that undernourished girls are older when menstruation starts but are of similar skeletal maturation compared with well-nourished girls( Reference Prentice 12 ). Kelly et al.( Reference Kelly, Kevany and de Onis 13 ) succinctly reviews the evidence for a nutritional effect on menarche. It is still unknown whether delayed menarche constitutes a relative advantage for an undernourished group, because it allows time to attain a greater pelvic size, as seems to be the case for young well-nourished women whose menarche occurs later. However, if chronic undernutrition delays pelvic growth as it delays menarche, any relative advantage of late maturation could be lost. Moreover, even if delayed maturation results in larger pelvic size at menarche( Reference Rasmussen and Yaktine 14 ), there still may be other negative effects of poor nutrition on reproductive performance and maternal nutritional status, especially if pregnancy follows menarche promptly.
Recent reports based on data from industrialised countries suggest that menarche is delayed or amenorrhoea may ensue when women, especially lean women, engage in heavy physical exercise( Reference Rasmussen and Yaktine 14 ). Whether strenuous physical activity among young women in marginally nourished agricultural populations potentiates a delay in menarche is still unknown. Although undernutrition may increase the age at which the birth canal reaches adult size, there is no conclusive evidence that undernutrition specifically alters pelvic growth except in cases of severe rickets occurring during childhood and of osteomalacia. However, perinatal complications are more common among populations where nutrition problems exist, particularly if prenatal care is poor( Reference Ramakrishnan, Manjrekar and Rivera 15 ). The contribution of cephalopelvic disproportion to these complications is still unclear, as is the contribution of nutrition to pelvic growth. It is believed by a number of obstetricians practicing in developing countries that small pelvic size is a major cause of difficult labours and deliveries (Naeye, personal communication) but, again, conclusive evidence does not exist.
Chronic undernutrition resulting in maternal stunting, or acute or chronic undernutrition resulting in low prepregnancy weight, may also negatively affect reproductive performance as reflected in reduced newborn size and its attendant risks of mortality and morbidity. A positive association between maternal size (height and weight) and newborn size is widely recognised( Reference Ramakrishnan, Manjrekar and Rivera 15 ). The relationship between height and pregnancy outcome is confounded by the fact that maternal height reflects environmental, early nutritional and genetic influences. The influence of height is also confounded because, although height appears to have an independent effect on birth weight( Reference Ramakrishnan, Manjrekar and Rivera 15 ), evidence from industrialised countries suggests that prepregnancy weight or pregnancy weight gain have a larger effect on birth weight than does height( Reference Mangham and Hanson 16 ). Han et al.( Reference Smith, Pell and Dobbie 17 ) in another study from industrialised countries, where women were on average taller and had better childhood nutritional status than is commonly found in developing countries did multivariate analyses of data from a longitudinal study in Guatemala on the effect of supplementation on birth weight. The study suggested that the independent contribution of height to birth weight is statistically significant (P < 0·05). This effect is as large as the effects of maternal weight and caloric intake from supplementation during pregnancy. In addition, the reason for the result could be because the women studied came from villages where childhood growth, especially in height, is affected by differences in nutrition; the authors assume that the adult height of the women studied was determined in large part by their childhood nutrition. Thus, these findings suggest that, at least in this population, the mother's nutritional status during childhood and immediately preceding pregnancy is as important a determinant of birth weight as is maternal nutrition during pregnancy.
Adequate nutrition for women who intend to become pregnant
Nutritional needs differ across various age groups and with certain health conditions. Pregnancy is one such instance in which nutritional needs differ. Women who intend to become pregnant should have adequate supply of proteins, vitamins and minerals before and between pregnancies. This is to ensure that the woman is in a state of good nutritional status to provide all the nutrients required for the rapid increase in cell number and development of the zygote within the first few weeks. Deficiencies of some micronutrients like folic acid, iron and iodine affect the foetus shortly after conception. By the time the pregnancy is detected, permanent damage is done.
Maternal nutrition for successful pregnancy outcome cannot be addressed during pregnancy alone. Varied diet rich in protein sources, fruit and vegetables should be consumed by women who intend to become pregnant.
Strategies to improve maternal nutrition for better pregnancy outcome during pregnancy
Varied diet for pregnant women
Pregnant women should consume varied diets with adequate supply of all the nutrients to meet the needs of the growing foetus e.g. foods rich in protein, iron, iodine, vitamin A, folic acid, zinc and calcium.
Increase nutrient supply for pregnant women
The demand for both energy and nutrients is increased during pregnancy( Reference Han, Mulla and Beyene 18 ). For well-nourished women, only a small amount of additional energy is required because the body adapts to the increased energy requirements and becomes more energy efficient through reduced physical activity and a lowered metabolic rate. Although the average-sized, well-nourished woman requires about 10460 kJ/d (2000 kcal/d) during the last trimester of pregnancy( Reference Picciano, Ziegler and Filer 19 ), many women in developing countries restrict their food intake during pregnancy to have smaller infants, on the premise that smaller infants will carry a lower risk of delivery complications( Reference Hytten, Campbell and Gillmer 20 ). Recent evidence suggests, however, that infants who are small or disproportionate at birth have increased health risks later in life( Reference Brems and Berg 21 – Reference Barker 23 ). The hypothesis is that such infants have had to adapt to a limited supply of nutrients and that in doing so their physiology and metabolism are permanently changed, although the rationale for this hypothesis has been challenged( Reference Barker 24 ).
