- CRP
C-reactive protein
- ER
endoplasmic reticulum
- UPR
unfolded protein response
Back in February 2004, the magazine Time dedicated its cover to inflammation and named it ‘The Secret Killer’. The authors aimed at highlighting the importance of inflammation in relation to the modern world's greatest health concerns, i.e. chronic diseases. The article echoed scientific observations linking inflammation to pathologies, such as Alzheimer's disease, heart attacks or cancers(Reference Gorman, Park and Dell1). In the last few years, research keeps confirming how an inappropriate inflammatory response – be it a result of a disproportionate activation, an insufficient resolution, or both – actually plays a crucial role in the onset, progression and severity of many chronic conditions, if not all of them.
Obesity is one of the most prevalent non-communicable diseases and a major concern for public health worldwide, mainly due to its well-established relationship with alterations, such as insulin resistance and diabetes, atherosclerosis, hypertension, or some types of cancer, among others. Obesity, like those chronic diseases mentioned earlier, presents an inflammatory component. Indeed, it is now widely agreed that obesity is also a state of low-grade chronic inflammation(Reference Hotamisligil2, Reference Bastard, Maachi and Lagathu3). This relationship was suggested by earlier observations of higher circulating levels of inflammatory proteins in obese individuals, but it is currently believed that inflammation originates locally in adipose tissue as a consequence of excessive fat deposition, and that it later reaches the systemic circulation.
Inflammatory markers in obesity
Altered circulating levels of inflammatory cytokines, such as TNFα, IL-6, or C-reactive protein (CRP), have been reported in overweight and obese adults(Reference Festa, D'Agostino and Williams4–Reference Bulló, García-Lorda and Megias6) (see Table 1), and this event has been linked to the concomitant development of insulin resistance, metabolic disorders and the increased cardiovascular risk seen in obesity(Reference Hotamisligil2). More specifically, measures of body fat have been shown to positively correlate with serum levels of inflammatory proteins, and it is interesting to note that markers of abdominal obesity (e.g. waist circumference) seem to be more strongly associated with inflammatory markers than the BMI or total body fat(Reference Festa, D'Agostino and Williams4, Reference Park, Park and Yu5), which indicates a greater impact of central obesity on inflammation. Furthermore, these relationships have been described for healthy individuals as well. For instance, Hermsdorff et al. analysed the associations between pro-inflammatory markers and proxies for total and central fat, and observed that indices of abdominal fat accumulation (waist circumference and waist:hip ratio) were associated with CRP, complement factor C3, IL-6 and retinol binding protein 4 concentrations, while total body fat percentage was correlated only with IL-6(Reference Hermsdorff, Zulet and Puchau7). Similarly, Lapice et al. showed a positive association between CRP and abdominal fat in healthy non-obese subjects(Reference Lapice, Maione and Patti8). These observations are in agreement with the more detrimental nature attributed to visceral adipose tissue over subcutaneous adipose tissue on the health disturbances associated with obesity(Reference Bastard, Maachi and Lagathu3, Reference Wajchenberg9), as will be briefly discussed at the end of the review.
Table 1. Summary of the inflammatory and immune changes seen in obesity
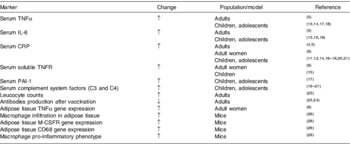
CRP, C-reactive protein; M-CSFR, macrophage colony stimulatory factor receptor; PAI-1, plasminogen activator inhibitor 1; TNFR, TNF receptor.
Is this chronic inflammation a consequence of advancing age?
