Ischaemic coronary disease in adults has multiple risk factors, one of which is chronic diabetes mellitus. The exact pathophysiology in patients with diabetes and myocardial ischaemia is unclear, as some have atherosclerotic plaques, while others have coronary microvascular dysfunction in the absence of plaques.Reference Severino, D’Amato and Netti1 While coronary artery disease and myocardial infarctions are well-known complications of chronic diabetes in adults, there are rare reports of myocardial infarcts in patients as young as 12 years during their initial episode of diabetic ketoacidosis.Reference Batra, Acherman, Wong and Silka2 There are also reports of coronary artery spasm in adults in diabetic ketoacidosis, but no reports in children.Reference Ziakas, Basagiannis and Stiliadis3 We present the youngest reported case of coronary artery spasm in an adolescent with a structurally normal heart and diabetes.
Case presentation
A 15-year-old Hispanic male with poorly controlled type 1 diabetes presented to the emergency department in severe diabetic ketoacidosis. He was afebrile, tachycardiac, hypertensive (142/95 mmHg) and tachypneic with Kussmaul breathing. Admission laboratories included: pH 6.94, glucose 482 mg/dl, lactic acidosis and increased anion gap. Haemoglobin A1C was elevated at 14.1%. A 12-lead electrocardiogram was obtained and showed sinus tachycardia with no ST depression or elevation (Fig 1a). He was admitted to the paediatric ICU.
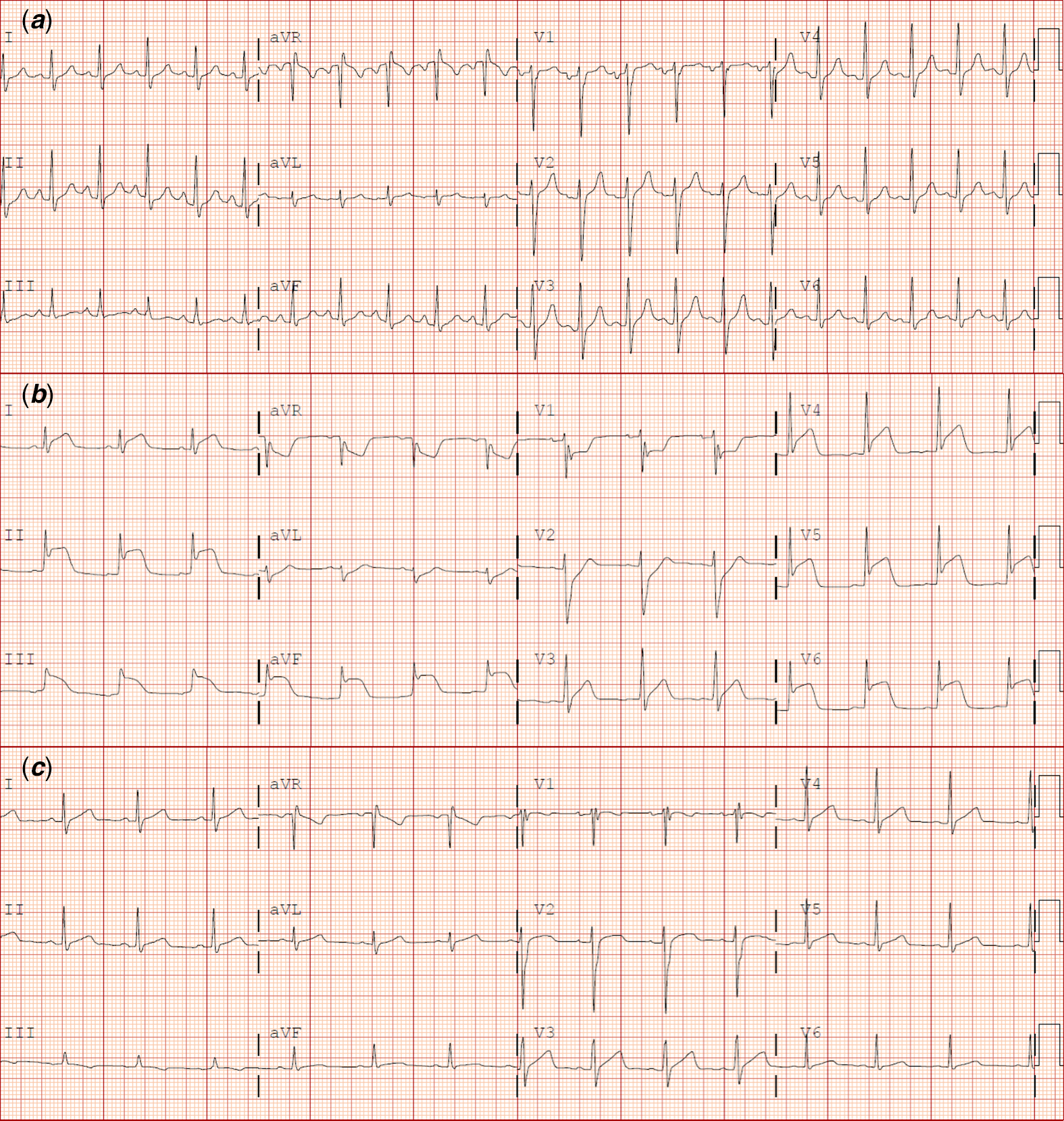
Figure 1. ( a ) Baseline 12-lead electrocardiogram on hospital admission showing sinus tachycardia and no ST changes. ( b ) Twelve-lead electrocardiogram during initial episode of chest pain showing diffuse ST elevations concerning for pericarditis versus myocardial ischaemia. ( c ) Twelve-lead electrocardiogram 2 weeks after hospital discharge showing normal sinus rhythm with complete resolution of ST changes.