Requirements for many, but not all, micronutrients increase during pregnancy. Deficiencies can exist because of losses or mal-absorption associated with disease or inadequate intakes, lack of knowledge about adequate prenatal nutrition, or dietary taboos associated with pregnancy( Reference Susser and Levin 25 ), with potential adverse consequences for both mothers and newborn infants. Rush( Reference Gittelsohn, Thapa and Landman 26 ) notes that anaemia in pregnancy and pregnancy-induced hypertension are common and thought to contribute significantly to maternal mortality and morbidity in developing countries. Maine( Reference Rush 27 ) however, shows there is little evidence that nutrition plays a role in pregnancy-induced hypertension.
As a component of prenatal care, micronutrient supplementation might reduce maternal morbidity and mortality directly by treating a pregnancy-related illness or indirectly by lowering the risk of complications at delivery. Nevertheless, the effectiveness of supplementation programmes, notably of iron and folate, has tended to focus on infant outcomes, perinatal mortality, preterm delivery and low birth weight( Reference Maine 28 ). When infant outcomes are discussed, however, a distinction needs to be made between the teratogenic effects of deficiency at periconception and deficiency in later pregnancy. The former includes folate deficiency resulting in fetal neural tube defects( Reference Rooney 29 ) and iodine deficiency that causes cretinism( Reference Kirke, Daly and Molloy 30 ), whereas the latter includes intra-uterine growth retardation( Reference Delange 31 , Reference Gulmezoglu, de Onis and Villar 32 ) and other pregnancy-related and delivery complications( Reference Scholl and Hediger 33 , Reference Kiiholma, Paul and Pakarinem 34 ). This distinction is important because many pregnancies in developing countries are unplanned; the use of prenatal care services, in which iron or iron and folate supplements are generally provided or prescribed, is less than optimal( Reference Hibbard 35 ); and the cost-effectiveness of the programmes promoted needs to be considered. In developed countries, prenatal care providers have reservations about the widespread and indiscriminate use of prophylactic minerals and vitamins because of unproven benefits in well-nourished populations, risks of teratogenicity and side effects( Reference Bothwell 36 ). These concerns need to be considered in the context of developing countries.
Data on vitamin and mineral metabolism and requirements during pregnancy are scanty, and determining the consequences of apparently deficient or excessive intakes is not easy( Reference Cetin, Berti and Calabrese 7 ). In pregnancy, maternal metabolism is altered by hormones that mediate the redirecting of nutrients to the placenta and mammary gland as well as the transfer of nutrients to the developing infant. Kidney function changes to handle the clearance of both fetal and maternal metabolic waste, which is associated with increased urinary excretion of water-soluble vitamins (e.g. folate)( Reference Cetin and Alvino 9 ). Blood volume and composition also change; by the third trimester, blood volume increases by 35–40 % over the non-pregnant state, largely because of a 45–50 % expansion of plasma volume and a 15–20 % expansion of erythrocytes mass.
Nutrient requirements during pregnancy are usually calculated by adding an increment to the value for non-pregnant and non-lactating women that covers the cost of fetal growth and development and the associated changes in maternal tissue metabolism. This factorial approach, however, may not necessarily be correct because it does not take into account metabolic changes in absorption or excretion that may compensate for the additional nutrient requirements without the need for an increase in intake.
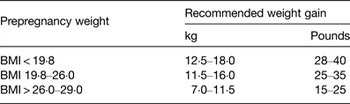
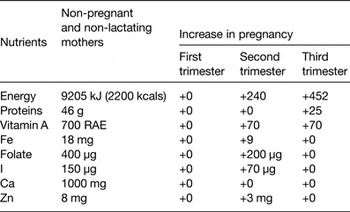
Pregnant women should have increased supply of nutrients to meet the increasing need for energy and nutrients as a result of the developing and growing foetus. An average pregnancy has an estimated energy requirement of approximately 1464–1867 kJ (350–450 kcals) as shown in Tables 1 and 2. This is required during the second and third trimester with the greater amount needed in the third trimester. Adequate energy intake is easy to achieve and can be assessed by appropriate weight gain throughout the pregnancy.
The food guide pyramid could be helpful in planning a diet for the pregnant woman. A trained nutritionist dietician could help plan the diet to ensure adequate intake of all the nutrients. (1) Pregnant women should strongly be encouraged to take their routine pregnancy drugs to help meet the requirements of some nutrients whose intake are difficult to get from food sources. Such routine drugs include micronutrient supplements, iron-folate supplements and calcium supplements. (2) If fortified foods are available, they should form part of the diet of pregnant women e.g. iodised salt to meet iodine requirements and other fortified food in adequate amount. (3) Nutrition education by trained nutritionist on care and adequate diet during pregnancy should be an important aspect of Mother and Child Health Clinics. Mothers should be educated on the importance and sources of nutrients for improved pregnancy outcome.
Conclusion
Maternal nutrition plays a crucial role in influencing fetal growth and birth outcomes. It is a modifiable risk factor of public health importance in the effort to prevent adverse birth outcomes, particularly among developing/low-income populations. It was possible to learn that almost all available studies of randomised control trials and other observational studies conducted in various parts of the world revealed that it is beneficial for the mother to be in a state of adequate nutrition before and during pregnancy for improved pregnancy outcome. Nutrition education should be provided using every opportunity for mothers, fathers, older women and children so that they would be advocates of good nutrition for pregnant women.
Acknowledgements
The author thanks the organisers of the ANEC VI conference for the opportunity to present this paper.
Financial Support
None.
Conflicts of Interest
None.
Authorship
The author had sole responsibility for all aspects of preparation of the paper.