Actually, it is not. Although it is true that inflammatory processes and inflammation-related diseases are more prevalent in older individuals, special attention must be paid to the fact that these relationships do not occur only in adults, but instead they are also being observed in adolescents and children. More and more frequently, children are being identified with obesity-associated metabolic problems, previously described only in adults(Reference Wärnberg, Nova and Romeo10). In the last few years, large-scale population-based studies have reported significant associations for CRP, a very sensitive marker of inflammation, and proxies for body fat (i.e. BMI and skin-fold thickness) in apparently healthy children and adolescents(Reference Quijada, Paoli and Zerpa11). In overweight pediatric populations, higher circulating levels have been found for several inflammation-related proteins, such as CRP, IL-6, or TNFα(Reference Weiss, Dziura and Burgert12–Reference Gøbel, Jensen and Frøkiaer18) (Table 1). Other inflammatory markers less extensively studied appear to be related to obesity as well. Results from our own group following the AVENA (in Spanish, ‘Food and Nutritional Assessment in Adolescents’) study showed associations between measures of body fat and the complement system factors C3 and C4(Reference Wärnberg, Nova and Moreno19). Moreover, C3 was also shown to be associated with waist circumference, independently of total body fat. In this same study, ceruloplasmin levels correlated with total body fat, although only in girls(Reference Wärnberg, Nova and Moreno19). These observations were reproduced in the most recent AFINOS (Physical Activity as a Preventive Agent of the Development of Overweight/Obesity, Infections, Allergies and Factors of Cardiovascular Risk in Adolescents) study, in which CRP, C3 and C4 were again positively associated with total body fat(Reference Martínez-Gómez, Eisenmann and Wärnberg20). In the European Youth Heart Study, similar results were obtained in younger children for CRP, C3 and body fat(Reference Ruiz, Ortega and Warnberg21).
Lifestyle-aimed interventions seem to be useful to improve the inflammatory condition. Environmental factors, for example physical activity, may counteract the consequences of excessive body fat. Indeed, the AFINOS study revealed that serum levels of CRP, C3 and C4 were not only positively associated with body fat but also inversely associated with cardio-respiratory fitness(Reference Martínez-Gómez, Eisenmann and Wärnberg20). In line with this, our group participated in the design and implementation of an intervention programme for overweight and obese adolescents, with the aim to promote a healthy lifestyle to help lose weight, the EVASYON (Integral Education on Nutrition and Physical Activity for Overweight/Obese Adolescents) study. This programme resulted in decreased serum levels of leptin and other inflammation-related proteins (IL-8, IL-10 and TNFα), without affecting those of adiponectin, and changes seemed to depend on the degree of physical activity and fitness(Reference Romeo, Martínez-Gómez and Díaz22).
Obesity: an immune disease?
The interactions between nutrition and nutritional status and the immune function have been the object of research for some time now, and it is known that undernutrition, or more generally, malnutrition, leads to defective immune function and impaired immunocompetence, so that the body is more vulnerable to illness and infections. Obesity, which is a state of malnutrition by excess, has been related to immune dysfunction as well, after observations of higher rates of infections and impaired wound healing in obese subjects(Reference Martí, Marcos and Martínez23). Excess body fat is accompanied by changes in leucocyte counts, with elevated leucocyte, neutrophil, monocyte and lymphocyte counts, but lower T- and B-cell mitogen-induced proliferation(Reference Martí, Marcos and Martínez23). In addition, other studies have shown that the production of antibodies after vaccination is diminished in obese patients(Reference Martí, Marcos and Martínez23, Reference Sheridan, Paich and Handy24). Even in children evidence was obtained of impaired cell-mediated immune responses with obesity(Reference Martí, Marcos and Martínez23). Considering all this, it seems clear that obesity, like other situations of malnutrition, impairs immune function.
Could it be also said that an altered immune system underlies the onset of obesity? This affirmation would be perhaps too speculative or not sufficiently founded at the moment, but what does seem plausible is that, at least, immune system dysfunction is a major contributor to the development of obesity-associated alterations, especially to inflammation and insulin resistance.
But how is obesity linked with the immune system?
The link seems to be adipose tissue itself. There are several connections indeed between adipose tissue and the immune system. For a start, macrophages and lymphocytes can be normally found in the non-adipose fraction of the tissue(Reference Caspar-Bauguil, Cousin and Galinier25). Moreover, white adipocytes have been suggested to share embryonic origin with immune cells, while characterisation of adipose tissue-resident lymphocytes led to the notion that this tissue was an ancestral immune organ(Reference Caspar-Bauguil, Cousin and Galinier25, Reference Saely, Geiger and Drexel26). And more recently, immature haematopoietic cells have been found in adipose tissue, hence it has been proposed as a site for formation and maturation of immune cell precursors(Reference Poglio, de Toni-Costes and Arnaud27).