Forty-eight hours after admission, the patient removed his telemetry monitor to shower and after replacement 45 minutes later, was noted to have ST elevations. Prior to this change, the monitor had shown normal sinus rhythm. He also reported new focal, pressure-like chest pain. A 12-lead electrocardiogram was obtained and showed diffuse ST elevations (Fig 1b). High-sensitivity troponin was mildly elevated at 504 ng/l (normal <11 ng/l; threshold for catheterisation >2000 ng/l), and he was hypokalaemic (3.0 mmol/l), mildly acidotic (pH 7.23) with improving hyperglycaemia (>200). He remained hemodynamically stable. Serial high-sensitivity troponin and 12-lead electrocardiograms were obtained. After 2 hours, the chest pain resolved without intervention and electrocardiograms showed near-normalisation of the ST elevations. A urine drug screen was negative. Given his stability, an echocardiogram was deferred and he was started on a course of naproxen for presumed pericarditis.
Despite resolution of the chest pain, high-sensitivity troponin continued to increase rapidly, peaking at 2,523 ng/l, at which time he went emergently to the catheterisation laboratory for coronary angiography and possible intervention. Selective coronary angiography revealed angiographically normal coronary arteries with no stenoses (Fig 2). Given the rapid progression of his course, an echocardiogram was not performed until after the catheterisation and revealed normal anatomy, biventricular size and systolic function with no focal wall motion abnormalities and no pericardial effusion.

Figure 2. Selective left ( a and b ) and right ( c ) coronary angiography showing normal coronary arteries with no evidence of stenosis.
Because the troponin leak and electrocardiogram changes were consistent with myopericarditis, he underwent cardiac MRI which showed no oedema, fibrosis or ischaemia. High-sensitivity troponin began to down-trend and was near-normal at discharge. Post-discharge 12-lead electrocardiogram 2 weeks later was normal, interestingly, with no pathologic Q wave changes (Fig 1c).
Discussion
Diabetes mellitus is a known risk factor for coronary artery disease and myocardial infarctions in adults, and rarely children, although those without true myocardial infarctions were attributed to hyperkalaemic coronary artery spasm.Reference Batra, Acherman, Wong and Silka2–Reference Elsayed4 Hyperkalaemia has been reported to cause ST segment elevation that simulates a myocardial infarction and has been deemed a “pseudoinfarction”.Reference Ziakas, Basagiannis and Stiliadis3 It is possible that hyperkalaemia contributes to these electrocardiogram changes by triggering coronary spasm, vasoconstriction of coronary arteries causing total or subtotal occlusion that can cause anginal pain.Reference Ziakas, Basagiannis and Stiliadis3,Reference Elsayed4 While more common in adults with diabetes, myocardial infarction has been reported in children as young as 12 years in diabetic ketoacidosis. Diabetic ketoacidosis is a state of metabolic decompensation and hyperosmolarity. The hyperosmolar state may predispose patients to thromboembolic complications, such as myocardial infarction.Reference Batra, Acherman, Wong and Silka2 In diabetic patients admitted in diabetic ketoacidosis, elevated troponin is a risk for future cardiac events and mortality.Reference Al-Mallah, Zuberi, Arida and Kim5 Although often in a total potassium deficit, patients in diabetic ketoacidosis often have elevated serum potassium levels due to a shift of potassium from the intracellular to extracellular space secondary to acidosis, insulin deficiency and hypertonicity.Reference Elsayed4 In contrast, the diagnosis of coronary artery spasm is suspected in a patient with anginal chest pain without atherosclerotic disease, congenital coronary artery abnormalities, coronary artery bridges, myocarditis, pericarditis or pulmonary or right ventricular abnormalities on echocardiogram or MRI. The present case is unique in that the patient is the youngest reported to suffer coronary arterial spasm associated with diabetic ketoacidosis with mildly low potassium levels and normal coronary angiography.
Conclusion
Thorough evaluation of patients with diabetes mellitus with chest pain is crucial due to the high risk of myocardial infarction in this patient population, even younger patients who would not typically be expected to suffer from coronary disease. While there have been a few reports of coronary arterial spasm in young adults with diabetic ketoacidosis, this diagnosis should be considered in children with diabetic ketoacidosis as well.
Acknowledgements
None.
Financial support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of interest
None.





