Women, especially pregnant and lactating women, infants and young children are among the most nutritionally-vulnerable groups. Their nutritional vulnerability stems from their physiologically-higher nutrient requirements, which are often not met(Reference Daelmans and Saadeh1, Reference Prentice2). Pregnancy and lactation places additional demands on women. Similarly, for infants rapid growth and development results in an increase in nutrient requirements(Reference Dewey3).
For women and children in Sub-Saharan Africa the environmental and economic conditions place an extra burden on their nutritional status(Reference Prentice2). Pervasive poverty affects the quality of the diet(4). The heavy workload of women increases their nutritional requirements(Reference Prentice, Whitehead, Watkinson, Lamb and Cole5). Frequent and short reproductive cycles often leave the African woman moving from one pregnancy to the next without adequately repleting body nutrient stores(Reference Linkages6). Infants and young children suffer frequent infections and have poor-quality diets(Reference Onofiok and Nnanyelugo7). These factors create an ideal environment for malnutrition to thrive. Malnutrition further predisposes African women and children to morbidity and mortality.
The objective of the present paper is to discuss the nutritional challenges faced by women and children in Sub-Saharan Africa and to highlight successful interventions to address these challenges.
Issues of maternal nutrition
The consequences of maternal malnutrition have both short- and long-term implications for the mother and her offspring.
Fig. 1 summarises the nutritional factors that often result in maternal malnutrition and the consequences for the mother and infant. The widespread malnutrition among African women is manifested by the low maternal BMI (<18·5 kg/m2) for ⩽20% of African women of reproductive age(Reference Linkages6). Consequently, maternal pregnancy weight gain is low(Reference Linkages6).
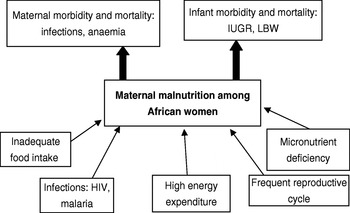
Fig. 1. Effect of maternal malnutrition on maternal and infant health. IGUR, intrauterine growth restriction; LBW, low birth weight.
Inadequate pregnancy weight gain is reflected in the high prevalence of low birth weight among 14% of infants in Sub-Saharan Africa(8). Although pregnancy is considered a normal physiological event in the life cycle, for most African women it is a life-threatening situation(Reference Abdoulae9). The probability of dying from pregnancy-related causes is one in sixteen for Sub-Saharan Africa compared with one in 4000 for industrialised countries(8). About 40% of women aged 20–24 years in Sub-Saharan Africa marry early (at <18 years of age)(8). With many years of child bearing ahead, pregnancies occur frequently and at short intervals, giving the mother insufficient time to replenish her nutrient stores before the next pregnancy(Reference Linkages6). The poor quality of the diet contributes to the widespread energy and micronutrient deficiencies(Reference Prentice, Whitehead, Watkinson, Lamb and Cole5).
HIV infection has worsened the nutritional profile of African women. About 13·1 million African women aged 15–49 years live with HIV/AIDS(8), which coupled with poor nutritional status quickly precipitates maternal malnutrition(Reference Linkages6). Maternal malnutritional status during pregnancy sets the stage for poor pregnancy outcomes, affecting the survival and quality of life for the offspring(Reference Shrimpton10).
Issues for infant and young children
For the developing fetus, its first battle is to survive the intrauterine environment(11). For those who survive there are several challenges that must be surmounted postnatally. The battle to survive through the first year of life is a tough one for the African child. Indeed, global statistics indicate that the infant mortality of 102 per 1000 live births for Sub-Saharan Africa(8) is the highest for all regions. Early childhood malnutrition most probably accounts for the high prevalence of stunting (38%) and underweight (28%) reported for children <5 years of age in Sub-Saharan Africa(8).
Infant feeding practices
Although evidence of the life-saving benefits of exclusive breast-feeding up to 6 months of age is compelling(12), only 30% of children <6 months of age in Sub-Saharan Africa are exclusively breast-fed(8). As a result of suboptimal feeding practices the complementary feeding period presents a great threat to the survival of the African child(Reference Onofiok and Nnanyelugo7). Complementary foods are mainly watery cereal porridges of low energy and nutrient densities(Reference Gibson, Ferguson and Lehrfeld13), and they are often prepared, served and stored under conditions that expose the child to frequent infections(Reference Kimmons, Brown, Lartey, Collision, Mensah and Dewey14).
Older infants and young children are not often given the care and attention needed for the selection of nutritious foods and the encouragement needed to eat foods in sufficient amounts to meet their energy and nutrient requirements(Reference Nti and Lartey15).
The advent of HIV/AIDS has been an obstacle to the efforts to improve child nutritional status(Reference Nduati, John and Mbori–Ngacha16). The feeding of infants and young children whose mothers are infected with HIV continues to be a challenge. Safe infant feeding options are still problematic(Reference Leshabari, Blystad, de Paoli and Moland17).
Interventions to improve maternal and child nutrition
Improving maternal nutritional status
As maternal malnutrition has intergenerational effects, the nutrition of women must be addressed very early in life(Reference Linkages6). Special emphasis must be placed on improving the nutrition of adolescent girls, who are at the dawn of adulthood (taking on reproductive roles). The nutritional demands of pregnancy place adolescent girls at high risk of maternal mortality, pregnancy-related complications and the delivery of low-birth-weight infants(Reference Kurtz, Barua, Khate and Prasad18). Addressing the nutritional needs of adolescent girls prepares them to move into adulthood ready to take on reproductive roles. Women must have an adequate nutritional status before and during pregnancy to provide a good intrauterine environment for the developing fetus(Reference Rush19).