In the early 2000s, histological studies in mice showed that macrophage infiltration in adipose tissue was greater in obese than in lean animals(Reference Weisberg, McCann and Desai28). The macrophages appeared as crown-shaped aggregates, similar to those observed in other known inflammatory conditions, such as rheumatoid arthritis, and grew larger with increasing degrees of obesity. This finding led to the idea that macrophage aggregates could partially explain the obesity-related inflammatory state(Reference Weisberg, McCann and Desai28). In support of this hypothesis, two different phenotypes for adipose tissue-resident macrophages were later described: one that acts as pro-inflammatory (known as M1 or ‘classically activated’), and another that acts as anti-inflammatory (M2 or ‘alternatively activated’). Interestingly, obesity has been associated with a switch from the M2 to the M1 phenotype; that is, to a more pro-inflammatory profile(Reference Lumeng, Bodzin and Saltiel29). Furthermore, the absence of the M2 phenotype has been associated with a higher susceptibility to obesity, inflammation and insulin resistance(Reference Odegaard, Ricardo-González and Goforth30).
The enhanced macrophage infiltration in the obese adipose tissue explains in part, but not completely, the increased production of cytokines and chemokines. These molecules are mainly produced by immune cells, e.g. monocytes, macrophages and T-lymphocytes, and also by other cells such as mast cells, fibroblasts, endothelial cells, neurons, or adipocytes themselves. Fat cells secrete, among others, TNFα, IL-6, monocyte chemotactic protein 1, transforming growth factor β, or acute phase proteins(Reference Trayhurn and Wood31). Consequently, alteration of adipocyte function plays a crucial role in the development of obesity-associated inflammation.
Why does an inflammatory response initiate in the adipose tissue?
This is still a complicated question to address. Cytokines are chemical messengers that are released to regulate gene expression in a specific organ or cell type, and which interact in a complex way, mutually inducing or inhibiting their production and effects. What is the purpose or usefulness of the enhanced cytokine production in obesity? We can only speculate in this respect so far, but the answers can be searched in the enlarged, lipid-loaded adipocyte. In a situation of excessive nutrient inflow and storage, there must be mechanisms operating within and from the cell in order to maintain or restore energy homoeostasis. Certain cytokines, e.g. IL-6 and TNFα, are known to induce insulin resistance(Reference Hotamisligil2, Reference Bastard, Maachi and Lagathu3), so their local production could constitute a regulatory mechanism to stop the hypertrophied adipocyte from storing lipids. Or, macrophage infiltration in response to adipocyte-derived chemokines, such as monocyte chemotactic protein 1 or macrophage migration inhibitory factor, may respond to the need for clearing the adipose tissue of dysfunctional and necrotic fat cells, such as phagocytes normally do, for instance, during an acute inflammatory response in the context of an infection. The problem arises when, as a result of sustained obesity, the inflammatory response does not achieve its goal and it is not resolved, thus turning from a local reaction to a systemic chronic state.
How does this response start? What is the trigger for the initial inflammatory signal?
The mechanisms linking obesity and chronic low-grade systemic inflammation are yet not entirely understood, but different plausible explanations have been proposed. They will be now commented on briefly in an attempt to offer a clear and likely picture of the situation. It is important, however, to keep in mind that these processes are not mutually exclusive, but instead they might all operate in an orchestrated synergistic fashion (see Fig. 1).

Fig. 1. Diagram of the proposed relationships between adipocytes and macrophages in the context of inflammation and immune alterations in obesity. The hypertrophied adipocyte presents altered secretion of adipokines, cytokines and fatty acids. This affects macrophage activity, with further release of pro-inflammatory cytokines and a stimulatory effect on adipocyte lipolysis. In addition, the adipocyte experiences hypoxia and cellular stress, exacerbating the local inflammatory response and leading to adipocyte dysfunction and metabolic alterations, especially insulin resistance. Solid arrows indicate production and release of molecules; dashed arrows indicate stimulatory events. ER, endoplasmic reticulum; PPAR, peroxisome proliferator activated receptors; TLR, Toll-like receptors.
The mechanisms for adipose tissue inflammation: all roads lead to Rome
Adipokines modulate the production and release of inflammatory cytokines
Adipose tissue in general and adipocytes in particular secrete a great number of bioactive molecules of different nature, collectively termed adipokines, many of which have immuno-modulatory actions(Reference Trayhurn and Wood31). This is the case for leptin and adiponectin, to mention only the two most paradigmatic adipokines.
Leptin, the first adipokine to be discovered, regulates immune function on various levels: stimulating monocyte proliferation and differentiation into macrophages, modulating the activation of natural killer lymphocytes, or inducing the production of pro-inflammatory cytokines such as TNFα, IL-6, or IL-12(Reference Martí, Marcos and Martínez23, Reference Tilg and Moschen32). In animal models, the absence of leptin or leptin action has been associated with defective immune function. For instance, ob/ob mice, which are leptin-deficient, present lymphoid organ atrophy, reduced thymus proportion, lower lymphocyte and natural killer cell numbers, decreased cytotoxic activity and lower expression of pro-inflammatory cytokines. These mice as well as the db/db mice (which lack leptin receptors) are less efficient in fighting infections. Zucker rats, which are also leptin receptor-deficient, show lymphopenia and a lower phagocytic capacity(Reference Martí, Marcos and Martínez23). Leptin is a sensor of the state of energy stores in the body, and when these stores enlarge, leptin acts on the central nervous system stimulating satiety and energy expenditure. Therefore, circulating leptin levels increase in parallel with body fat mass. However, it is well known that, in most cases, human obesity is accompanied by a blunt central response to leptin action, and this leads to a situation of leptin resistance and compensatory hyperleptinaemia, with possible consequences on the activation of immune cells.
Adiponectin, an anti-inflammatory and insulin-sensitizing hormone, exerts opposite immune-modulatory actions to leptin. It inhibits the phagocytic activity and the production of TNFα in macrophages, the differentiation of monocyte precursors, the synthesis of endothelial adhesion molecules and the formation of foam cells(Reference Koerner, Kratzsch and Kiess33). In addition, it stimulates the release of anti-inflammatory IL, such as IL-10 or IL-1 receptor agonist(Reference Tilg and Moschen32). And it is known that, unlike those of leptin, adiponectin concentrations correlate inversely with body weight.
Therefore, changes in the levels of the two main adipokines may contribute to the onset and maintenance of the systemic inflammation along with insulin resistance present in obesity.
Fatty acids can induce inflammation
Abnormally elevated blood lipid levels, including NEFA, are a common feature in obesity. There are different explanations for this increase; one is known as the ‘adipose tissue expandability’ hypothesis(Reference Virtue and Vidal-Puig34). According to this hypothesis, the adipose tissue as a whole has limited capacity to expand and to store energy. Exceeding this limit leads to enhanced lipolysis within the adipocyte and the subsequent release of NEFA into the blood stream. NEFA reach other tissues and organs, and exert toxic effects on them, e.g. resistance to insulin action; a phenomenon known as lipotoxicity.
The chemical nature of fatty acids is relevant to triggering the inflammatory response. Studies on weight-discordant twins have shown that obese individuals exhibited signs of insulin resistance and stimulated inflammatory and immune response pathways in adipose tissue when compared to their lean twins. These alterations paralleled considerable differences in adipose tissue fatty acid composition, which resulted in diminished proportions of stearic (18:0), linoleic (18:2n-6) and α-linolenic (18:3n-3) acids, and elevated levels of palmitoleic (16:1n-7) and arachidonic (20:4n-6) acids in obese twins(Reference Pietiläinen, Róg and Seppänen-Laakso35). SFA appear to be especially important in this regard, as they may stimulate TNFα and IL-6 production in adipocytes(Reference Stryjecki and Mutch36). In addition, there seems to be a positive feedback loop involving SFA from adipocytes and cytokines from macrophages: SFA can increase the production of TNFα in macrophages, and in turn the immune cells induce lipolysis in adipocytes (Fig. 1). These events accelerate the inflammatory change in the adipose tissue in obesity(Reference Suganami, Tanimoto-Koyama and Nishida37).