Many countries in Sub-Saharan Africa have instituted supplementary feeding programmes to improve the nutritional status of schoolchildren. The window of opportunity to make a difference for nutrition should start prenatally(20). Thus, supplementary feeding programmes for pregnant and lactating women in countries with high rates of maternal malnutrition should also be considered. Antenatal and postnatal centres provide a captive audience for such programmes. Maternal nutrition education should be a strong component of antenatal and postnatal care and should emphasise the use of fortified staples, animal-source foods, dietary diversification and the use of supplements to improve the quality of diet(Reference Gross21). With this approach, early and regular antenatal attendance would ensure that women would benefit fully from micronutrient supplements and other nutrition interventions.
Mothers should have ready access to skilled medical attendants at delivery. Data from UNICEF indicate that only 42% of births in Sub-Saharan Africa are attended by skilled health personnel(8).
Sustaining exclusive breast-feeding
Promotion of exclusive breast-feeding is ranked as the most effective intervention for reducing the mortality of <5 year-olds(Reference Jones, Steketee and Black22). Access to this knowledge does not necessarily increase exclusive breast-feeding rates. Consistent and concerted efforts are needed to ensure exclusive breast-feeding to 6 months of age. A community-based randomised intervention study in Ghana has assessed the effect of lactation counselling on exclusive-breast-feeding rates among Ghanaian mothers(Reference Aidam, Perez-Escamilla and Lartey23). The results show a 100% increase in exclusive-breast-feeding rates among mothers that received exclusive-breast-feeding support compared with the control group that only received health education information without breast-feeding support. The effectiveness of incorporating breast-feeding counselling within the healthcare system has been well recognised in the WHO–UNICEF Baby Friendly Hospital Initiative(24). However, for sustained impact support must move beyond the hospital environment into the communities where mothers face the biggest challenge to continue with the practice.
Improving complementary feeding practices
Growth faltering is often widespread during the complementary feeding period, an indication of the suboptimal complementary feeding practices(Reference Dewey, Peerson, Heinig, Nommsen, Lonnerdal, Lopez de Romana, de Kanashiro, Black and Brown25). Considerable global and national efforts and attention have been devoted to breast-feeding promotion to the neglect of complementary feeding practices. As pointed out by Lutter ‘infant and young child nutrition will improve only if improvements in complementary feeding are combined with improvement in breastfeeding, environmental sanitation and health’(Reference Lutter26).
Interventions using local technologies such as roasting, malting, drying, fermentation and grinding to process locally-available ingredients are likely to be more successful(Reference Mensah and Tomkins27). To this end, the uses of multimixes of cereal legumes have been extensively explored and studied(Reference Amuna, Zotor, Chinyanga and Chinyanga28–Reference Lartey, Manu, Brown, Peerson and Dewey30).
Sub-Saharan Africa abounds in a variety of indigenous and traditional foods that can be drawn upon to improve the quality of complementary foods through dietary diversification. However, lack of information on the nutritional composition of local indigenous and traditional foods limits their use(Reference Smith, Eyzaguirre, Matig and Johns31).
Meeting the micronutrient requirements of infant and young children is a challenge, because of their high nutrient requirement and small stomach capacity(Reference Dewey3, Reference Gibson, Ferguson and Lehrfeld13, 32). Fortification of staple foods does not address their micronutrient needs(Reference Dewey3). Direct fortification of commercial complementary foods is more effective(Reference Zlotkin, Christofides, Hyder, Schauer, Tondeur and Sharieff33). However, cost and affordability remain an issue for poor households(Reference Nesamvuni, Vorster, Margetts and Kruger34). Direct addition of micronutrients, as sprinkles powder, crushable nutritabs tablets or nutributter, to home-prepared complementary foods is gaining ground as a useful strategy for improving the micronutrient quality of children's diet(Reference Adu-Afarwuah, Lartey, Brown, Zlotkin, Briend and Dewey35), as it does not require the caregiver to prepare new foods.
Nutrition education
Nutrition education for caregivers on child feeding practices has the potential to improve child nutritional status. Nutrition education that provides simple messages tailored for low-income families has made an impact on caregiver child feeding practices, and subsequently on child growth(Reference Penny, Creed-Kanashiro, Robert, Narro, Caulfield and Black36). Studies using the positive deviant approach have shown that in the midst of poverty good caregiver practices can substantially improve growth for children in both urban(Reference Ruel, Pelletier, Habicht, Mason, Chobokoane and Maruping37) and rural(Reference Nti and Lartey15) settings. Nutrition education must be made an integral part of the health delivery system.
Attempts to improve infant and child nutrition must be linked to regular growth monitoring and intervention. The WHO child growth standards(38) provide the tool to assess and advocate for appropriate infant and young child feeding and good care practices for improved growth.
Conclusions
There are serious issues relating to maternal and child nutrition that often result in unacceptably-high morbidity and mortality rates in Sub-Saharan Africa. The interventions needed to make a difference are known. What is needed is to scale up these successful interventions to levels that would make an impact. A country that seeks to tap the full potential of its human resource cannot afford to neglect the nutrition of its citizens, especially the nutrition of women and children. This process requires resources and commitment. For every child a delay of 1 d in intervening is a missed opportunity to make a difference.