How can fatty acids elicit an inflammatory response? In the first place, they have been suggested to modulate adipokine production and/or secretion. As an example, adiponectin levels have been associated with fatty acids, this correlation being negative with SFA, palmitoleic (16:1n-7) or γ-linolenic (18:3n-6) fatty acids and positive with oleic acid and total n-6 and n-3 PUFA(Reference Fernández-Real, Vendrell and Ricart38, Reference Pérez de Heredia, Sánchez and Priego39).
Alternatively, NEFA may directly induce inflammatory pathways through activation of cell receptors. For instance, they are natural ligands for the PPAR. These transcription factors regulate cell metabolism and adipocyte differentiation, and can also suppress the activity of the NF-κB, another transcription factor crucial in the initiation of the inflammatory response. In addition, PPAR seem to be involved in the aforementioned phenotypic switch of adipose tissue macrophages (from M2 or anti-inflammatory to M1 or pro-inflammatory)(Reference Coll, Barroso and Álvarez-Guardia40). On the other hand, recent evidence has suggested that fatty acids, especially SFA, may also act through binding to Toll-like receptors, the activation of which induces the synthesis of inflammatory markers in macrophages and aggravates insulin resistance(Reference Fessler, Rudel and Brown41) (Fig. 1).
In turn, pro-inflammatory cytokines increase NEFA levels(Reference Grunfeld and Feingold42), and chronic systemic inflammation stimulates lipolysis and decreases lipogenesis in adipose tissue, while having the opposite effects on lipid synthesis in skeletal muscle and liver(Reference Mei, Zhao and Li43), and in consequence the situation is aggravated.
Too many nutrients mean cellular stress
The excessive adipose tissue growth has further consequences at the cellular and subcellular levels, and a role has been suggested for endoplasmic reticulum (ER) stress in the origin of adipocyte dysfunction in obesity(Reference Gregor and Hotamisligil44). Briefly, the ER is a primary site for protein synthesis and TAG droplet formation. Under conditions of cellular stress of various natures, ER function becomes progressively impaired and this triggers a security mechanism known as the ‘unfolded protein response’ (UPR). The UPR is linked to: (1) the production of reactive oxygen species, and therefore greater oxidative stress and (2) the activation of inflammatory pathways, with increased expression of cytokines, such as IL-8, IL-6, monocyte chemotactic protein 1 and TNFα.
The state of nutrient excess and cell expansion in obesity implies a higher demand for protein and TAG droplet formation, and this may as well induce ER stress and the UPR. Additionally, nutrients themselves may serve as signals leading to ER stress. For example, and in relation to the previous section, NEFA have been shown to induce the UPR in various cell types. Paradoxically, glucose deprivation might also contribute to ER stress in obesity; this could happen as a result of insulin resistance eventually developing within the adipose tissue.
Finally, and closing a positive feed-back loop, the inflammatory condition in the obese adipose tissue induces the UPR and enhances ER stress(Reference Gregor and Hotamisligil44).
The obese adipocyte needs oxygen
We have already commented on how the obese adipocyte receives a greater nutrient supply that it transforms into TAG droplets, becoming larger and larger. The capacity of adipose tissue to change its size surpasses that of other organs and tissues. In consequence, adipose tissue expansion in obesity eventually reaches a point where the development of local vasculature is insufficient, and cannot meet the oxygen demands of distant enlarged adipocytes. It was hypothesized that hypoxic adipocytes would then produce inflammatory signals in order to stimulate angiogenesis(Reference Trayhurn and Wood31), and later studies in animal and culture models have confirmed this hypothesis(Reference Trayhurn, Pérez de Heredia, Wang, Clément, Spiegelman and Christen45). The key element in the initiation of the cellular response to hypoxia is the hypoxia-inducible factor 1, a transcription factor highly unstable under normoxic conditions, but which becomes stabilized when oxygen availability is low. Once stabilized, hypoxia-inducible factor 1 regulates the expression of a great number of genes involved in different functions that include angiogenesis, inflammation and energy metabolism. Some of these genes are leptin, plasminogen activator inhibitor 1 or macrophage migration inhibitory factor, all of which become up-regulated, and adiponectin, which becomes down-regulated(Reference Trayhurn, Pérez de Heredia, Wang, Clément, Spiegelman and Christen45).
Hypoxia has important consequences for adipocyte metabolism, as it forces the cell to switch from aerobic to anaerobic glycolysis, in order to obtain energy from glucose. This results in increased production and release of lactate from adipocytes(Reference Pérez de Heredia, Wood and Trayhurn46). Lactate has been shown to stimulate inflammatory pathways in macrophages(Reference Samuvel, Sundararaj and Nareika47) and it also appears to enhance the lipopolysaccharide-induced inflammatory response in pre-adipocytes(Reference Pérez de Heredia, Wood and Trayhurn48).
However, adipocytes are not the only cells responsive to hypoxia within adipose tissue. Resident macrophages tend to accumulate around hypoxic areas, probably recruited by chemotactic signals released from affected adipocytes, and they respond to the lack of oxygen in a similar manner to adipocytes, by producing pro-inflammatory cytokines. Pre-adipocytes are also sensitive to hypoxia, although their response is milder than that of mature adipocytes(Reference Trayhurn, Pérez de Heredia, Wang, Clément, Spiegelman and Christen45).
It is apparent that the hypoxia response fails to achieve the expected effect of increasing adipose tissue vascularization, but instead it leads to a situation of local fibrosis, which contributes to adipose tissue dysfunction(Reference Halberg, Khan and Trujillo49). In line with this, hypoxia has been found to induce the UPR (see earlier) in cultured adipocytes(Reference Gregor and Hotamisligil44).
Visceral fat v. total fat: what difference does it make?
As mentioned earlier in this review, most characteristics of adipose tissue vary according to its anatomical localisation, and these differences render the visceral fat more clinically relevant than the subcutaneous fat, with regard to the development of metabolic disturbances, insulin resistance or cardiovascular risk(Reference Bastard, Maachi and Lagathu3, Reference Wajchenberg9). As far as inflammation is concerned, there are several features that suggest that visceral fat accumulation is again more detrimental than subcutaneous fat. Firstly, infiltration of macrophages in obesity seems to be greater in visceral than in subcutaneous adipose tissue(Reference Cancello, Tordjman and Poitou50). On the contrary, the gene expression of the anti-inflammatory adipokine adiponectin was found to be lower in the visceral than in the subcutaneous depot(Reference Hernández-Morante, Milagro and Gabaldón51). More recently, it has been observed in obese subjects that endothelial cells isolated from visceral fat show a higher expression of genes related to angiogenesis and inflammation than endothelial cells from subcutaneous adipose tissue(Reference Villaret, Galitzky and Decaunes52). In addition, the expression of hypoxia-related genes also seems to be greater in the visceral adipose tissue, although vascularisation is not poorer there when compared with the subcutaneous depot. And finally, the cells from visceral fat show more evident signs of cellular senescence than those from subcutaneous fat(Reference Villaret, Galitzky and Decaunes52).
Conclusions
In summary, inflammation and an altered immune response are important components of obesity and contribute greatly to the development of related metabolic complications, especially of insulin resistance. The explanation lies in the close interrelationship between the adipose tissue and the immune system. As a matter of fact, obesity-associated chronic systemic inflammation has its origin in a dysfunction of the adipose tissue. Various plausible explanations have been proposed for the phenomenon, such as changes in adipokine secretion, fatty acid-induced inflammation, oxidative stress, ER stress, or adipose tissue hypoxia, and they are likely to act in a synergistic manner. However, more research is still needed to understand the precise mechanisms for adipose tissue inflammatory response and how it leads to metabolic alterations.
Acknowledgements
All authors contributed equally to the writing of the first draft and F.P.H. and A.M. structured and compiled the final version. The authors declare no conflicts of interest.




